Chronic Obstructive Pulmonary Disease (COPD) is characterised by respiratory symptoms which are persistent with airway and/or alveolar abnormalities which lead to airflow limitation due to significant exposure to noxious particles and gases. Loss of small airways contributes to mucociliary dysfunction.
Estimated number of COPD cases was 384 million in 2010 with a global prevalence of 11.7% [1]. Globally COPD causes around three million deaths anually [2]. The prevalence of COPD over the next 40 years is expected to rise and expected deaths from COPD and related conditions maybe over 5.4 million anually [3,4]. In 2005, COPD was the eighth leading cause of Disability Adjusted Life Years (DALYs) lost across the world but by 2013 COPD was ranked as fifth leading cause of DALYs lost [5].
AECOPD is defined as a sustained worsening of the patient’s respiratory symptoms that causes a change in the regular medication taken by the patient of COPD with usually upgradation of doses of drugs and/or addition of new drugs to the current medications depending on the severity of exacerbation [6,7]. Bacterial infection is one of the important cause of AECOPD and was found in studies done by Anthonisen NR et al., White AJ et al., and Papi A et al., however it has been found that the bacteria responsible for exacerbations of COPD differ in the Indian and Western population [8-10].
This study was done with the aim of finding microbiological profile and their sensitivity pattern in AECOPD patients to form an antibiogram which will help in the forming correct treatment protocol and to avoid unnecessary use of antibiotics preventing drug resistance.
Materials and Methods
The present prospective study was done in Department of Tuberculosis and Respiratory Diseases, in association with Department of Microbiology, JN Medical College, Aligarh, Uttar Pradesh, India for 1.5 years from November 2016 to June 2018. Institutional Ethical Committee (IEC) approval was obtained for the study. Informed consent was obtained from the study group.
