Myofascial Pain Syndrome (MPS) is one of the most common causes of muscle pain. MPS is characterised by the presence of trigger points that form a taut band in the muscle. The aim of this review was to evaluate the literature related to MPS and to analyse the outcome of Myofascial Release (MFR) Techniques for various musculoskeletal conditions from published articles. Online search engines such as MEDLINE, PubMed, Google scholar and Physiotherapy Evidence Database (PEDro) were searched. There were no limitations for dates applied to the review article. Sixteen articles were selected with the terms MFR techniques used. The data were tabulated according to the type of study, number of participants in the study, the condition being treated, treatment given, outcome measures, and results. This literature review found mixed responses to the outcomes of MFR techniques. These contrasting results reveal the need for future research. This may help researchers to conduct Randomised Controlled Trials (RCT) using MFR and further develop protocols to enhance better interpretations and the need for evidence-based information.
Fascia, Myofascial release therapy, Musculoskeletal conditions, Pain, Trigger point release
Introduction
The MPS is a musculoskeletal pain producing condition and has few localised trigger points. History and evaluation play a major role in the diagnosis of MPS [1]. There are varied manual therapy techniques to treat MPS and one of them is MFR therapy techniques which has become very popular over the past years. Michigan State University had first coined the term MFR in a course they had conducted in the late ‘80s [2].
Fascia is divided into three layers of connective tissues- the superficial layer, a layer of potential space, and an innermost layer. These continuously connected sheets are present around single muscles, that cover muscle tendon, joint capsules and/or the periosteum and create tensegrity in the body [3,4].
Taut bands that develop within the muscle fibers are sensitive spots and are termed trigger points. These taut bands are located by palpation [4]. The taut bands are classified into active or latent trigger points. Active Trigger Points (ATrPs) produce tenderness, spontaneous pain and are associated with reduced range of motion whereas Latent Trigger Points (LTrPs) are developed by maintaining the muscle in a shortened position for a long duration and are associated with tenderness, twitch response, and referred pain [4]. When the trigger points are compressed on palpation, subjects respond with a facial grimace or verbal cue which is termed as a “jump sign” [5]. The musculoskeletal systems is an intricate network of interconnected tissues that work in unison to provide movement efficiently. Muscular functions are inhibited when the muscles and fascia undergo microtrauma. These Myofascial Trigger Points (MTrP) which develop in the fascia can result in decreased range of motion, strength, and changes in neuromuscular properties. As the fibers of the fascia run in many directions, it is able to move and change with the surrounding tissues [2]. Due to overuse syndromes, the connective tissues become thicker and alter the collagen fiber composition of muscles and causes changes in the ground substance [5-9]. There are various types of MFR techniques to release trigger points. These depend on the biomechanical loading of tissues and modifications of neural reflex by stimulation of fascia mechano receptors [2].
Based on the application techniques, MFR techniques involve direct MFR technique or indirect MFR technique. In direct MFR technique, the trigger point is released by the use of elbow or a tool by which the practitioner stretches the fascia. The indirect MFR technique involves a gentle stretch with minimal pressure and the hand follows the direction of the fascial restriction. This is also called passive MFR techniques as minimal pressure is applied to the tissue and the subject remains passive during treatment [10].
Mechanism underlying the MFR is the fascia which is the most restricted position and continuous pressure is applied here for 90-120 seconds, histological length changes occur in the tissue and the first release is felt. Once the tissue barriers are released in one area, the practitioner follows the release into a new tissue barrier and hold. After a few releases, the tissue becomes pliable. As the length to the myofascial tissue is restored, the pressure reduces from the affected structures and the mobility and alignment to the joints are restored [6].
As the fascia has a dynamic function, it does not follow any specific pain patterns because of which pain due to trigger points can be difficult to diagnose. This can be treated using various hand skill techniques but according to Kidd RF, there is not much research to support this [11].
The results of MFR rely on the experience and skills of the therapist and this being a manual therapy technique depends on the ability to feel the changes in the tissue. Some authors suggest that it cannot be evidence-based as the results of the treatment are subjective. In the past, the same argument was applied to different techniques applied using hand and nowadays they are considered as research based on evidence [11].
