Solitary Prostatic Urethral Carcinoma: Cryptic cause of Acute Urinary Retention
Mayank Jain1, Abhishek Umesh Bhalerao2, M Shivalingaiah3, Navaneeth R Srinidhi4, Pramod Adiga5
1 Assistant Professor, Department of Urology, Institute of Nephrourology, Bengaluru, Karnataka, India.
2 Resident Doctor, Department of Urology, Institute of Nephrourology, Bengaluru, Karnataka, India.
3 Professor, Department of Urology, Institute of Nephrourology, Bengaluru, Karnataka, India.
4 Assistant Professor, Department of Urology, Institute of Nephrourology, Bengaluru, Karnataka, India.
5 Assistant Professor, Department of Urology, Institute of Nephrourology, Bengaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Mayank Jain, Department of Urology, Institue of Nephrourology, Victoria Hospital Campus, K R Market, Bengaluru, Karnataka, India.
E-mail: ricky_bjpune@yahoo.com
Acute Urinary Retention (AUR) caused by urological malignancy is a rare event, even in elderly. A solitary prostatic urethral Transitional Cell Carcinoma (TCC) causing retention of urine is even rarer. Hereby, a case of 60-year-old non-smoker, with sudden onset of AUR was reported. Detailed clinical examination, biochemical and radiological investigations were not conclusive. Cystoscopy revealed a solitary papillary prostatic urethral growth projecting from base probably causing urinary retention. Histopathology confirmed it as a low grade urothelial carcinoma. Patient voided well after complete transurethral resection. Hence, an urothelial malignancy can have varied presentation, and appropriate histological diagnosis with cross-sectional imaging and regular follow-up with cystoscopy is mandatory.
Isolated, Low grade, Prostatic urethra, Urothelial carcinoma
Case Report
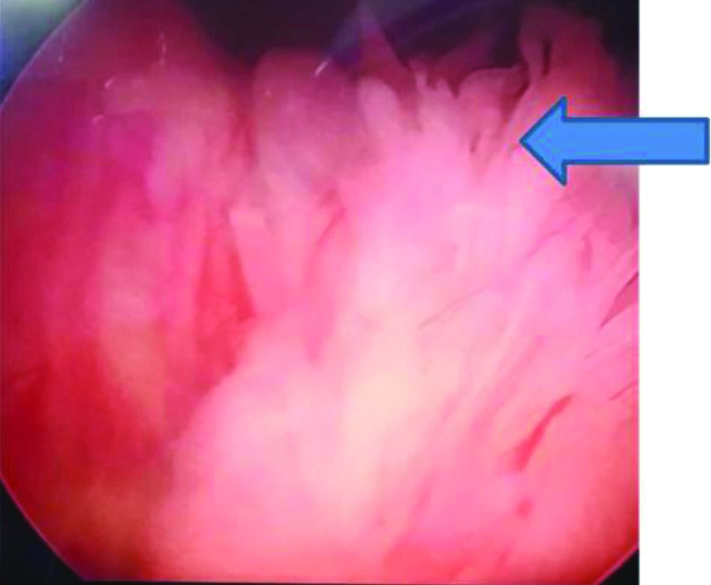
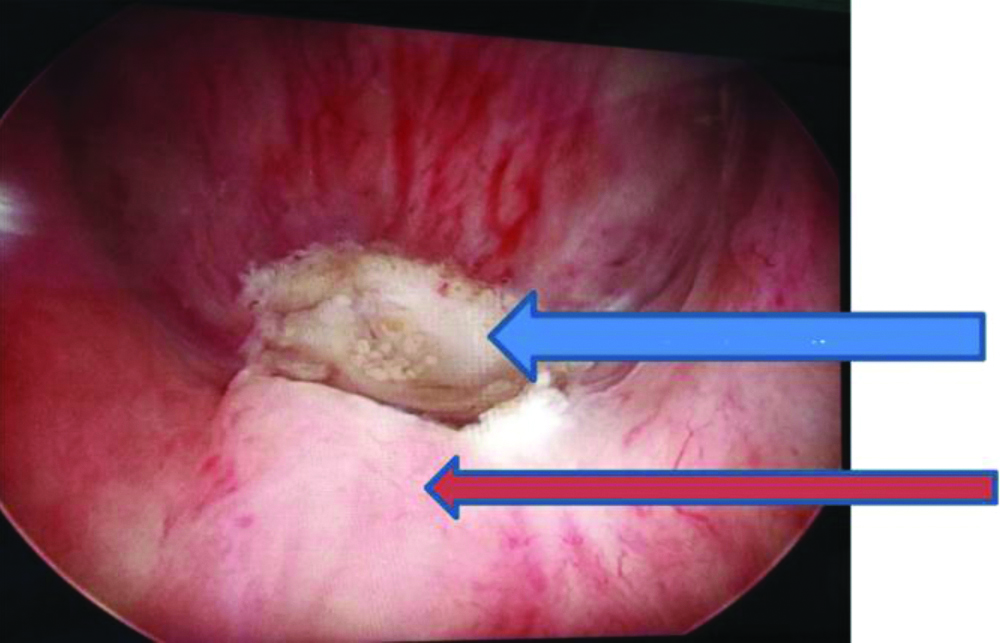
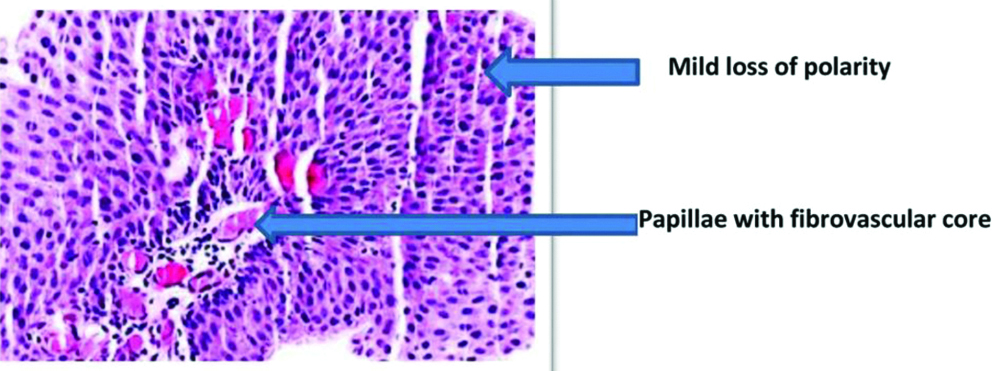
