Hemichorea Hyperglycaemia Basal Ganglia Syndrome in a Patient with Type 1 Diabetes Mellitus: A Rare Case Report
Swathi Gurursamy1, Kalaimani Sivamani2, Selvaraj Pitchai3, Ameya S Chogle4
1 Postgraduate, Department of Internal Medicine, Mahatma Gandhi Medical College and Research Institute, Pillaiyarkuppam, Puducherry, India.
2 Ex-Assistant Professor, Department of Internal Medicine, Mahatma Gandhi Medical College and Research Institute, Pillaiyarkuppam, Pondicherry, India.
3 Professor, Department of Internal Medicine, Mahatma Gandhi Medical College and Research Institute, Pillaiyarkuppam, Pondicherry, India.
4 Postgraduate, Department of Internal Medicine, Mahatma Gandhi Medical College and Research Institute, Pillaiyarkuppam, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Kalaimani Sivamani, No. 26, Bheeshmar Street, Kennedy Garden, Lawspet, Puducherry-605008, India.
E-mail: kalaimani.sivamani@gmail.com
Hyperglycaemia induced involuntary movements are uncommon in clinical practice though Chorea Hyperglycaemia Basal Ganglia syndrome (CHBG) or Non-ketotic Hyperglycaemic Hemichorea (NHH) is being reported with increasing frequency due to the clinical awareness and widespread availability of neuroimaging. Prompt recognition of CHBG is essential, since correction of hyperglycaemia usually leads to early resolution of the involuntary movements. It is usually seen in elderly patients with uncontrolled Type 2 diabetes mellitus who present acutely with hemichorea or hemiballismus. It is rarely reported in Type 1 diabetes mellitus. Here, the author presents a 25-year-old male patient diagnosed with Type 1 diabetes mellitus with persistent chorea involving the left upper and lower extremity in whom the movement disorder persisted despite correction of hyperglycaemia.
Blood glucose, Dyskinesia, Movement disorders
Case Report
A 25-year-old male, diagnosed with Type 1 diabetes mellitus since 5 years of age, on irregular insulin therapy, presented with involuntary movements of left upper limb and lower limb on and off for the past 4 years. The diagnosis of Type 1 diabetes was based on his age of onset, though serological tests for anti-Glutamic Acid Decarboxylase (GAD) and other autoantibodies were not done.
The involuntary movements started in the left upper limb and left lower limb which were brief and jerky. It was not present during sleep. There was no history of fever, chest pain and joint pain. There was no history of cardiac illness. There was no family history of chorea. Patient was found to have blood sugar levels above 500 mg/dL when the symptoms first started 4 years back though he did not adhere to the prescribed dose of insulin and the involuntary movements continued for the subsequent years before his current presentation.
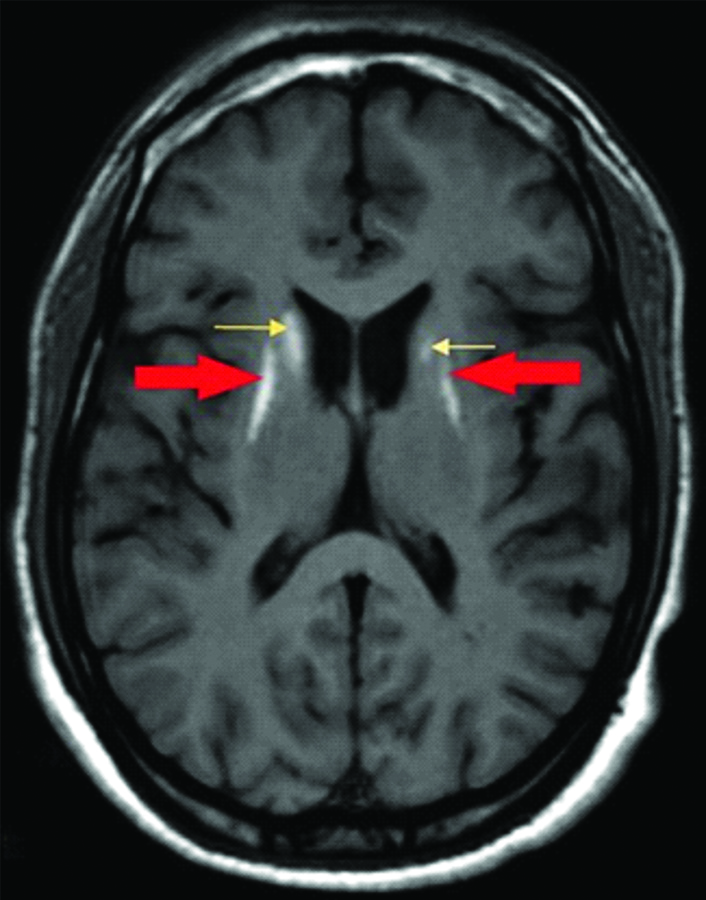