Therefore, the main purpose of this review article was to critically analyse the outcome of MFR as a treatment technique for myofascial pain conditions and to gather documented evidences for MFR.
Materials and Methods
Literature Search Methodology
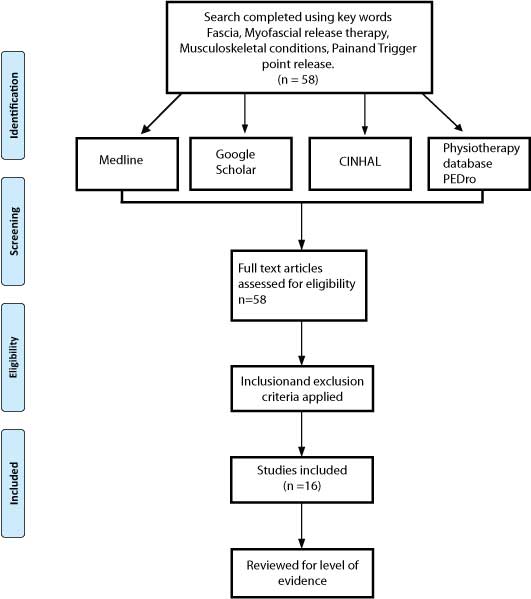
Online search engines used to collect journals were MEDLINE, Google Scholar, PEDro, and CINHAL. The authors identified articles based on the keywords. The articles were collected in full text. A total of 58 articles were identified, out of which 16 were selected for review [Table/Fig-1].
Study flow diagram.
CEBM: Centre for evidence based medicine
Study Selection
Data extraction: The data which was collected were tabulated based on the sample size, treatment given, outcome measures used, the results obtained, level of evidence were arranged in chronological order. The CEBM levels of evidence were used to assess the quality of the study [12].
Inclusion criteria: (1) published in English language only; (2) Direct or indirect MFR techniques; (3) published in peer review journals only; (4) adult human participants were studied. The studies which were only systematic reviews and RCTs were included for the study.
Exclusion criteria: (1) editorials expert opinion; (2) case studies; (3) individual case-control studies were excluded from the study.
Literature Evaluation
The results of the research varied widely. Out of the 58 original articles, 16 articles were eligible as per the inclusion criteria. Studies ranged from systematic review to RCT, excluding case studies. There were no limitations for dates applied to the review article. The studies were grouped into two categories, 2 Systematic reviews and 14 RCTs. There was no overlap of studies in both the systematic reviews. The selected articles were checked for the level of evidence using Centre for Evidence-Based Medicine (CEBM) [Table/Fig-2] [4,13-27]. One study was rated as 1a, four studies as 1b, and 11 studies were rated as 2b according to CEBM levels of evidence.
Study results and level of evidence grading included in this review [4,13-27].
