Peritonitis is one of the most commonly encountered acute surgical problems that a surgeon has to face. Peritonitis due to hollow viscus perforation has a high mortality rate in spite of advances in the surgical treatment. Early prognostic evaluation of peritonitis is important to select patients who will require an aggressive management for optimum outcome [1,2].
Various scoring systems have been used to indicate prognosis of patients with peritonitis [3-5]:
The presence of organ failure is assessed as per criterion published by Deitch EA [6] in 1992:
APACHE II is a disease independent scoring system used most commonly in ICU settings. MPI on the other hand is disease specific scoring system. APACHE II has a greater number of variables than MPI which makes it more time consuming and cumbersome calculation when compared to MPI which is relatively simple to calculate and less time consuming. In emergency settings, time is an important factor. So, we need a scoring system which is easy, less time consuming and also precise in assessing prognosis of the disease. Few studies in the past conducted by Kumar P et al., Fugger R et al., have indicated that MPI may be comparable or even better than APACHE II in emergency setting [7,8]. This study was done to find out efficacy of MPI in comparison to APACHE II to prognosticate perforation peritonitis.
Materials and Methods
This prospective observational study from November 2015 till March 2017 was conducted at Department of General Surgery, ABVIMS and Dr. Ram Manohar Lohiya Hospital, New Delhi, India.
Inclusion criteria: 63 patients above 18 years of age presenting with perforation peritonitis were included.
Exclusion criteria: Patients with perforation peritonitis secondary to abdominal trauma, primary peritonitis and postoperative peritonitis due to anastomosis leak were excluded from the study. Ethical committee clearance was taken. {No.T. P(MD/MS) (42/2015)/IEC/PGIMER/RML/4945} Dt. 26.10.2015. Appropriate patient Consent was taken in each case.
Sample size was calculated and considered according to the previous study with p=5% [9] and d=absolute error of 5%. All the patients in preoperative phase were adequately resuscitated, broad spectrum antibiotic (inj. Ceftriaxone 1gm I.V.) prophylaxis was given, Arterial Blood Gases (ABG) and serum electrolytes were checked and if any abnormality was found, it was corrected, Foley’s and Ryles tube catheterisation was done, pulse and BP charting was done, parts preparation done just before induction of anaesthesia and then were subjected to emergency surgery. Outcome of patients was studied in terms of postoperative wound infection; wound dehiscence assessed clinically, anastomotic leak, respiratory complications, duration of hospital stay, need of ventilator support and mortality. MPI score [Table/Fig-2] was calculated in all the patients and compared with APACHE II score (as a standard).
According to MPI score, patients were divided into Low risk 0-21, Moderate risk >21-29 and High risk >29. Patients were divided into Low risk <10, Moderate risk >11-20 and High risk >20 as per APACHE II score.
Statistical Analysis
Statistical analysis was done using statistical software package SPSS v22.0. Data were represented as mean±SD. Continuous variables were compared using t-test and ROC plotting was done to predict the critical value. Correlation between two continuous variables was established using Pearson’s correlation coefficient. The p-value <0.05 was taken as significant.
Results
Of the 63 patients, 50 were males and 13 were females. Mean age of male subjects (37.4 years) and female subjects (38.5 years). Total of 69.8% (44 patients) had wound infection, 42.9% (27 patients) had respiratory complications, 33% (21 patients) had wound dehiscence, 30% (19 patients) required ventilatory support, 7.9% (5 patients) had anastomotic leak and 19% (12 patients) died in the postoperative period [Table/Fig-3].
Frequency of all outcome variables.
| Serial number | Postoperative consequences | Frequency (%) |
|---|
| 1 | Wound infection | 44 (69.8%) |
| 2 | Wound dehiscence | 21 (33.3%) |
| 3 | Respiratory complications | 27 (42.9%) |
| 4 | Ventilatory support | 19 (30.2%) |
| 5 | Anastomotic leakage | 5 (7.9%) |
| 6 | Death | 12 (19%) |
The mean APACHE II score was 11.2±8.1 with range of 0 to 35. The mean MPI score was 26.9±7.2 with range of 6 to 39 [Table/Fig-4].