A total of 200 patients admitted with the diagnosis of AECOPD were selected as study group. All the patients in the study group were more than 40 years of age.
Inclusion criteria: Patients (previously and currently diagnosed COPD) were selected as per GOLD guidelines [11] and Anthonisen criteria for exacerbation of COPD [8].
Exclusion criteria: Patients of COPD having bronchiectasis, sputum positive tuberculosis, lung malignancy and other evident disease on chest X-ray (pneumothorax, hydro-pneumothorax, pleural effusion, lung mass, lung abscess) were excluded. Patients with oral candidiasis were also excluded from the study.
All the sputum samples were collected under strict aseptic precautions in sterile containers, properly labeled and were transported to the laboratory in appropriate conditions and processed according to standard guidelines [12]. Bartlett grading system was used for microscopic analysis of sputum samples [13]. To each sputum sample 2% (w/v) N-acetyl-L cysteine and a few glass beads (2.5-3.5 mm) were added. A pH of 7.3 was adjusted. Homogenised samples were diluted in brain heart infusion broth and plated on blood agar, chocolate agar and MacConkey agar as following:
5% sheep Blood agar plate at 37°C for 24 hours, with 5-10% CO2
Chocholate agar plate, at 37°C for 24 hours, with 5-10% CO2
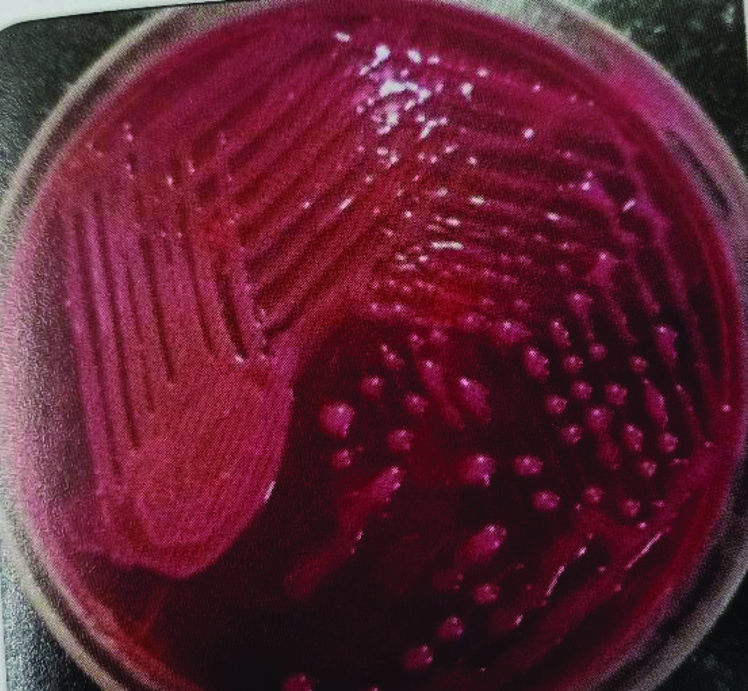
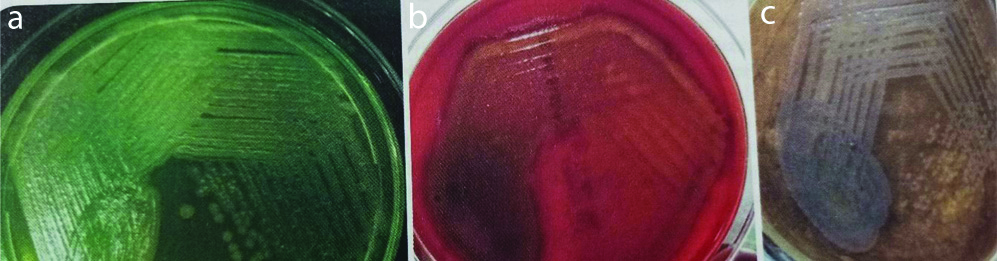
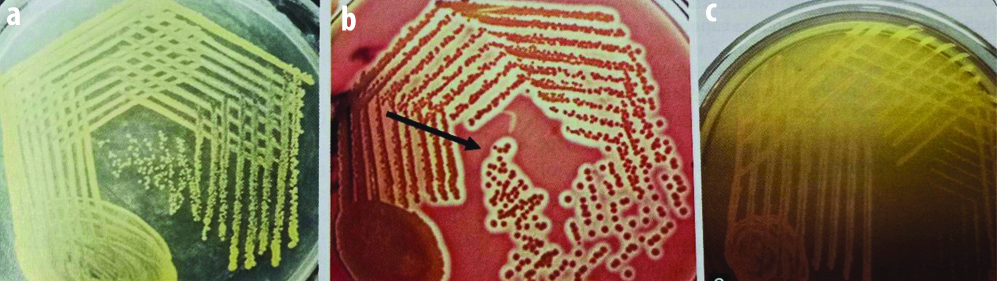
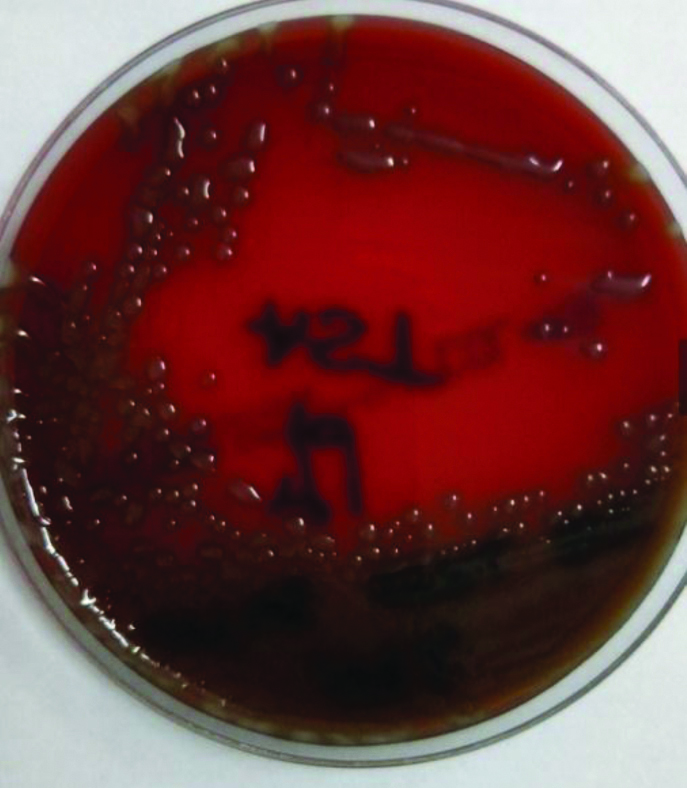
MacConkey agar plate, for 24 hours at 37°C in ambient air [Table/Fig-1,2,3 and 4]
Klebsiella on MacConkey agar showing mucoid dome shaped pink coloured lactose fermenting colonies.
a) Pseudomonas aeruginosa on nutrient agar with metallic sheen and green pigmentation, b) Blood agar showing moist colonies with beta haemolysis, c) MacConkey agar showing pale non-lactose fermenting with metallic sheen.
a) Staphylococcus aureus on nutrient agar showing golden yellow colonies, b) Blood agar showing beta haemolysis (shown by arrow), c) Mannitol agar showing yellow coloured colonies due to fermentation of mannitol.
