It is notable that evidence-based research has been used to confirm the significance of the PDR. Results have shown adequate PDR leads to higher patient satisfaction, symptom elimination, and more acceptable treatment compliance [1,2]. According to past studies, the relationships established between the health care provider; for example, physicians and patients is one of the crucial components of the delivery of health services [3]. According to the results obtained during the last 40 years, PDR contributes effectively to delivering the high-quality patient-centered health care [4].
Communication and interaction skills are two essential traits all doctors require. These are essential qualities apart from the professional character of every physician [5]. Patient’s communication skills are also equally important because the patient is an important part of the health system [6]. Moreover, establishing an effective relationship with the patients, their families and caregivers is of special importance for obtaining comprehensive output for patient treatment outcomes [7].
Thus, if a doctor communicates with a patient, he would not only gain knowledge about the patient’s problems but also create a therapeutic relationship crucial to manage the disease and its treatment [8]. Another main parameter affecting the care effectiveness is the quality of the PDR. Reasonable PDR correlates with the increased satisfaction of the patients and more acceptable agreements [9]. Communication skills also include abilities for conveying information to one another effectively and efficient communication would combine various skills such as non-verbal communications, emotion management, attentive listening, capability of making trust and respect, and common decisions [10].
One of the studies identified communication as the most significant parameter to determine the patients’ agreement to the therapeutic options, which would develop naturally over time and with experience [11]. Analysis of patients’ complaints with regard to doctors indicates that most of the complaints relate to poor communication and interpersonal skills [12]. According to some studies, optimisation of the PDR may result in more reasonable patient health and outcomes, in particular, in the primary care [13,14].
Any deficiency in communications is related to the negative experiences of patients, medical errors, and professional misconduct, in particular, in the primary care service [15]. However, other studies have indicated that an unsuitable interaction between patients and doctors is a factor involved in patient disagreements [16,17].
For example, Osterberg L and Blaschke T summarised the barriers under the three inter-dependent factors associated with patient, doctor, and the health care systems. The researchers strongly emphasised on the patients’ poor understanding of the diseases, advantages of treatment and hazards of disagreement [18]. Thus, the PDR is a strong indicator of the health care qualities, which may detect the patient’s self-management behaviors and health consequences [19]. A PDR has in fact been considered as one of the most vital factors in the health care centers that influences the course of patients cares and patient’s agreement with the treatments advised [19].
Thus, the connection between the physician and the patients’ care-givers is of high significance in all steps of health center services management [6]. Thus, this research aimed at the evaluation of the reliability and validity of the Persian version of the PDR Questionnaire (PDRQ-9) in the Iranian population in the primary health center.
Materials and Methods
According to the research design, primary health centres affiliated to Iran University of Medical Sciences were selected to conduct this methodological research between March and May 2019. The Ethics Committee of Iran University of Medical Sciences approved this research (IR.IUMS.REC.1397.655).
Study population of the research included all individuals, who wanted to get health services from the doctors, referred to the health centres situated at Tehran, Iran between March and May 2019. Inclusion criteria for choosing participants were their willingness to participate in the research and essential communication skills. Patients apprehensive about participation in the study were excluded. Thus, 208 patients who fulfilled the inclusion criteria were randomly selected.
Accordingly, each participant was informed of the research goals and methods. In addition, they were assured of voluntary participation. Moreover, they were ensured that their data would be confidential. Written consents were obtained from each participant.
In order to collect the required data, we distributed a demographic questionnaire containing items such as gender, age and educational status; and the PDRQ-9 [20] among the participants.
A forward-backward translation method was utilised for translating the scale from Persian to English and back to Persian. We invited two English-Persian translators for providing an independent translation of the PDRQ-9. Finally, an expert panel involving the present research and both translators, evaluated and integrated both translations and formulated a single Persian translation of PDRQ-9. PDRQ-9 included nine items scored on a five-point scale from 1 (not at all appropriate) to 5 (totally appropriate) [20].