General physical examination revealed diffuse lipomatosis. His vitals were stable. Neurological examination revealed normal higher mental functions, normal tone, power of 5/5 in all 4 limbs and normal deep tendon and superficial reflexes. There were brief involuntary jerky movements involving left upper limb and occasionally in left lower limb. The investigations revealed fasting blood sugar of 600 mg/dL, post-prandial blood sugar of 718 mg/dL, HbA1c of 14.7%, urine ketones were negative. His cardiac, renal and liver parameters were within normal limits. Fundus examination revealed mild nonproliferative diabetic retinopathy in the right eye and slit lamp examination did not reveal any Kayser-Fleischer (KF) ring. A 2D echocardiogram was found to be normal. Antinuclear antibody and Human Immunodeficiency Virus (HIV) tests were negative. His thyroid profile was normal. MRI brain was done which showed bilateral symmetrical hyperintense signals at both globus pallidi and caudate nuclei on T1 weighted imaging [Table/Fig-1] and no restriction on Diffusion Weighted Imaging (DWI). He was admitted for glycaemic control with a diagnosis of hemichorea hyperglycaemia basal ganglia syndrome.
T1 weighed MRI of Brain showing bilateral symmetrical hyperintensities at both globus pallidi (red arrows) and caudate nuclei (yellow arrows).
Blood sugar levels were controlled with biphasic isophane insulin injection (30% regular insulin and 70% isophane), the dose of which was titrated according to blood sugar levels. He was given 25 units of pre-mixed insulin in the morning and 15 units at night and regular monitoring of Capillary Blood Glucose (CBG) pre- and post-meals was done.
After 3 days of admission all his random blood sugar values were below 200 mg/dL. There was a decrease in the frequency of the involuntary movements, but it persisted. Hence, he was started on T. Quetiapine 25 mg HS as advised by neurologist. The patient was followed-up after one month and there was reduction in choreic movements but he reported that it increased whenever he skipped his insulin doses. A repeat MRI was not taken during follow-up as there was no complete resolution of the symptoms.
Discussion
Chorea Hyperglycaemia Basal Ganglia syndrome (CHBG) is a rare condition that occurs in uncontrolled Type 2 diabetes mellitus and characterised by hemichorea/hemiballismus with non-ketotic hyperglycaemia. CHBG is pre-dominantly seen in women especially in Asian women indicating genetic predisposition [1-3]. Only few cases of hyperglycaemia induced chorea have been reported in Type 1 diabetes mellitus with one of the patients having ketotic hyperglycaemia and the remaining having non-ketotic hyperglycaemic chorea [4-9]. The index case had non-ketotic hyperglycaemia.
The exact aetiopathogenesis of CHBG syndrome is incompletely understood, with multiple theories suggesting impaired cerebral autoregulatory mechanism, activation of anerobic metabolism and depletion in the GABAergic neurons and reduction in acetyl choline synthesis leading to dysfunction of the striatum producing the clinical manifestations of this syndrome. Histological findings may suggest neuronal loss/atrophy within corpus striatum [10,11].