Mucoid colonies of Streptococcus pneumoniae on 5% sheep blood agar.
The isolated colonies were identified by means of Gram’s stain, motility, catalase test, oxidase test, coagulase test and by various other biochemical reactions like Indole test, Methyl red test, Voges Proskauer test, Citrate utilisation test, Urease test, Triple sugar iron agar, Nitrate reduction test, Hugh-Leifsons oxidation fermentation test, coagulase production (for Staphylococcus), Optochin Sensitivity (for Streptococcus pneumoniae) were performed. Sugar fermentation tests with sugars viz., Glucose, Lactose, Sucrose, Maltose, Mannitol, Xylose, Arabinose and Dulcitol, Inositols etc., were done to identify the isolate according to standard laboratory procedures [14-16].
Antimicrobial susceptibility testing for Non-fastidious organisms was done by disc diffusion method using Kirby bauer technique on Mueller Hinton agar (HiMedia, Mumbai) [17], and for Fastidious organism on Mueller Hinton agar supplemented with 5% sheep blood using appropriate antimicrobial drugs as directed by CLSI guidelines [18].
Phenotypic screening was done for Extended Spectrum Beta Lactamases (ESBL) using disc diffusion method as per CLSI guidelines using Ceftazidime and Ceftriaxone. Antibiotic Break point zone diameter for possible ESBL strains was Ceftriaxone (30 μg) ≤25 mm and Ceftazidime (30 μg) ≤22 mm [19].
Phenotypic screening for metallo-betalactamases and Methicillin resistance was done with 0.5 Mcfarland’s suspension of test isolate lawn cultured on cation adjusted Mueller Hinton agar plates. Ten microgram (10 μg) Meropenem disc and 30 μg Cefoxitin disc was placed on the surface of lawn culture, incubated at 33-35°C; in ambient air for 16-18 hours. Isolates showing zone of inhibition <16 mm were positive for Carbapenamase production and ≤21 mm were considered as Methicillin resistant isolates [20,21].
All enterococcal isolates were tested for Vancomycin and High Level Aminoglycoside (HLA) resistance by disc diffusion method using high dose Gentamicin (120 mcg), Streptomycin (300 mcg) and Vancomycin (30 mcg) disc inoculated on Mueller hinton agar plate lawn cultured with 0.5 Mc Farland standard suspension of isolate. The plates were further incubated at 35°C for 18-24 hours and zone diameters were measured [22,23].
Direct microscopy using Gram stain and KOH mount was done for identification of fungal isolates. After initial inoculation and incubation; all culture media were examined daily in the first week and then every alternate day for three weeks for fungal growth. Identification of isolates was done on macroscopic and microscopic morphological characteristics using standard techniques [24]. Antifungal sensitivity testing was done by disc diffusion method using standard protocols [25-27].
Statistical Analysis
Statistical analysis was done by using SPSS version-20. The test applied in the current study was modified chi-square for comparison of proportion to analyse statistical significance for antibiotic sensitivity. The p-value <0.05 was considered statistically significant.
Results
A total of 200 patients were included in the present study with the diagnosis of AECOPD. [Table/Fig-5] shows age and sex distribution among study group. The majority of AECOPD patients were in the age group of 51-60 years of age (49.5%) with an overall predominance of males (74%) over females (26%).
Age and sex distribution among study group.