Since more than 20% of the participants were not sufficiently educated (i.e., illiterates or beginners), the items were translated to them by a trained assistant expert for recording their responses.
Face and Content Validity
Face validity was assessed by study participants and received an acceptable impact score. In the assessment of face validity, for each question the five-part spectrum was used. The impact factor of all questions was higher than 1.5, which was an acceptable value. Content validity was also evaluated with the approval of six experts and obtained an acceptable score based on the Lawshe tab (99% and above 99%). Six experts examined the questions; each question was examined based on a three-part spectrum. The value of content validity ratio for all questions was equal to 1.
Construct Validity Assessment
In order to evaluate construct validity of the questionnaire, an Exploratory Factor Analysis (EFA) with the method of PCA were used to examine the factor structure of the Persian PDRQ-9 via a PCA accompanied by a varimax rotation using SPSS 22 (SPSS Inc., Chicago, IL, USA). The minimum sample size for conducting the factor analysis should be 5 to 10 times greater than the number of the items in questionnaire [17]. Therefore, a sample size of 208 respondents was deemed sufficient to provide a more than adequate participant/item ratio. The research participants were invited for completing the Persian PDRQ-9.
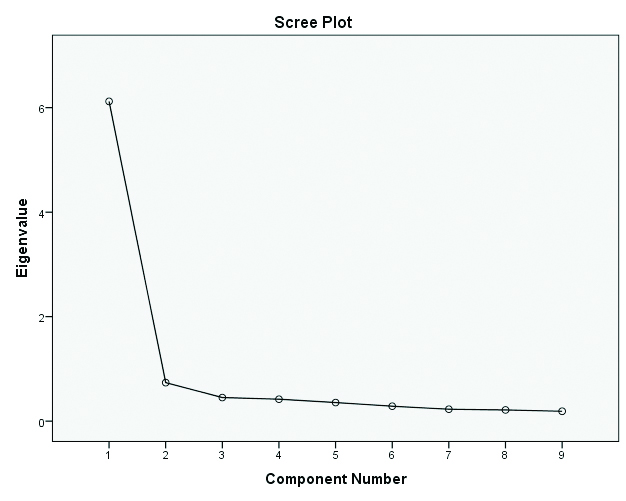
In order to examine the sample and factor analysis adequacy, we applied Bartlett’s and Kaiser-Meyer-Olkin (KMO) tests. The numbers of the factors were specified on the basis of Eigenvalues and scree plot so that items with absolute loading values equal to 0.4 or more, were treated as suitable items [13]. Then, CFA was used to confirm and validate PCA outputs. Afterwards, a CFA run with AMOS 19 was for examining the factor structure achieved from the EFA. Finally, the most popular indices of goodness of fit model in CFA: Root Mean Square Error of Approximation (RMSEA), χ2 goodness-of-fit index, the Normed Fit Index (NFI), Parsimonious Comparative Fit Index (PCFI), Adjusted Goodness of Fit Index (AGFI) and Chi-square divided by Degrees of Freedom value (CMIN/DF) were run on the software [18,21].
It is notable that when developing and validating scales, EFA and CFA are among statistical methods employed for studying the factor structure. In fact, EFA should be applied at the initial phases of instrument formulation as it aims at finding the latent variables underlying the scale [22]. In other words, CFA is utilised for testing the fit of a prior hypothesised structure of the scale and hence, it is beneficial in the later phases of the instrument formulation because it is a robust statistical tool for determining if the introduced factor structure may sufficiently fit the data or not (goodness of fit) [23]. [Table/Fig-1] reports the cut-off criteria of the model fit indicators for the latent variable models [21].
Cut-off criteria for several fit indices Bentler PM and Bonett DG [21].
| Indices | Acceptable fit |
|---|
| Chi-squared p-value | >0.05 |
| PCFI | >0.5 |
| PNFI | >0.5 |
| AGFI | >0.8 |
| RMSEA | Good<0.08, moderate<0.08-0.1 |
| CMIN/DF | Good<3, acceptable<5 |
Reliability Evaluation
According to the research design, reliability of the Persian PDRQ-9 had been initially evaluated via assessing its internal consistency and computing the Cronbach’s alpha. Alpha values ≥0.7 represent acceptable internal consistency [21].