| Sl. no. | Authors | Study design | Participants no. | Condition | Treatment | Control group | Outcome measure | Results | Level of evidence |
|---|
| 1 | Kisilewicz A et al., [13] | RCT | 12 | Unilateral neck or shoulder pain in basketball players | Compression trigger point therapy | Nil | Myoton PRO device | stiffness decreased with single session | 2b |
| 2 | Laimi K et al., [14] | Systematic review | 8 studies | Chronic musculoskeletal pain | MFR | NA | ROM & QOL | Effective in reducing pain and improving function | 2b |
| 3 | Gutiérrez-Rojas C et al., [15] | RCT | 30 | Trigger Point in the forearm of young adults | Ice, MFR, | Ice and MFR | Nil | PPT, PPP, Flexor and extensor strength of forearm | MFR &Ice showed better improvement in PPT | 1b |
| 4 | Cagnie B et al., [4] | Systematic review. | 15 studies. | Upper trapezius MFTrP | Ischemic Compression and Dry Needling | NA | Pain, range of motion, functionality, and quality-of-life, including depression | IC &DN showed positive results | 1a |
| 5 | Ravish VN et al., [16] | RCT | 60 | Unilateral trapezitis | MFR, PRT with LASER | Nil | CROM, VAS, NDI | MFR with LASER showed better improvement. | 2b |
| 6 | Chaudhary ES et al., [17] | RCT | 45 | Upper trapezius spasm | MFR, cold pack and exercises | NIL | VAS, PPT ROM | MFR &Exercise showed better results | 2b |
| 7 | Ajimsha MS et al., [18] | RCT | 68 | Lateral epicondylitis | MFR. Sham US | Sham US | PRTEE | MFR is effective-Pain decreased | 2b |
| 8 | Kain J et al., [19] | RCT | 31 | Chronic myogenous TMJ disorders | indirect MFR for 3 min | Moist heat for 20 min | PROM | MFR is effective as hot packs in increasing ROM | 2b |
| 9 | Renan-Ordine R et al., [20] | RCT | 60 | Plantar heel pain | SST&MFR | SST | QOL-SF 36, PPT | MFR is superior to SST group. | 1b |
| 10 | Tozzi P et al., [21] | RCT | 120 | Non-specific cervical (NP) or lumbar pain (LBP) | NP: MFR 6 min LBP: MFR 12 Min single session | NP: Sham MFR 6 Min LBP: Sham MFR 12 min | dynamic ultrasound (US) | MFR group -Pain reduced in NP & LBP | 2b |
| 11 | Kalamir A et al., [22] | RCT | 30 | Chronic myogenic TMJ disorders | MFR-15 min, MFR 15 min with self care and exercises | Nil | Pain and ROM | MFR alone or with self-care is beneficial | 2b |
| 12 | Aguilera FJM et al., [23] | RCT | 66 | Myofascial trigger points (MTrPs) in the trapezius muscle. | Ischemic compression (IC) and ultrasound (US) | Sham US | AROM, BEA of the upper trapezius muscle, PPT, VAS | IC AND US improved but not sham US | 1b |
| 13 | Kuhar S et al., [24] | RCT | 30 | Plantar fasciitis | Ultrasound, contrast bath, exercises, MFR | Ultrasound, contrast bath, exercises | FFI, VAS | Significant reduction in VAS and FFI | 2b |
| 14 | Hsieh CYJ et al., [25] | RCT | 200 | Sub-acute LBP | MFR, Back school, manipulation, and combined therapy | Nil | VAS, Roland Morris activity scale, | No difference among groups; back pain improved in all | 1b |
| 15 | Barnes MF et al., [26] | RCT | 10 | Unilateral pelvic rotation | MFR to the pelvic region, 10 min | Rest 10 min | Pelvic position | MFR showed better pelvic rotation | 2b |
| 16 | Hante WP and Chandler SD [27] | RCT | 75 | Hamstrings tightness | MFR to lower extremity, contract-relax PNF | Supine rest 35 min | Passive straight-leg-raise | PNF showed better results than MFR | 2b |
US: Ultrasound; MFR: Myofascial release; IC: Ischemic compression; ROM: Range of motion; QOL: Quality of life; PPP: Pressure pain perception; PNF: Proprioceptive neuromuscular facilitation; NDI: Neck disability index; PRTEE: Patient rated tennis elbow evaluation; SST: Somatostatin; MFTrP: Myofascial trigger point; DN: Dry needling-positional release therapy; CROM: Cervical range of motion; VAS: Visual analogue scale; PPT: Pain pressure threshold-Neck Pain; LBP: Low back pain; AROM: Active range of motion; BEA: Basal electrical activity; FFI-Foot function Index; TMJ: Temporomandibular joint; PROM: Passive range of motion
1a- The study was a systematic review with homogeneity of RCTs; 1b- Individual RCT with narrow Confidence Interval; 2b Individual cohort study including low quality RCT
Data Synthesis
The study by Cagnie B et al., conducted a high-quality study, ranked at level 1a according to the CEBM, levels of Evidence scale denotes a high-quality work [4]. The 1a rating reflects that the study was a systematic review with homogeneity of RCTs. This study compared the effectiveness of ischaemic compression and dry needling in trigger points of upper trapezius and neck pain, and concluded that both dry needling had strong evidence compared to MFR on pain and also inferred that more research is required to develop conclusive evidence. Four studies were categorised in 1b of the CEBM denoting high quality studies [15,20,23,25].