| Age in years | Male | Female | Total | % |
|---|
| 41-50 | 28 | 11 | 39 | 19.5 |
| 51-60 | 71 | 28 | 99 | 49.5 |
| 61-70 | 38 | 10 | 48 | 24 |
| >70 | 11 | 3 | 14 | 7 |
| Total | 148 | 52 | 200 | 100 |
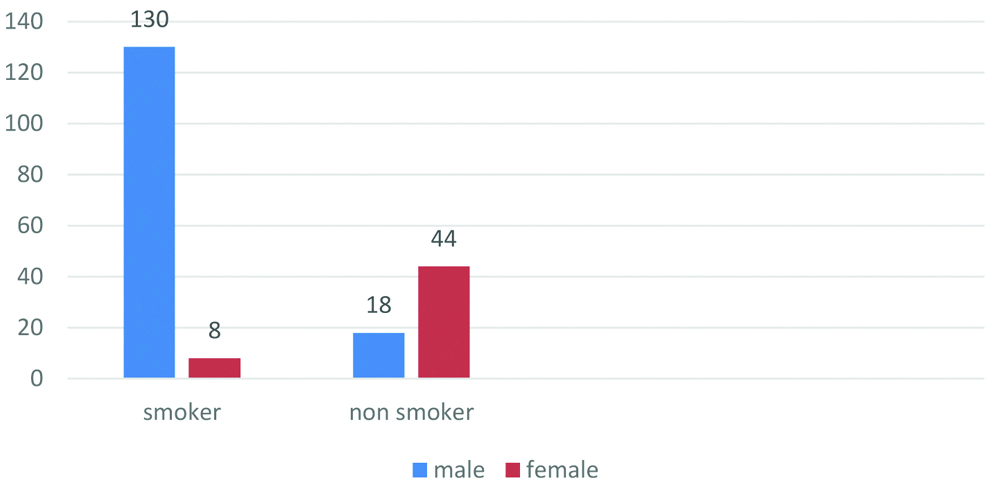
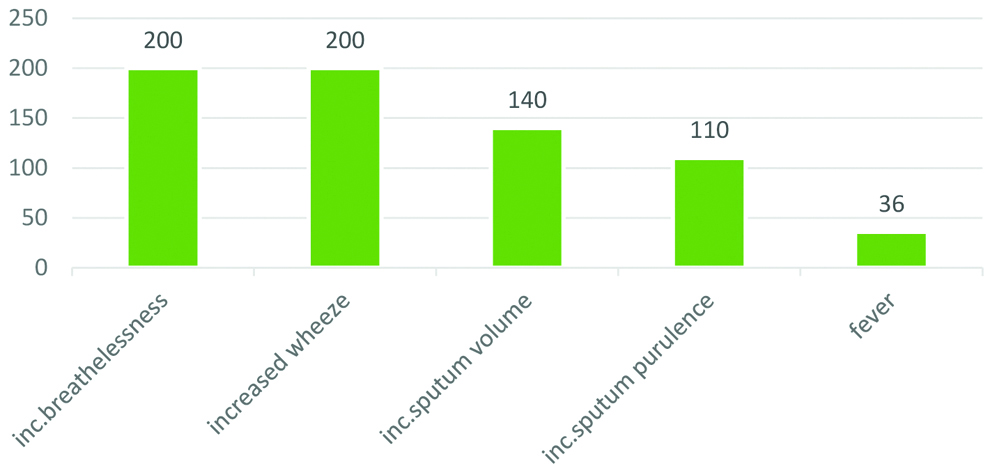
Smoking was associated with 138 (69%) [Table/Fig-6] patients in the current study of which 65% smokers were male and only 4% females were smokers. Among the 22% of non smoker females majority of them had the history of chulha smoking. Increased level of breathlessness and wheeze were the common symptoms in AECOPD (100%). Next most common symptom was increased in sputum volume (70%), and sputum purulence (55%) [Table/Fig-7].
Distribution of study group as smokers and non smokers.
Distribution of symptoms of study group.
Out of 200 patients, 78.5% showed culture positivity while 21.5% were culture negative [Table/Fig-8] Gram negative organisms (57.5%) predominated gram positive organisms (21%) among which monobacterial isolates were more common than polybacterial isolates (93% vs. 7%).
Bacterial culture results in sputum.
| No. of patients | % |
|---|
| Gram negative | 115 | 57.5 |
| Gram positive | 42 | 21 |
| Culture negative | 43 | 21.5 |
Among Gram negative organisms, Klebsiella sp. was most common isolate seen in 34 patients (21.6%) followed by Pseudomonas aeruginosa in 32 patients (20.7%), Moraxella catarrhalis in 26 patients (16.5%), E. coli in 12 patients (7.6%) and Citrobacter sp. in 11 patients (7%) [Table/Fig-9]. Among Gram positive organisms, Staphylococcus aureus was most commonly isolated in 21 patients (13.3%) followed by Streptococcus pneumoniae in 15 patients (9.5%), Enterococcus sp. in 3 patients (1.9%) and Coagulase negative Staphylococcus in 3 patients [Table/Fig-9].