Hemichorea is a hyperkinetic movement disorder due to lesions of contralateral striatum [12]. There are various causes like haemorrhagic or ischemic stroke, neoplasm, systemic lupus erythematosus, hyperosmolar hyperglycaemic non-ketotic syndrome, Huntington’s disease, Sydenham’s chorea, HIV, hyperthyroidism, trauma and drug toxicity. CHBG can be seen both in patients with long standing uncontrolled diabetes mellitus as well as the initial manifestation of hyperglycaemia leading to the diagnosis of diabetes mellitus [13-16]. This patient was considered to have CHBG syndrome after excluding other secondary causes of chorea like Wilson’s disease; (Huntington’s disease usually start in the fourth decade), negative family history, there was no recent head injury and patient was not on any antipsychotics or antiepileptics drug. A 2D echocardiography was normal and there was no evidence of rheumatic heart disease. HIV causes chorea by direct effects as well as opportunistic infections like toxoplasmosis involving the basal ganglia [17]. Hyperthyroidism has also been reported to cause chorea probably due to functional alteration in the dopamine turnover in the corpus striatum [18]. HIV serology was negative and thyroid profile was normal in this patient.
The radiological findings in CHBG syndrome include hyperintensities in striatum and globus pallidus in T1 weighed imaging without contrast enhancement. In a report of 20 cases of chorea associated with hyperglycaemia, almost all the patients had striatal abnormalities on neuroimaging which was either contralateral to the hemichorea or bilateral in some cases [16]. The index case had bilateral striatal abnormalities though he had unilateral symptoms. The typical triad of chorea with striatal abnormalities on neuroimaging and hyperglycaemia in a patient with diabetes mellitus clinches the diagnosis of CHBG syndrome, as in this patient.
The treatment of CHBG syndrome or NHH is to achieve optimal glycaemic control with insulin and oral hypoglycaemic drugs. Complete resolution of the movement disorder can occur within 48 hours of glycaemic control, though it may continue for few weeks in many patients [16]. In a case series of 5 adult patients with non-ketotic hyperglycaemia, chorea persisted despite optimal control of blood sugars for more than 6 months during follow-up [19]. In the reported cases of Type 1 diabetes mellitus with chorea, there was complete resolution of the involuntary movements in all cases except one [4-9]. In the index patient the movement disorder persisted for more than 4 years probably due to noncompliance to insulin therapy. In those patients with persistent chorea despite blood sugar control, neuroleptics like haloperidol, benzodiazepines like clonazepam and antiepileptics like sodium valproate have been tried with variable response [9,16,19].
Conclusion(s)
CHBG is a rare complication of non-ketotic hyperglycaemia which has a good prognosis if promptly recognised and optimal glycaemic control is achieved. Clinicians should be aware that this entity can occur in both Type1 and Type 2 diabetes mellitus.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 05, 2020
Manual Googling: Apr 29, 2020
iThenticate Software: Jun 03, 2020 (13%)
[1]. Oh SH, Lee KY, Im JH, Lee MS, Chorea associated with non-ketotic hyperglycaemia and hyperintensity basal ganglia lesion on T1-weighted brain MRI studyJournal of the Neurological Sciences 2002 200:57-62.10.1016/S0022-510X(02)00133-8 [Google Scholar] [CrossRef]
[2]. Kranick SM, Price RS, Prasad S, Hurtig HI, Clinical reasoning: A 52-year-old woman with subacute hemichoreaNeurology 2008 71:e59-62.10.1212/01.wnl.0000334759.72146.3919001243 [Google Scholar] [CrossRef] [PubMed]