Gutiérrez-Rojas C et al., conducted an RCT with repeated measures design to study the effect of MFR with ice on latent MTrP in the forearm of young adults. They concluded that all the groups had favourable effects on pain. The major drawback of this study was that the sample size was small and there was no follow-up. The level of activity performed and their psychological status was not evaluated [15].
An RCT on 60 subjects to find the effect of trigger point release manual therapy combined with self-stretching of the calf muscles in unilateral plantar fasciitis for 4 days a week for 4 weeks. The study had no control group and hence it was not possible to say that whether trigger point release therapy with self-stretching was superior. The study only assessed the short-term effects and the long-term effects were not known. Though the study showed that trigger point release with self-stretching was effective, the blinding was not mentioned. Further, the SF-36 questionnaire used had poor sensitivity to pain, trigger point and not condition-specific [20]. Aguilera FJM et al., conducted an RCT that was rated at a level of 1b on the CEBM. The purpose was to determine the immediate effect of Ultrasound and Ischemic compression on a latent myofascial trigger point in the upper trapezius. In this study, the same examiner did the pre and post-test measurement and another examiner applied the treatment to all groups. Only the third group was blinded. The study results had a positive outcome but only the immediate effects of MFR were known [23]. The study by Hsieh CYJ et al., was a well-designed and strong study with a high PEDro score of 7 out of 10 and CEBM level 1b. The study had adequate participants with a follow-up. And it concluded that it is relevant to use MFR as a treatment [25].
The study of Kisilewicz A et al., was ranked 2b. This study assessed the effects of compression trigger point therapy on the trapezius muscle in professional basketball players. The small sample size resulted in a lack of significant difference in stiffness of the middle and lower trapezius. Since it was a single session study, it lessened the quality of the study. As the participants were professional basketball players, the results of this study could not be applied to the general population [13].
Laimi K et al., conducted a systematic review with 8 RCT’s to find the effectiveness of MFR in musculoskeletal conditions. This study was ranked 2b in the level of evidence. Since their criteria were only chronic cases, the results of the studies would not be used for acute cases [14].
Barnes MF et al., conducted a study that was of high-quality and ranked at 2b with a PEDro score of 8 out of 10. But the CEBM rating of the level of evidence was lowered due to the small sample size being 10. The authors had stated that 23 participants were required in the experimental group and 15 in the control group for data analysis. There was a lack of follow-up measurements in the study [26].
The study by Kuhar S et al., was ranked 2b which earned a 7 out of 10 in the PEDro scale. This study used MFR to treat plantar fasciitis. This study did not have a follow-up and only pre- and post-treatment measurements were taken which lessened the quality of the study. To know the long-term effects of the treatment procedure, follow-up measurements are required [24].
The study by Hanten WP and Chandler SD was ranked 2b on the CEBM scale. The score on the PEDro scale being 6 out of 10. This study compared MFR and Proprioceptive Neuromuscular Facilitation (PNF) stretching in improving the angle of straight-leg-raise. The results of the study showed that PNF was better than MFR. Though PNF proved to be effective, there was no random selection of participants and follow-up which reduced the quality of the study [27].
The study by Chaudhary ES et al., compared the MFR and cold for the spasm of the upper trapezius. The article stated that MFR was effective than cold. Though there was randomisation of subjects, there was no blinding done. The sample size was small and no follow-up measurement is done which brought down the quality of the study and could not come to conclusive evidence on the effects of MFR [17].
Ajimsha MS et al., conducted a study to find the effect of MFR in lateral epicondylitis for computer professionals [18]. This study was rated 2b on the CEBM level of evidence and the PEDro score was 6 out of 10. Randomisation and follow-up measurements were done It was a single-blinded study and also had a control group. This study proved that MFR is a good choice of treatment for Lateral epicondylitis.