Species distribution of gram negative and gram positive bacterial culture positivity.
| Isolates | No. of patients | Percentage (%) |
|---|
| Klebsiella sp. | 34 | 21.6 |
| Pseudomonas aeruginosa | 32 | 20.7 |
| Moraxella catarrhalis | 26 | 16.5 |
| Staph. aureus | 21 | 13.3 |
| Streptococcus pneumoniae | 15 | 9.5 |
| E. coli | 12 | 7.6 |
| Citrobacter sp. | 11 | 7.0 |
| CONS | 3 | 1.9 |
| Enterococcus sp. | 3 | 1.9 |
| No bacterial growth seen | 43 | 21.5 |
| Total | 157 | 100 |
CONS: coagulase-negative staphylococci
Isolated Klebsiella sp. were found resistant to Ceftazidime (100%), Cefoperazone-sulbactum (94.2%), Cotrimoxazole (85.3%), Cefixime (82.4%), Amoxyclav (82.4%), Ceftriaxone (79.5%), and Levofloxacin (70.6%). However, they were sensitive to Amikacin (41.1%) (p=0.006), Piperacillin-tazobactum (41.1%) (p=0.003), Meropenem (41.1%) (p=0.003), Levofloxacin (29.4%) (p=0.01), Ceftriaxone (20.5%) (p=0.07), Colistin (100%) (p<0.01), Tigecycline (100%) (p<0.01) and Polymyxin B (100%) (p<0.01) [Table/Fig-10]. Pseudomonas aeruginosa isolates were sensitive to Amikacin (84.3%) (p<0.01), Piperacillin-tazobactum (84.3%) (p<0.01), Levofloxacin (81.2%) (p<0.01), Meropenem (71.8%) (p<0.01). However, a high level of resistance was seen with Ceftazidime (93.8%), Aztreonam (93.8%) and Cefixime (75%) [Table/Fig-10]. All the isolated gram negative organisms were sensitive to Tigecycline (p<0.01), Polymyxin B (p<0.01) and Colistin (p<0.01). ESBL production by screening method was found in all isolates of Klebsiella sp., E.coli, Citobacter sp. and Moraxella catarrhalis and 30 isolates of Pseudomonas aerunisosa and by confirmatory method highest ESBL production was found in Citrobacter sp. (81.2% isolates) and lowest ESBL production in Moraxella catarrhalis (19.5% isolates) [Table/Fig-11]. Highest level of Metallobeta lactamases production was seen in Citobacter sp. (90.9% isolates) and lowest in Pseudomonas aeruginosa (26.47% isolates) and respectively by screening method [Table/Fig-12].
Antibiotic sensitivity pattern of gram negative isolates.
| Antibiotics | Klebsiella sp. (N=34) | E.coli (N=12) | Citrobacter sp. (N=11) | Moraxella catarrhalis (N=26) | Psedomonas aeruginosa (n=32) |
|---|
| S (%) | R (%) | S (%) | R (%) | S (%) | R (%) | S (%) | R (%) | S (%) | R (%) |
|---|
| Amikacin | 14 (41.1)p=0.006 | 20 (58.9) | 5 (41.6)p=0.06 | 7 (58.4) | 0 (0) | 11 (100) | 21 (80.7)p<0.01 | 5 (19.3) | 27 (84.3)p<0.01 | 5 (15.7) |
| Amoxy-clav. | 6 (17.6)p=0.13 | 28 (82.4) | 0 (0) | 12 (100) | 0 (0) | 11 (100) | 8 (30.7)p=0.54 | 18 (69.3) | - | - |
| Cefixime | 6 (17.6)p=0.13 | 28 (82.4) | 0 (0) | 12 (100) | 0 (0) | 11 (100) | 11 (42.3)p=0.14 | 15 (57.7) | 8 (25)p=1 | 24 (75) |
| Ceftriaxone | 7 (20.5)p=0.07 | 27 (79.5) | 0 (0) | 12 (100) | 0 (0) | 11 (100) | 16 (61.5)p=0.005 | 10 (38.5) | - | - |
| Cefo-sulbactum | 2 (5.8)p=1 | 32 (94.2) | 0 (0) | 12 (100) | 0 (0) | 11 (100) | 15 (57.7)p=0.01 | 11 (42.3) | - | - |