Frequency distribution of patients according to APACHE II and MPI score.
| APACHE II score | No. of patients | MPI score | No. of patients |
|---|
| <10 | 34 | <21 | 10 |
| >10-20 | 21 | >21-29 | 31 |
| >20 | 8 | >29 | 22 |
The postoperative morbidity and mortality were calculated according to APACHE II scoring [Table/Fig-5a,b] and MPI scoring [Table/Fig-6a,b]. APACHE II was able to predict postoperative respiratory complications, postoperative need for ventilatory support, hospital stay duration and mortality; while MPI was able to predict postoperative respiratory complications, postoperative need for ventilatory support and mortality. Neither APACHE II nor MPI could predict postoperative anastomotic leak, postoperative wound infection, and postoperative wound dehiscence.
Comparison of postoperative morbidity according to APACHE II scoring.
| Postoperative complications | APACHE II score | Total | Pearson’s chi-square | p-value |
|---|
| 0-10 | 11-20 | 21 or more |
|---|
| Postoperative Wound Infection | No | 10 | 7 | 2 | 19 | 1.347 | 0.510 |
| Yes | 28 | 10 | 6 | 44 |
| Total | 38 | 17 | 8 | 63 | | |
| Wound dehiscence | No | 28 | 10 | 4 | 42 | 2.313 | 0.315 |
| Yes | 10 | 7 | 4 | 21 |
| Total | 38 | 17 | 8 | 63 | | |
| Respiratory complication | No | 29 | 6 | 1 | 36 | 15.528 | <0.001*** |
| Yes | 9 | 11 | 7 | 27 |
| Total | 38 | 17 | 8 | 63 | | |
| Ventilatory support | No | 34 | 8 | 2 | 44 | 18.780 | <0.001*** |
| Yes | 4 | 9 | 6 | 19 |
| Total | 38 | 17 | 8 | 63 | | |
| Anastomotic leak | No | 35 | 15 | 8 | 58 | 1.031 | 0.597 |
| Yes | 3 | 2 | 0 | 5 |
| Total | 38 | 17 | 8 | 63 | | |
| Mortality | No | 34 | 14 | 3 | 51 | 11.607 | 0.003** |
| Yes | 4 | 3 | 5 | 12 |
| Total | 38 | 17 | 8 | 63 | | |
**Moderately significant; ***Highly significant
Correlation of APACHE II with hospital stay duration.
| APACHE II score | Duration of hospital stay |
|---|
| APACHE II score | Pearson correlation | 1 | 0.249 |
| Sig. (2-tailed) | | 0.049 |
| N | 63 | 63 |
The mean post hospital duration was 9.4 days with range of 1 to 30 days; Correlation is significant at the 0.05 level (2-tailed)
Comparison of postoperative morbidity according to MPI scoring.
| Postoperative complications | MPI score | Total | Pearson’s chi-square | p-value |
|---|
| 0-20 | 21-29 | 30 or more |
|---|
| Post operative wound infection | No | 5 | 7 | 7 | 19 | 2.743 | 0.254 |
| Yes | 5 | 24 | 15 | 44 |
| Total | 10 | 31 | 22 | 63 | | |
| Wound dehiscence | No | 9 | 21 | 12 | 42 | 3.921 | 0.141 |
| Yes | 1 | 10 | 10 | 21 |
| Total | 10 | 31 | 22 | 63 | | |
| Respiratory complication | No | 9 | 20 | 7 | 36 | 10.858 | 0.004** |
| Yes | 1 | 11 | 15 | 27 |
| Total | 10 | 31 | 22 | 63 | | |
| Ventilatory support | No | 10 | 25 | 9 | 44 | 14.779 | 0.001** |
| Yes | 0 | 6 | 13 | 19 |
| Total | 10 | 31 | 22 | 63 | | |
| Anastomotic leak | No | 9 | 30 | 19 | 58 | 1.978 | 0.372 |
| Yes | 1 | 1 | 3 | 5 |
| Total | 10 | 31 | 22 | 63 | | |
| Mortality | No | 10 | 27 | 14 | 51 | 7.390 | 0.025* |
| Yes | 0 | 4 | 8 | 12 |
| Total | 10 | 31 | 22 | 63 | | |
*Significant; **Moderately significant
Correlations of hospital stay with MPI score.