A 60-year-old male came with chief complaint of AUR since one week and was in per urethral catheter. There was no history of Lower Urinary Tract Symptoms (LUTS), haematuria, abdominal pain, constipation. Patient was non-diabetic, non-alcoholic, non-smoker and no history of any surgical intervention in past. On examination, he was moderate in built and nourished with BMI of 23.6 Kg/ m2. Systemic examination was normal. Per rectal examination revealed Grade 1 firm prostate as per Barnes per rectal grading [1]. Biochemical investigations and urine analysis were well within normal limits. Ultrasonography revealed 25 cc prostate and no features suggesting bladder outlet obstruction. Patient was given trial void after one week course of alpha blocker, but failed. Subsequently patient underwent urodynamic evaluation which suggested bladder outlet obstruction. On cystoscopy surprisingly a 3 cm isolated papillary mobile growth was seen in prostatic urethra from 5 to 7 o’clock arising just proximal to verumontanum encroaching bladder neck without involving it [Table/Fig-1,2]. No other synchronous lesions were found in bladder and bladder mucosa was normal. Complete transurethral resection was done and it revealed low grade papillary urothelial neoplasm [Table/Fig-3]. CT Urogram and metastatic workup notified no other abnormality. On 1 year regular follow-up with cystoscopy and CT urogram, patient is symptom free and voiding well.
Cystoscopy of prostatic urethral carcinoma showing 3 cm papillary growth in prostatic urethra (blue arrow).
Cystoscopy: Small growth seen proximal to verumontanum after resection.
Red arrow- verumontanum and Blue arrow- growth
Histopathology revealing low grade urothelial carcinoma (papillae with fibrovascular core, mild loss of cell polarity and occasional mitosis). (200x magnification H&E stain).
Discussion
Retention of urine can be spontaneous or precipitated that is following a cause. Spontaneous AUR in elderly is a common urological emergency with benign prostatic hyperplasia accounting for most of the cases followed by stricture urethra, neurogenic bladder or urethral calculus; carcinoma prostate, prostatic abscess, carcinoma bladder being rarer diagnosis [2]. A precipitated AUR is secondary to some inciting event like hernia or haemorrhoid surgery, drugs etc.