| Cotrimoxazole | 5 (14.7)p=0.23 | 29 (85.3) | 0 (0) | 12 (100) | 0 (0) | 11 (100) | 6 (23.1)p=1 | 20 (76.9) | - | - |
| Levofloxacin | 10 (29.4)p=0.01 | 24 (70.6) | 1 (8.3)p=1 | 11 (91.7) | 0 (0) | 11 (100) | 15 (57.7)p=0.01 | 11 (42.3) | 26 (81.2)p=1 | 6 (18.8) |
| Piptaz | 14 (41.1)p=0.003 | 20 (58.9) | 3 (25)p=0.28 | 9 (75) | 2 (18.1)p=0.54 | 9 (81.9) | 21 (80.7)p<0.01 | 5 (19.3) | 27 (84.3)p<0.01 | 5 (15.7) |
| Meropenem | 14 (41.1)p=0.003 | 20 (58.9) | 7 (58.3)p=0.01 | 5 (41.7) | 1 (9)p=1 | 10 (91) | 17 (65.3)p=0.02 | 9 (34.7) | 23 (71.8)p<0.01 | 9 (28.2) |
| Polymyxins | 16 (n=16)(100)p<0.01 | 0 (0) | 12 (100)p<0.01 | 0 (0) | 11 (100)p<0.01 | 0 (0) | 6 (n=6)(100)p<0.01 | 0 (0) | 6 (n=6) (100)p<0.01 | 0 (0) |
| Tigecycline | 16 (n=16) (100)p<0.01 | 0 (0) | 12 (100)p<0.01 | 0 (0) | 11 (100)p<0.01 | 0 (0) | 6 (n=6)(100)p<0.01 | 0 (0) | 6 (n=6) (100)p<0.01 | 0 (0) |
| Colistin | 16 (n=16) (100)p<0.01 | 0 (0) | 12 (100)p<0.01 | 0 (0) | 11 (100)p<0.01 | 0 (0) | 6 (n=6) (100)p<0.01 | 0 (0) | 6 (n=6) (100)p<0.01 | 0 (0) |
| Ceftazidime | 0 (0)p=1 | 34 (100) | 0 (0) | 12 (100) | 0 (0) | 11 (100) | 0 (0) | 26 (100) | 2 (6.2)p=1 | 30 (93.8) |
| Aztreonam | - | - | - | - | - | - | - | - | 2 (6.2)p=1 | 30 (93.8) |
Extended spectrum beta lactames production.
| S. No. | Isolates | Screening (Ceftazidime) | Confirmatory (Piperacillin Tazobactum) |
|---|
| R | % | R | % |
|---|
| 1 | Klebsiella sp. (n=34) | 34 | 100 | 20 | 58.8 |
| 2 | Pseudomonas aeruginosa (n=32) | 30 | 93.8 | 9 | 28.1 |
| 3 | E. coli (n=12) | 12 | 100 | 9 | 75 |
| 4 | Citrobacter sp. (n=11) | 11 | 100 | 9 | 81.2 |
| 5 | Moraxella catarrhalis (n=26) | 26 | 100 | 5 | 19.5 |
Metallobeta lactamases production.
| S. No. | Isolates | Screening-disc diffusion method |
|---|
| R | % |
|---|
| 1 | Klebsiella sp. (n=34) | 22 | 64.7 |
| 2 | Pseudomonas aeruginosa (n=32) | 9 | 26.47 |
| 3 | Moraxella catarrhalis (n=26) | 9 | 34.6 |
| 4 | E.coli (n=12) | 5 | 41.6 |
| 5 | Citrobacter sp. (n=11) | 10 | 90.9 |
Staphylococcus sp. isolates were sensitive to Vancomycin (83.3% (p<0.04), Amikacin (54.1%) (p=0.04) and Clindamycin (50%) (p=0.07). No resistance was seen with Linezolid, Tobramycin and Tigecycline. However, resistance was seen with azithromycin (79%), Amoxicillin-clavulinic acid (75%), Levofloxacin (75%) and Cotrimoxazole (58.4%) [Table/Fig-13]. In the current study MRSA by screening Cefoxitin disc diffusion method was found to be 62.5%. Streptococcus pneumoniae isolates were sensitive to Vancomycin (86.7%) (p<0.01), clindamycin (80%) (p<0.01), Ampicillin (73.3%) (p<0.01) and Doxycycline (60%) (p<0.01). However, isolated organisms were resistant to Levofloxacin (86.7%) and Azithromycin (80%). Enterococcus sp. was isolated from 3 AECOPD patients. The isolated organism was sensitive to Vancomycin (66.6%) (p=0.04) and Azithromycin (33.3%). No resistance was seen with high dose Gentamycin and high dose Streptomycin [Table/Fig-13]. Tests with Amikacin were not done.