| Duration of hospital stay | MPI score |
|---|
| Duration of stay | Pearson correlation | 1 | .211 |
| Sig. (2-tailed) | | .098 |
| N | 63 | 63 |
The mean MPI score has no correlation with hospital stay; (Pearson’s correlation coefficient=0.211; p-value >0.05)
Chi-square analysis of MPI as well as APACHE II score severity grading showed that there is increased risk of respiratory complications, need of ventilator support and mortality with increase in both the scores [Table/Fig-5,6].
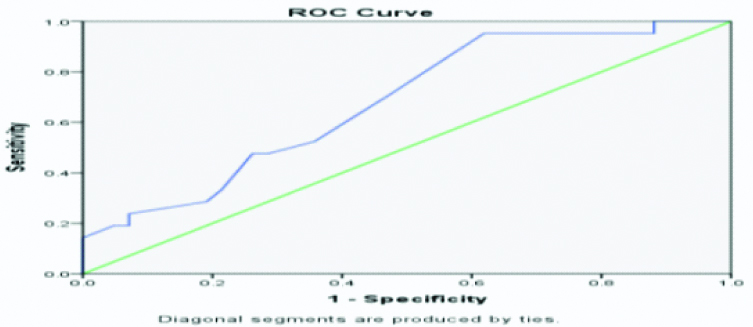
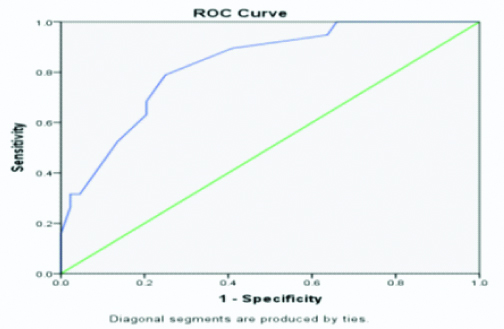
ROC curve analysis suggests that cut-off value of MPI >26.5 can predict the postoperative wound dehiscence with 71.4% sensitivity and 52.4% specificity [Table/Fig-7].
ROC curve of MPI score for Postoperative wound dehiscence.
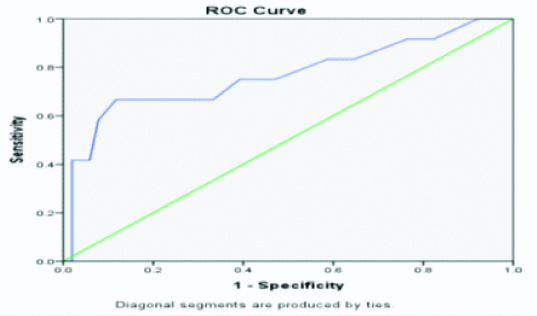
ROC curve analysis suggests that cut-off value of APACHE II >9.5 can predict the postoperative respiratory complications with 70.4% sensitivity and 72.8%, specificity [Table/Fig-8a].
ROC curve of APACHE II score for Postoperative respiratory complications.
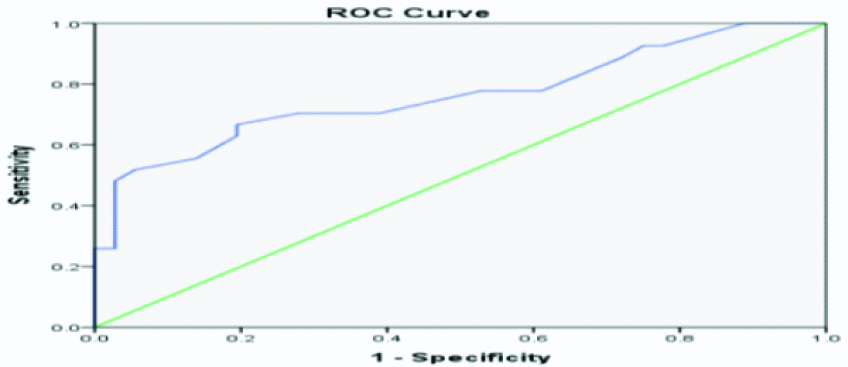
ROC curve analysis suggests that cut-off value of MPI >26.5 can predict the postoperative respiratory complications with 81.5% sensitivity and 64.0% specificity [Table/Fig-8b].