Results
According to the data obtained, the average age of the patients {n=208; 109 females (52.4%); 99 males (47.6%)} was 35 years (SD=12.24). In addition, most heads of household were employed (86.5%). 21.6% of patients had a university (Academic education) degree, 57.2% of patients were diploma and sub-diploma holders and 21.2% of patients had primary education or were illiterates.
Results of the current study showed that the PDRQ-9 reliability was 0.94 and mean score of PDRQ-9 was 3.61 (SD=1.10). According to the findings, items q2 and q5 exhibited the maximum and minimum average of 3.99 (SD=1.12) and 3.01 (SD=1.52), respectively [Table/Fig-2]. Moreover, correlation between items was found to be satisfactory in the range between 0.46 and 0.78 [Table/Fig-3].
Mean±SD of the item features of PDRQ-9.
| PDRQ-9 | Mean±SD | Total correlation of the corrected item | Cronbach’s alpha if item deleted |
|---|
| q1 | 3.82±1.27 | 0.700 | 0.937 |
| q2 | 3.99±1.12 | 0.718 | 0.936 |
| q3 | 3.57±1.33 | 0.821 | 0.930 |
| q4 | 3.61±1.31 | 0.820 | 0.930 |
| q5 | 3.01±1.52 | 0.755 | 0.935 |
| q6 | 3.65±1.29 | 0.736 | 0.935 |
| q7 | 3.54±1.46 | 0.764 | 0.934 |
| q8 | 3.74±1.32 | 0.819 | 0.930 |
| q9 | 3.60±1.39 | 0.821 | 0.930 |
| Mean score | 3.61±1.10 | |
Inter-item correlation of PDRQ-9.
| Inter-item correlation matrix* |
|---|
| q1 | 1 | | | | | | | | |
| q2 | 0.732 | 1 | | | | | | | |
| q3 | 0.597 | 0.632 | 1 | | | | | | |
| q4 | 0.622 | 0.642 | 0.773 | 1 | | | | | |
| q5 | 0.556 | 0.556 | 0.665 | 0.677 | 1 | | | | |
| q6 | 0.535 | 0.604 | 0.647 | 0.599 | 0.622 | 1 | | | |
| q7 | 0.460 | 0.495 | 0.672 | 0.668 | 0.662 | 0.606 | 1 | | |
| q8 | 0.625 | 0.584 | 0.679 | 0.700 | 0.624 | 0.632 | 0.742 | 1 | |
| q9 | 0.590 | 0.564 | 0.727 | 0.706 | 0.637 | 0.648 | 0.725 | 0.784 | 1 |
*All item p-value <0.01
Furthermore, principal factor analysis with varimax rotation was run for assessing the basic structure scree plot for the nine items of PDRQ-9 [Table/Fig-4]. According to varimax rotation, one item loaded and the factor justified 68.01% of the rotation variance. [Table/Fig-5] represents the items and factor loadings for the rotated factor.
Scree plot structure for the nine items of PDRQ-9.
Exploratory factor loading of the items in the PDRQ-9 with one factor.
| Factor | Items | Loading | % of variance | Eigenvalues |
|---|
| 1 | My physician helps me. | 0.586 | 68.01 | 6.12 |
| My physician has enough time for me. | 0.605 |
| I trust my physician. | 0.748 |
| My physician understands me. | 0.746 |
| My physician is committed to help me. | 0.653 |
| My physician and I agree on the nature of my medical symptoms. | 0.628 |
| I can talk to my physician. | 0.665 |
| I feel content with my physician’s treatment. | 0.743 |
| I have easy access to my physician. | 0.746 |
Then, CFA was used to evaluate the factor structure achieved with EFA so that the fit of the resulting CFA was found to be satisfactory (PCFI=0.626, AGFI=0.923, CMIN/DF=1.849, NFI=0.880, and RMSEA=0.056). Cut-off criteria of the model fit indicators for the latent variable models present in [Table/Fig-1].