Antibiotic sensitivity pattern of gram positive isolates.
| Antibiotics | Staphylococcus Sp. (N=24) | S.pneumoniae (N=15) | Enterococcus Sp. (N=3) |
|---|
| S (%) | R (%) | S (%) | R (%) | S (%) | R (%) |
|---|
| Amikacin | 13 (54.1)p=0.04 | 11 (45.9) | - | - | - | - |
| Amoxy-clav | 6 (25)p=1 | 18 (75) | - | - | - | - |
| Levofloxacin | 6 (25)p=1 | 18 (75) | 2 (13.3)p=1 | 13 (86.7) | 0 (0) | 3 (100) |
| Cotrimoxazole | 10 (41.6)p=0.22 | 14 (58.4) | - | - | - | - |
| Cefoxitin | 9 (37.5)p=0.35 | 15 (62.5) | - | - | - | - |
| Clindamycin | 12 (50)p=0.07 | 12 (50) | 12 (80)p<0.01 | 3 (20) | 0 (0) | 3 (100) |
| Azithromycin | 5 (20.8)p=1 | 19 (79.2) | 3 (20)p=0.62 | 12 (80) | 1 (33.3)p=1 | 2 (66.6) |
| Vancomycin | 20 (83.3)p<0.04 | 4 (16.7) | 13 (86.7)p<0.01 | 2 (13.3) | 2 (66.6)p=0.04 | 1 (33.3) |
| Tobramycin (n=4) | 4 (100)p<0.01 | 0 (0) | - | - | - | - |
| Linezolid (n=4) | 4 (100)p<0.01 | 0 (0) | - | - | - | - |
| Tigecycline (n=8) | 8 (100)p<0.01 | 0 (0) | - | - | - | - |
| Doxycycline | - | - | 9 (60)p<0.01 | 6 (40) | 0 (0) | 3 (100) |
| Ampicillin | - | - | 11 (73.3)p<0.01 | 4 (26.7) | 0 (0) | 3 (100) |
| High dose gentamicin | - | - | - | - | 3 (100)p<0.01 | 0 (0) |
| High dose streptomycin | - | - | - | - | 3 (100)p<0.01 | 0 (0) |
In the present study, out of 200 patients fungal growth was seen in only 49 (24.5%) patients of which 37 (75.5%) patients showed Candida sp. and 12 (24.5%) patients showed Aspergillus sp.
Among fungal isolates no resistance was seen with Candida sp. to Itraconazole, Ketoconazole, Amphotericin B, Nystatin, Cotrimazole, Caspofungin and Flucytosine [Table/Fig-14]. Aspergillus sp. all were sensitive to Caspofungin and Amphotericin B and 75% isolates were sensitive to Itraconazole and Ketoconazole [Table/Fig-14].
Antibiotic sensitivity pattern of fungal isolates.
| Antibiotic | Candida sp. (N=37) | Aspergillus sp. (N=12) |
|---|
| S (%) | R (%) | S(%) | R(%) |
|---|
| Caspofungin | 37 (100)p<0.01 | 0 (0) | 12 (100)p<0.01 | 0 (0) |
| Itraconazole | 37 (100)p<0.01 | 0 (0) | 9 (75)p<0.01 | 3 (25) |
| Amphotericin B | 37 (100)p<0.01 | 0 (0) | 12 (100)p<0.01 | 0 (0) |
| Flucytosine | 37 (100)p<0.01 | 0 (0) | - | - |
| Nystatin | 37 (100)p<0.01 | 0 (0) | - | - |
| Ketoconazole | 37 (100)p<0.01 | 0 (0) | 9 (75)p<0.01 | 3 (25) |
| Clotrimazole | 37 (100)p<0.01 | 0 (0) | - | - |
Discussion
In the present study microbiological spectrum was analysed in 200 AECOPD cases. The majority of patients were in the age group of 51-60 years of age (49.5%) followed by age group of 61-70 years (24%) with a predominance of males (74%) over females (26%). This can be explained by the fact that COPD has the highest prevalence in fifth and sixth decade of life. As age advances, the physiological decrease in lung function is accentuated by the cumulative damage done by smoking and other co-morbid conditions. Other studies also showed a similar results as done by Saxena S et al., (43% in 55-65 years age; 68% male, 32% female [28], Rakesh G et al., (the most common age group was 55 years constituting 43%; 70% male, 30% female) [29].
Men have pronounced smoking habits and are exposed more to outside environment as compared to females. Smoking leads to decreased mucociliary clearance and innate immunity thereby leading to increased bacterial colonisation that can give rise to increased airway inflammation and thus exacerbation. Smoking was associated with 138 (69%) patients in the current study of which 65% smokers were male and only 4% females were smokers. Among the 22% of non smoker females majority of them had the history of chulha smoking. There is a growing evidence that indoor biomass exposure to modern and traditional fuels used during cooking may predispose women to develop COPD in many developing countries [30-32]. Occupational exposure, organic and inorganic dusts, chemical agents and fumes are an under appreciated risk factor for COPD among nonsmokers [33,34]. Other studies also showed a predominance of smokers in AECOPD like by Sharan H (62.5% smokers) [35] and Rakesh G et al., (70% smokers) [29].