ROC curve of MPI score for postoperative respiratory complications.
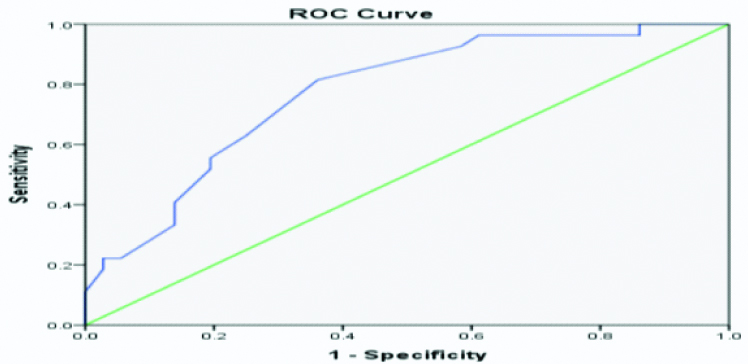
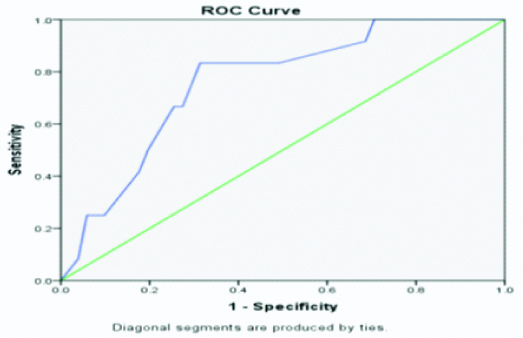
ROC curve analysis suggests that cut-off value of APACHE II >9.5 can predict the postoperative need of ventilation support with 84.2% sensitivity and 70.5% specificity [Table/Fig-9a].
ROC curve of APACHE II score for postoperative ventilator support.
ROC curve analysis suggests that cut-off value of MPI >28.0 can predict the postoperative need of ventilation support with 78.9% sensitivity and 75.0% specificity [Table/Fig-9b].
ROC curve of MPI score for postoperative need of ventilatory support.
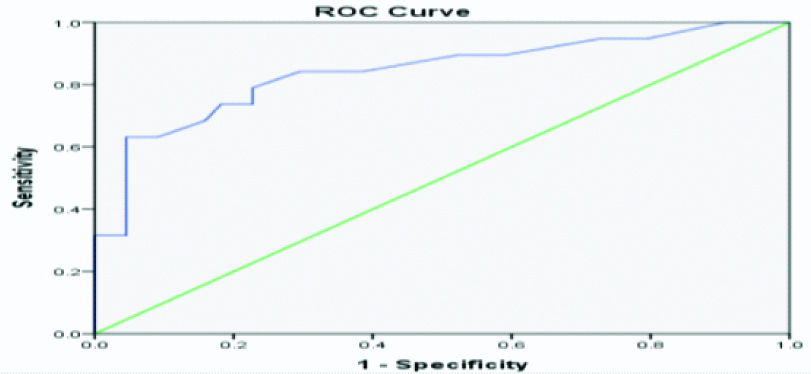
ROC curve analysis suggests that cut-off value of APACHE II >9.5 can predict the postoperative mortality with 75.0% sensitivity and 60.8% specificity [Table/Fig-10a].
ROC curve of APACHE II score for postoperative mortality.
ROC curve analysis suggests that cut-off value of MPI >28.0 can predict the postoperative mortality with 83.3% sensitivity and 68.6% specificity [Table/Fig-10b].