In addition, KMO was 0.93, and Bartlett’s test of sphericity was found to be significant (p<0.001), which reveals that the sampling was acceptable.
Discussion
It is widely accepted that psychometrics contributes significantly to the primary health care, the psychiatry, public health, and several other areas [10]. However, relationships between patients and physicians have been studied since the time of origin of medicine [10].
The purpose of the present research was the evaluation of the reliability and validity of the Persian version of PDRQ-9 in the Iranian population. Therefore, the related information was analysed and internal consistency confirmed by determining Cronbach’s alpha. Intra-class correlation coefficient was found to be acceptable. In addition, outputs from the principal component EFA with varimax rotation demonstrated that the Persian PDRQ-9 had a one-factor structure, explaining 68.01% of the total variance and had an eigenvalue of 6.12. Furthermore, other researches in diverse populations exhibited that this scale has one and two latent factors [20,24].
Therefore, based on the findings, this instrument could be presented for measuring the PDR with regard to 9 items. As a result, it exhibited excellent function of the questionnaire assessed for reliability and validity measures.
In addition, the items had suitable correlation in the present study. All nine items positively and directly correlated. Similar correlation has been seen in other studies also [25,26]. As seen in [Table/Fig-1], the model showed a suitable fit index, and the items’ validity has been confirmed. Furthermore, the items have been aggregated into one factor.
The findings of this study showed that trust in doctors would be of special importance to the patients. In addition, based on study findings, it is of great importance for the patients that the doctors understand them and their conditions. In this regard, one of the studies indicated empathy as one of the fundamental skills that physicians need to expand for helping them perceive their patients’ indirect emotions so that these emotions can be acknowledged and further explored during the patient-physician encounter [27].
Based on the findings of this research, it has been found that patients need a trustworthy and honest doctor with regard to their conditions; so that patients are able to create a suitable communication with the physicians for receiving health care services. Mercer LM et al., studied 81 patients and showed higher satisfaction of the patients who received treatment with respect, adequate attention, care and concern in comparison with patients not treated in a similar acceptable manner and not greeted appropriately [28]. Kripalani S et al., study also demonstrated the negative effects of poor communication and inadequate information to the patients on their level of satisfaction and care services during follow-ups [29]. A previous study also revealed that changes in communication with patients would bring about a positive change in practice thus increasing the patients’ satisfaction [30].
According to this research finding, it would be worthwhile to understand the patients, pay attention to them, and spend sufficient professional time with them. In this regard, Burt J et al., found the following items in a PDR; spending sufficient time for patients, asking about symptoms of the disease, listening to them, illustrating the treatment and experiment options, engaging patients in making decisions about their care services, behaving with caution and concern, and resolving their issues thoughtfully [31]. Thereby evidently, communications skills contribute significantly for adequate diagnosis, patient satisfaction, and to satisfactorily solve their respective problems and difficulties [32]. It should be noted that such qualities would be of greater importance in patients requiring longer treatment courses, in particular the health sectors where the clients are motivated for following up on their health procedures [32].
In addition, high internal consistency reported in diverse populations (α=0.94-0.95) as seen in the present research could also be seen in other evaluations of the scale, including in Dutch and German populations [20,24].
Limitation(s)
This study conducted the forward-backward translation procedure at a high standard. Nevertheless, the use of the scales developed for diverse populations constantly face potential difficulties. Moreover, it was not possible to translate cultural differences and subtle differences in the language used in this questionnaire. Therefore, it is recommended to those who use such instruments to have knowledge of these potential problems.
Conclusion(s)
Data analysis indicated reasonable reliability and validity of the Persian version of PDRQ-9 in the Iranian population in primary care. A valid and reliable instrument is considered as a key factor in the study of patient-doctor relationship especially in health centers and leads to a better understanding of this phenomenon in the studied population.
*All item p-value <0.01