Culture results (78.5% culture positive vs. 21.5% culture negative) of current study were similar as found in other studies like Madhavi S et al., (55% culture positive) [36], Arora N et al., (72% culture positive) [37]. Gram negative organisms (57.5%) predominated gram positive organisms (21.0%) which were in accordance with results of studies done by Saxena S et al., (gram negative 65.95%; 34.04% of gram positive) [28], Sharan H (gram negative 61.54%; gram positive 38.46%) [35], Rakesh G et al., [29] (gram negative 51.3%; 48.64% gram positive isolates), Madhavi S et al., (75% gram negative; 25% gram positive) [36]. In this study, it was found that monobacterial isolates were more common than polybacterial isolates (93% vs. 7%). Similar results were observed by Saxena S et al., (37% single bacterial isolates and 5% double bacterial isolates), Rakesh G et al., (51.35% of monobacterial isolates and 5% of polybacterial isolates), Chawla K et al., (monobacterial growth 92.85% and growth of two organisms was isolated in 7.14% cases) [28,29,38], however, it is not of much clinical significance. Culture results of gram positive and negative isolates were in accordance with other studies done by, Madhavi S et al., (Klebsiella pneumonia 59%, followed by Pseudomonas aeruginosa 15%, Staphylococcus aureus 13.6%, Streptococcus. 8%) [36], Patel AK et al., (Klebsiella pneumonia 59%) [39], Saxena S et al., (Klebsiella pneumoniae 42.55%, followed by Staphylococcus aureus 28.73%, P. aeruginosa 14.89%, E coli 8.51%, CONS 4.26%, S pneumoniae 1.06%) [28]. Similar results were seen in other studies done by Sharan H, Pradhan KC et al., and Babu D et al., [35,40,41]. Gram negative isolates were found to be sensitive to piperacillin-tazobactum, amikacin, meropenem, levofloxacin and resistant to mainly ceftazidime, cotrimoxazole, cefixime, amoxicillin-clavulinic acid and aztreonam. Gram positive isolates were sensitive to Vancomycin, Ampicillin, Doxycycline, Clindamycin, high dose streptomycin and high dose gentamicin and resistance was seen with Azithromycin and Levofloxacin. Among gram negative isolates no resistance was seen with polymyxin B, colistin and tigecycline. Fungal growth was seen in only 49 (24.5%) patients of which 37 (75.5%) patients showed Candida sp. and 12 (24.5%) patients showed Aspergillus sp. In a study done by Huerta A et al., prevalence of Aspergillus sp. isolation was 16.6% on admission [42]. The independent risk factors associated with Aspergillus sp. colonisation were AECOPD and concurrent isolation of Progressive Multiple Sclerosis (PPMs), most frequently Pseudomonas aeruginosa. Fungal isolates were found to be sensitive to commonly used antifungals such as Itraconazole, Ketoconazole, Amphotericin B, Nystatin, Cotrimazole and Caspofungin.
Exacerbations of COPD is mostly an infectious aetiology and are a frequent cause of morbidity in COPD patients. Present study and few previous Indian studies (discussed above) have shown that bacterial pathogens responsible for AECOPD is different in India from that of western countries and so is their sensitivity pattern so periodic isolation and the knowledge of resistance pattern will help in formulating the antibiogram.
Limitation(s)
One of the limitations of the study was that no information was collected about viral infections in AECOPD as viruses are an important cause of exacerbation of COPD. The other limitation being only qualitative analysis of antimicrobial and antifungal sensitivity and resistance was done, quantitative analysis was not done. Confirmatory test for metallobeta lactamases production was also not done.
Conclusion(s)
Exacerbations punctuate the clinical course of COPD in patients leading to increased morbidity and mortality. A high level of resistance to commonly used antibiotics is emerging due to incorrect diagnosis and inappropriate use of antibiotics. Periodic isolation and identification of microbiological profile and sensitivity pattern for AECOPD will help in formulating local antibiotic policy and treatment protocol to help reduce the morbidity, mortality and emerging high level of resistance to antibiotics. Further studies are required for fungal culture and sensitivity to determine whether the isolated organisms exist only as commensal or responsible for causing disease.
CONS: coagulase-negative staphylococci