ROC curve of MPI score for postoperative mortality.
Discussion
In this study, MPI score was used to prognosticate patients of perforation peritonitis. APACHE II score was used as a standard score against which the findings of MPI score were compared. APACHE II was able to predict postoperative respiratory complications (p<0.001), postoperative need for ventilatory support (p<0.001), hospital stay duration and mortality (p<0.004) while MPI was able to predict postoperative respiratory complications (p<0.001), postoperative need for ventilatory support [p<0.001] and mortality (p<0.006).
Increase in APACHE II and MPI score did not increase the risk of postoperative wound infection. Inamdar MF and Naresh KL assessed the effectiveness of MPI in predicting the morbidity and mortality in perforation peritonitis and found that 5.8% of patients with MPI score less than 21 developed wound infection while 41.4% of patients had wound infection with MPI score 21 to 27 [10]. They found this outcome to be statistically insignificant.
Postoperative wound dehiscence did not show any correlation with increase in MPI and APACHE II score. Kalra D et al., compared APACHE II with various morbidities and found that postoperative wound dehiscence was statistically insignificant [11]. Muralidhar VA et al., assessed the effectiveness of MPI in Perforation peritonitis and found wound dehiscence was seen in only 4% cases [12]. Postoperative respiratory complications showed statistically significant correlation with increasing MPI and APACHE II score. Patil VA et al., found that high risk group (MPI>29) has more respiratory complications than intermediate (MPI 21 to 29) and low risk group (MPI <21) [13].
Increase in MPI score had no effect on postoperative hospital stay while increase in APACHE II score increased the postoperative hospital stay. Increase in severity of both APCHE II and MPI increased the risk of postoperative ventilatory support requirement. Ahuja A and Pal R found the mean ICU stay of 9.75 days in patients with APACHE II score more than 20 compared to 0.13 days ICU stay in patients having APACHE II score less than 10 (mean hospital stay was 12 days) [14]. Postoperative anastomotic leak did not show any statistical significance with increasing MPI and APACHE II score in the present study.
In this study, twelve out of sixty-three patients died (19%). The high mortality could be attributed to patients presenting late. All patients who presented within 24 hours after onset of symptoms recovered postoperatively and were discharged. However, 12 out of 47 patients who presented >24 hours after onset of symptoms could not survive due to sepsis and Multiple Organ Dysfunction Syndrome. Increase in both APACHE II and MPI increased the risk of postoperative mortality which was statistically significant. Kumar P et al., compared MPI and APACHE II in predicting the outcome in patients of peritonitis and found no significant difference between MPI and APACHE II in predicting the mortality [7].
Limitation(s)
In this study, there was no case of malignant aetiology and only one patient had chronic obstructive pulmonary disease. The impact on preoperative score and final outcome therefore could not be assessed. Multicentric studies with large sample size may alleviate this issue.
Conclusion(s)
Both APACHE II and MPI scores are equally good in predicting the outcomes of perforation peritonitis. MPI is easy to apply but it does not consider underlying physiological disturbances. It also needs operative findings so in true sense; it cannot be used as a preoperative scoring system. This hampers its use to stratify patients into groups to decide whether definitive surgery or damage control surgery can be carried out safely. On the other hand, APACHE II can be calculated preoperatively to categorise patients but it does not take into account peritoneal contamination which has a huge bearing on the final outcome. It is worthwhile to use combination of both scores for a superior prediction of mortality in patients of perforation peritonitis.
Declaration: This article was submitted to Scientific Session of the 16th World Congress of Endoscopic Surgery, Jointly Hosted by Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) and Canadian Association of General Surgeons (CAGS), Seattle, Washington, USA, 11-14 April 2018 for poster presentation and was later accepted, but it was never presented.
**Moderately significant; ***Highly significant
The mean post hospital duration was 9.4 days with range of 1 to 30 days; Correlation is significant at the 0.05 level (2-tailed)
*Significant; **Moderately significant
The mean MPI score has no correlation with hospital stay; (Pearson’s correlation coefficient=0.211; p-value >0.05)