Urological malignancies causing AUR is rarely encountered. Urothelial carcinoma of bladder, upper tract or highly vascular renal cell carcinoma with involvement of pelvicalyceal system or secondary trauma can cause AUR or clot retention [2]. To the best of knowledge, isolated prostatic urethral growth causing AUR has not been reported, so far in literature. Generally, prostatic urethral carcinoma is seen in conjugation with primary bladder cancer or it can be metastatic involvement of carcinoma prostate [3]. The growth can be benign or malignant which includes differential diagnosis of cystitis cystica, cystitis glandularis, urethral polyp, schistosomiasis, tuberculosis, urothelial carcinoma, squamous cell carcinoma [4].
Prostatic urethral carcinoma is observed in 15-48% of radical cystectomy specimens, performed for carcinoma bladder. Multifocality, carcinoma in situ, bladder neck or trigonal tumour is the risk factors for prostatic involvement in bladder tumour [5]. Distinctly in index case, none of the risk factors was seen. Degree of involvement can include acini, ducts, urethral mucosa, and stroma of the gland, which has been shown to affect the outcome [6]. It can present as asymptomatic entity, haematuria, Lower Urinary Tract Symptoms (LUTS), urinary retention or features of advanced disease.
Primary TCC of the prostatic urothelium is rare, occurring in 1-4% of patients, but development of TCC in the PU during follow-up of bladder cancer patients are more common [6]. Once the diagnosis of urothelial malignancy is suspected, patient needs to undergo detailed history taking including smoking history and history of risk factors, clinical examination, complete blood count, renal function tests, coagulation profile, CT Urogram and subsequent transurethral resection of tumour. Disease needs to be stratified as low or high grade and TNM staging should be done. In cases of localised muscle invasive disease radical Cystoprostatectomy is gold standard. T1 lesions can be followed as per strict protocol with cystoscopy and urine cytology. Intravesical therapy with Bacillus Calmette-Guerin (BCG) immunotherapy is an alternative treatment in prostatic urethral involvement [7]. Metastatic disease carries a dismal prognosis in view of renal failure, obstructive uropathy, uremic encephalopathy, anaemia, cancer cachexia. Chemotherapy, urinary diversion and palliative treatment remain the mainstay of treatment in advanced disease.
Conclusion(s)
Urothelial malignancy once diagnosed in urinary tract needs extensive evaluation and strict adherence to follow-up protocol. Low grade cancer can be treated with regular cystoscopy and transurethral resection of bladder tumour and high grade cancers need definitive surgery. Diagnosis of prostatic urethral TCC should also be considered while evaluating a case of AUR.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 27, 2020
Manual Googling: May 18, 2020
iThenticate Software: May 28, 2020 (5%)
[1]. Barnes RW, Bergman RT, Hadley HL, Alken CE, Andersson L, Endoscopy 1959 1st edNew YorkSpringer:15410.1007/978-3-642-86571-8 [Google Scholar] [CrossRef]
[2]. Selius BA, Subedi R, Urinary retention in adults: Diagnosis and initial managementAm Fam Physician 2008 77(5):643-50. [Google Scholar]
[3]. Celestino F, Verri C, De Carlo F, Zampa G, Pagliarulo V, Mauro Di Stasi FMS, Urothelial carcinoma of the prostatic urethra: Long-term follow-up studyJournal of Clinical Oncology 2015 33(15):e1563910.1200/jco.2015.33.15_suppl.e15639 [Google Scholar] [CrossRef]
[4]. Campbell Walsh Urology. 11th International Edition 2016 by Elsevier Inc. Chapter 93-Non-muscle Invasive Bladder Cancer. Page 2206-23 [Google Scholar]
[5]. Canda AE, Tuzel E, Mungan MU, Yorukoglu K, Kirkali Z, Conservative management of mucosal prostatic urethral involvement in patients with superficial transitional cell carcinoma of the bladderEuropean Urology 2004 45(4):465-69.discussion 469-7010.1016/j.eururo.2003.12.01415041110 [Google Scholar] [CrossRef] [PubMed]
[6]. Knoedler JJ, Boorjian SA, Tollefson MK, Cheville JC, Thapa P, Tarrell RF, Urothelial carcinoma involving the prostate: The association of revised tumour stage and coexistent bladder cancer with survival after radical cystectomyBJU Int 2014 114(6):832-36.10.1111/bju.1248624119219 [Google Scholar] [CrossRef] [PubMed]
[7]. Kirkali Z, Canda EA, Superficial urothelial cancer in the prostatic urethraThe Scientific World Journal 2006 6:2603-10.10.1100/tsw.2006.40217619737 [Google Scholar] [CrossRef] [PubMed]