The study is done by Kain J et al., to compare the effect of MFR and hot pack in increasing the ROM [19]. This study was rated 2b and the results of the study showed that both types of treatment were equal. The sample size was small and no blinding was done. The treatment was given only once with no follow-up measurement, and hence the quality of the study was low. The results of this study could not be generalised for other musculoskeletal conditions. The study by Ravish VN et al., was conducted to compare the effects of MFR and PRT with LASER in subjects with unilateral trapezitis [16]. This study was ranked 2b. The results of the study proved that MFR with LASER showed significant improvement. Though the study showed positive results towards MFR, there was no randomisation and blinding done and there was also no follow-up. So, it could not be concluded that MFR is a better choice.
In the 2b ranking studies, the number of subjects was less and the treatment had no follow-up there was no blinding of subjects or therapists or assessors. Overall, few studies had shown MFR to be effective and few studies had shown it to be equally effective to other conservative treatment given.
Discussion
In this review, there were fourteen RCTs and two systematic reviews. The sample size in the RCTs varied from 10 to 120 with a mean of 59.8. The CEBM levels of evidence assess quality based on the study design. RCTs received higher ranking particularly with long term follow-up and narrow confidence intervals. The number of studies in the systematic reviews was 8 studies and 15 studies respectively and the sample size varied from 23 to 117. The total number of samples inclusive of the systematic review and RCTs were 1697.
The results of the studies were encouraging with 12 of the RCTs stated that MFR given along with other treatment was effective in reducing the symptoms. Since MFR was given as an adjunct to other treatments, the specific response could not be judged [13-26].
Another study stated that MFR was not effective when compared to PNF therapy and this study was conducted by Hanten WP and Chandler SD who stated that though MFR was found to be effective in reducing hamstring tightness against a group receiving no treatment, the effect was inferior to PNF treatment [27]. Two studies concluded that MFR is better than placebo treatment for various MPSs. One study demonstrated when only MFR was given, it did show a decrease in symptoms. One study showed no difference to the treatment given [18,21]. Out of the fourteen RCTs, six of them did not have a control group. Different varieties of conditions are treated by MFR however; evidence is required to support its efficacy. Hence, the experimental studies in this review can be a starting point for further research [13-17,22,25]. RCTs with a follow-up, double-blinding and objective outcome measurement could be categorised as high-quality studies as per CEBM levels of evidence.
From these studies, it is clear that the results are mixed. Few articles showed that MFR was superior to other treatment techniques whereas the rest showed that other treatment techniques were equally effective for that particular condition. Since few of the articles only had a pre- and post-treatment measurement with no follow-up, to comment on the long-term effects would be impossible This indicates that more research is required to determine the effectiveness of MFR. Though not statistically significant, all studies showed that MFR had some positive practical effects.
To achieve high scores in the PEDro scale, a random sampling technique with blinding of participants and assessor could be done with repeated post-test measurements and follow-up treatment. The control group or sham group could be compared with MFR along with other evidence-based treatment methods.
Limitation(s)
The studies which were included in this review were heterogeneous in terms of population, the type of MFR given and duration of treatment session. Though all possible published RCTs were searched, some relevant studies might have been missed. Due to resource constraints, publications only in English were reviewed.
Conclusion(s)
This literature review analysed the effects of MFR for MPSs. The wide range of RCTs and systematic reviews used demonstrates that MFR can be a choice of treatment for musculoskeletal conditions and it is of prime importance to have evidence for these. The guidelines given in this review will help us to achieve higher quality results and to also determine the true effectiveness of MFR as a treatment for MPS.