[3]. Nath J, Jambhekar K, Rao C, Armitano E, Radiological and pathological changes in hemiballism-hemichorea with striatal hyperintensityJournal of Magnetic Resonance Imaging 2006 23:564-68.10.1002/jmri.2054816514597 [Google Scholar] [CrossRef] [PubMed]
[4]. Awasthi D, Tiwari AK, Upadhyaya A, Singh B Tomar, Ketotic hyperglycaemia with movement disorderJ Emerg Trauma Shock 2012 5:90-91.10.4103/0974-2700.9309522416165 [Google Scholar] [CrossRef] [PubMed]
[5]. Suratos CT, Benitez JA, Urquiza SC, Sacro CA, Paediatric non-ketotic hyperglycaemic hemichorea-hemiballismusBMJ Case Reports 2018 2018:bcr-2017.10.1136/bcr-2017-22342929622707 [Google Scholar] [CrossRef] [PubMed]
[6]. Alves C, Sampaio S, Barbosa V, Machado M, Acute chorea and type 1 diabetes mellitus: Clinical and neuroimaging findingsPediatric Diabetes 2012 13:e30-34.10.1111/j.1399-5448.2012.00856.x22369150 [Google Scholar] [CrossRef] [PubMed]
[7]. Mihai CM, Catrinoiu D, Stoicescu RM, Atypical onset of diabetes in a teenage girl: A case reportCases J 2008 1:42510.1186/1757-1626-1-42519116001 [Google Scholar] [CrossRef] [PubMed]
[8]. Faundez T, Klee P, Hanquinet S, Schwitzgebel V, Burkhard PR, Korff CM, Diabetic striatopathy in childhood: A case reportPediatrics 2016 137(4):e2014376110.1542/peds.2014-376127012747 [Google Scholar] [CrossRef] [PubMed]
[9]. Aquino JH, Spitz M, Pereira JS, Hemichorea-hemiballismus as the first sign of type 1b diabetes during adolescence and its recurrence in the setting of infectionJournal of Child Neurology 2015 30(10):1362-65.10.1177/088307381455397225387546 [Google Scholar] [CrossRef] [PubMed]
[10]. Sperling M, Bhowansingh R, Chorea hyperglycaemia basal ganglia syndrome in a 63-year-old maleCase reports in medicine 2018 2018:910120710.1155/2018/910120730532787 [Google Scholar] [CrossRef] [PubMed]
[11]. Cheema H, Federman D, Kam A, Hemichorea-hemiballismus in non-ketotic hyperglycaemiaJournal of Clinical Neuroscience 2011 18:293-94.10.1016/j.jocn.2010.04.03621159513 [Google Scholar] [CrossRef] [PubMed]
[12]. Qi X, Yan Y, Gao Y, Zheng ZS, Chang Y, Hemichorea associated with non-ketotic hyperglycaemia: A case reportDiabetes Research and Clinical Practice 2012 95:e1-3.10.1016/j.diabres.2011.09.02021995866 [Google Scholar] [CrossRef] [PubMed]
[13]. Dwarak S, Prabhakar K, Kakanale M, Aswathanarayana A, Sindhu BR, Chorea, hyperglycaemia, basal ganglia syndrome in diabetes- two rare case reportsMaedica (Buchar) 2019 14:59-62. [Google Scholar]
[14]. Narayanan S, Hyperglycaemia-induced hemiballismus hemichorea: A case report and brief review of the literatureThe Journal of Emergency Medicine 2012 43:442-44.10.1016/j.jemermed.2010.05.00320566257 [Google Scholar] [CrossRef] [PubMed]
[15]. Bizet J, Cooper CJ, Quansah R, Rodriguez E, Teleb M, Hernandez GT, Chorea, Hyperglycaemia, Basal Ganglia Syndrome (C-H-BG) in an uncontrolled diabetic patient with normal glucose levels on presentationAm J Case Rep 2014 15:143-46.10.12659/AJCR.89017924744820 [Google Scholar] [CrossRef] [PubMed]
[16]. Cosentino C, Torres L, Nuñez Y, Suarez R, Velez M, Flores M, Hemichorea/hemiballism associated with hyperglycaemia: Report of 20 casesTremor and Other Hyperkinetic Movements 2016 :610.5334/tohm.29127536463 [Google Scholar] [CrossRef] [PubMed]
[17]. Bhidayasiri R, Truong DD, Chorea and related disordersPostgraduate Medical Journal 2004 80:527-34.10.1136/pgmj.2004.01935615356354 [Google Scholar] [CrossRef] [PubMed]
[18]. Arifi B, Gupta S, Sharma S, Daraboina A, Ahuja S, A case report of chorea associated with hyperthyroidismJ Clin Diagn Res 2016 10:PL0110.7860/JCDR/2016/17299.727727042533 [Google Scholar] [CrossRef] [PubMed]
[19]. Ahlskog JE, Nishino H, Evidente VG, Tulloch JW, Forbes GS, Caviness JN, Persistent chorea triggered by hyperglycaemic crisis in diabeticsMov Disord 2001 16:890-98.10.1002/mds.117111746619 [Google Scholar] [CrossRef] [PubMed]