[1]. Desai MJ, Saini V, Saini S, Myofascial pain syndrome: A treatment reviewPain Ther 2013 2(1):21-36.10.1007/s40122-013-0006-y25135034 [Google Scholar] [CrossRef] [PubMed]
[2]. McKenney K, Elder AS, Elder C, Hutchins A, Myofascial release as a treatment for orthopaedic conditions: A systematic reviewJ Athl Train 2013 48(4):522-27.10.4085/1062-6050-48.3.1723725488 [Google Scholar] [CrossRef] [PubMed]
[3]. Stecco C, Macchi V, Porzionato A, Duparc F, De Caro R, The fascia: The forgotten structureItal J Anat Embryol 2011 116(3):127-38. [Google Scholar]
[4]. Cagnie B, Castelein B, Pollie F, Steelant L, Verhoeyen H, Cools A, Evidence for the use of ischemic compression and dry needling in the management of trigger points of the upper trapezius in patients with neck pain: A systematic reviewAm J Phys Med Rehabil 2015 94(7):573-83.10.1097/PHM.000000000000026625768071 [Google Scholar] [CrossRef] [PubMed]
[5]. Travell JG, Simons DG, Myofascial pain and dysfunction: The trigger point manual: Volume 1, The upper half of body, Second edition 1999 BaltimoreWilliams & Wilkins:11-86. [Google Scholar]
[6]. Langevin HM, Fox JR, Koptiuch C, Badger GJ, Greenan-Naumann AC, Bouffard NA, Reduced thoracolumbar fascia shear strain in human chronic low back painBMC Musculoskelet Disord 2011 12:20310.1186/1471-2474-12-20321929806 [Google Scholar] [CrossRef] [PubMed]
[7]. Ajimsha MS, Effectiveness of direct vs indirect technique myofascial release in the management of tension-type headacheJ Body Mov Ther 2011 15(4):431-35.10.1016/j.jbmt.2011.01.02121943616 [Google Scholar] [CrossRef] [PubMed]
[8]. Day JA, Stecco C, Stecco A, Application of fascial manipulation technique in chronic shoulder pain- Anatomical basis and clinical implicationsJ Bodyw Mov Ther 2009 13(2):128-35.10.1016/j.jbmt.2008.04.04419329049 [Google Scholar] [CrossRef] [PubMed]
[9]. Stecco A, Gesi M, Stecco C, Stern R, Fascial Components of the myofascial pain syndromeCurr Pain Headache Rep 2013 17(8):35210.1007/s11916-013-0352-923801005 [Google Scholar] [CrossRef] [PubMed]
[10]. Schleip R, Fascial plasticity- A new neurobiological explanation: Part 1Journal of Bodywork and Movement Therapies 2003 7(1):11-19.10.1016/S1360-8592(02)00067-0 [Google Scholar] [CrossRef]
[11]. Kidd RF, Why myofascial release will never be evidence-basedInternational Musculoskeletal Medicine 2009 31(2):55-56.10.1179/175361409X412575 [Google Scholar] [CrossRef]
[12]. Burns PB, Rohrich RJ, Chung KC, The levels of evidence and their role in evidence-based medicinePlast Reconstr Surg 2011 128(1):305-10.10.1097/PRS.0b013e318219c17121701348 [Google Scholar] [CrossRef] [PubMed]
[13]. Kisilewicz A, Janusiak M, Szafraniec R, Smoter M, Ciszek B, Madeleine P, Changes in muscle stiffness of the trapezius muscle after application of ischemic compression into myofascial trigger points in professional basketball playersJ Hum Kinet 2018 64:35-45.10.2478/hukin-2018-004330429897 [Google Scholar] [CrossRef] [PubMed]
[14]. Laimi K, Mäkilä A, Bärlund E, Katajapuu N, Oksanen A, Seikkula V, Effectiveness of myofascial release in treatment of chronic musculoskeletal pain: A systematic reviewClin Rehabil 2018 32(4):440-50.10.1177/026921551773282028956477 [Google Scholar] [CrossRef] [PubMed]
[15]. Gutiérrez-Rojas C, González I, Navarrete E, Olivares E, Rojas J, Tordecilla D, The effect of combining myofascial release with ice application on a latent trigger point in the forearm of young: A randomized clinical trialMyopain 2015 23(3-4):201-08.10.1080/24708593.2017.1403526 [Google Scholar] [CrossRef]
[16]. Ravish VN, Shridhar S, Helen S, To compare the effectiveness of myofascial release technique versus positional release technique with laser in patients with unilateral trapezitisJournal of Evolution of Medical and Dental Sciences 2014 3(9):2161-66.10.14260/jemds/2014/2121 [Google Scholar] [CrossRef]
[17]. Chaudhary ES, Shah N, Vyas N, Comparative study of myofascial release and cold pack in upper trapezius spasmInt J Health Sci Res 2013 3(12):20-27. [Google Scholar]
[18]. Ajimsha MS, Chithra S, Pillai Thulasyammal R, Effectiveness of myofascial release in the management of lateral epicondylitis in computer professionalsArch Phys Med Rehabil 2012 93(4):604-09.10.1016/j.apmr.2011.10.01222236639 [Google Scholar] [CrossRef] [PubMed]
[19]. Kain J, Martorello L, Swanson E, Sego S, Comparison of an indirect tri-planar myofascial release (MFR) technique and a hot pack for increasing range of motionJ Bodyw Mov Ther 2011 15(1):63-67.10.1016/j.jbmt.2009.12.00221147420 [Google Scholar] [CrossRef] [PubMed]
[20]. Renan-Ordine R, Alburquerque-Sendín F, Rodrigues de Souza DP, Cleland JA, Fernández-de-Las-Peñas C, Effectiveness of myofascial trigger point manual therapy combined with a self-stretching protocol for the management of plantar heel pain: A randomized controlled trialJ Orthop Sports Phys Ther 2011 41(2):43-50.10.2519/jospt.2011.350421285525 [Google Scholar] [CrossRef] [PubMed]
[21]. Tozzi P, Bongiorno D, Vitturini C, Fascial release effects on patients with non-specific cervical or lumbar painJ Bodyw Mov Ther 2011 15(4):405-16.10.1016/j.jbmt.2010.11.00321943614 [Google Scholar] [CrossRef] [PubMed]
[22]. Kalamir A, Pollard H, Vitiello A, Bonello R, Intra-oral myofascial therapy for chronic myogenous temporomandibular disorders: A randomized, controlled pilot studyJ Man Manip Ther 2010 18(3):139-46.10.1179/106698110X1264074071237421886424 [Google Scholar] [CrossRef] [PubMed]
[23]. Aguilera FJM, Martín DP, Masanet RA, Botella AC, Soler LB, Morell FB, Immediate effect of ultrasound and ischemic compression techniques for the treatment of trapezius latent myofascial trigger points in healthy subjects: A randomized controlled studyJ Manipulative Physiol Ther 2009 32(7):515-20.10.1016/j.jmpt.2009.08.00119748402 [Google Scholar] [CrossRef] [PubMed]
[24]. Kuhar S, Khatri KS, Jeba C, Effectiveness of myofascial release in the treatment of plantar fasciitis: A RCTIndian Journal of Physiotherapy and Occupational Therapy-An International Journal 2007 1(3):03-09. [Google Scholar]
[25]. Hsieh CYJ, Adams AH, Tobis J, Hong CZ, Danielson C, Platt K, Effectiveness of four conservative treatments for subacute low back pain: A randomized clinical trialSpine (Phila Pa 1976) 2002 27(11):1142-48.10.1097/00007632-200206010-0000312045509 [Google Scholar] [CrossRef] [PubMed]
[26]. Barnes MF, Gronlund RT, Little MF, Personius WJ, Efficacy study of the effect of a myofascial release treatment technique on obtaining pelvic symmetryJournal of Bodywork and Movement Therapies 1997 1(5):289-96.10.1016/S1360-8592(97)80064-2 [Google Scholar] [CrossRef]
[27]. Hanten WP, Chandler SD, Effects of myofascial release leg pull and sagittal plane isometric contract-relax techniques on passive straight-leg raise angleJ Orthop Sports Phys Ther 1994 20(3):138-44.10.2519/jospt.1994.20.3.1387951290 [Google Scholar] [CrossRef] [PubMed]