Use of Vaginal Flaps and Pubovaginal Sling in Urethral Reconstruction
Kishan K Raj1, Prateek Ramdev2, Ashwin P Shekar3
1 Junior Consultant, Department of Urology, Sri Sathya Sai Institute of Higher Medical Sciences, Anantpur, Andhra Pradesh, India.
2 Senior Resident, Department of Urology, Sri Sathya Sai Institute of Higher Medical Sciences, Anantpur, Andhra Pradesh, India.
3 Consultant, Department of Urology, Sri Sathya Sai Institute of Higher Medical Sciences, Anantpur, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kishan K Raj, Department of Urology, Sri Sathya Sai Institute of Higher Medical Sciences, Puttaparthi, Anantpur, Andhra Pradesh, India.
E-mail: krajkaranth@gmail.com
The delayed or prolonged second stage of labour occurs when the foetal head exert pressure against the anterior vaginal wall and it results in ischemia and necrosis of bladder base and urethra. The ischaemic injury can result in Vesicovaginal Fistula (VVF) and Urethrovaginal Fistula (UVF). Most of the time it is related to Stress Urinary Incontinence (SUI) because of wearing out of sphincter mechanism. The index case is of a 43-year-old female who presented with total incontinence. Patient had previously undergone transvaginal fistula closure for UVF resulting from obstructed labour. On evaluation she was found to have UVF and SUI. She underwent simultaneous urethral reconstruction and pubovaginal sling surgery for SUI. Patient is currently continent and has satisfactory voiding. Simultaneous pubovaginal sling along with urethral reconstruction is a safe and feasible procedure in managing such patients.
Stress urinary incontinence, Urethrovaginal fistula, Vesicovaginal fistula
Case Report
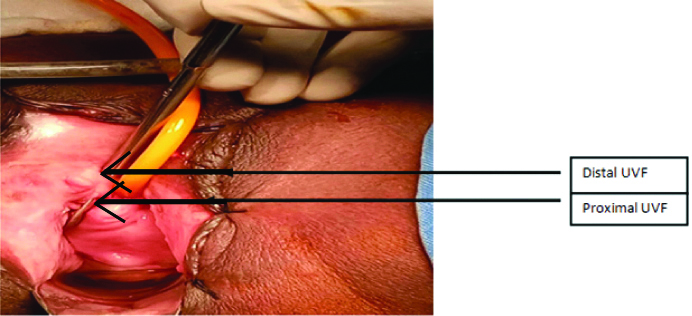
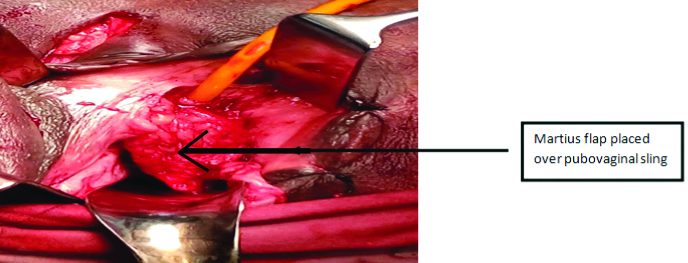
The index case is of a 43-year-old female with history of continuous urinary incontinence following vaginal delivery 25 years back. She was subsequently evaluated and was found to have UVF. She underwent transvaginal primary closure of UVF one year following the inciting event. Patient developed incontinence post urinary catheter removal on postoperative day 20. She was subsequently evaluated and told about failure of primary fistula repair. Patient presented to us 24 years later following the last surgery. Per vaginal examination showed two openings in the region of proximal urethra which is 1 cm from each other with a thin rim of tissue in between. Urethrocystoscopy showed two fistulas in urethra 1 cm from each other. There was no evidence of VVF. Patient was counseled and subsequently underwent transvaginal UVF repair under spinal anaesthesia. Patient was placed in high lithotomy position. Weighted vaginal speculum was used for exposure. Examination showed a thin rim of tissue of approximately 1 cm between proximal and distal fistula [Table/Fig-1]. This tissue was opened ventrally in midline and a U shaped vaginal flap was created which was rotated dorsally so as to form the ventral wall of the neourethra. Patient was asked to cough with full bladder after UVF repair. As there was urinary leakage, she was suspected to have SUI. Pubovaginal sling using autologous rectus sheath was fashioned and placed on the proximal part of the neourethra. The flap was further buttressed with a martius interposition flap as a second layer cover [Table/Fig-2]. Adequate voiding was achieved two weeks after removal of the catheter and now the patient was continent. Patient was on follow-up till two years with no complications.
Preoperative photograph showing distal and proximal UVF. Foleys catheter has been inserted into bladder through proximal fistula.
Intraoperative photograph of martius flap.
Discussion
Obstetric trauma is secondary to prolonged labour which leads to pressure necrosis due to compression of the foetal head against bladder trigone, bladder neck, anterior vaginal wall and urethra. The resulting ischaemic injury is a field defect that can result in VVF and UVF. The most serious amongst these is complete urethral loss. These fistulas should be repaired after a minimum of six months following the inciting event [1]. Surrounding inflammation and infection is expected to resolve by this time. The goals of repair in UVF are to create a continent channel for painless, non-obstructed passage of urine. The principles of repair include multilayer, watertight, tension free repair with interposition flap [1].
Voiding cystourethrography in lateral position can help in diagnosis and characterisation of fistula track. Endovaginal magnetic resonance imaging can be used to visualise UVF and assess periurethral scarring. Urethrocystoscopy and vaginoscopy can aid in direct visualisation of fistula [1].
Rangnekar N et al., studied the outcome in 12 patients with UVF following obstetric trauma, eight patients underwent martius repair and four patients underwent anatomic repair. One patient with a UVF treated with a martius procedure had recurrence, compared with three patients having anatomic repair [2]. Abdelbary AM, undertook a study in 19 patients with UVF and concurrent SUI. Repair of UVF in these patients was done by interposition of Martius flap and SUI which was related to it was corrected by modified anterior vaginal wall sling. All 19 patients had successful UVF repair. SUI was corrected in 16 patients (84%) [3]. Interposition with labial fat pad helps in tissue healing by providing additional lymphatic drainage and blood supply. Success of surgery is enhanced by preventing overlapping of vaginal and urethral suture lines. Rangnekar N et al., observed lower rate of dyspareunia and failure rates when martius flap was used [2].
UVF has been characterised as simple or complex based on vaginal scarring and bladder capacity [4]. As present case patient had severe vaginal scarring as a result of prior surgery and extensive urethral loss, it was a complex fistula.
The urethra can be reconstructed using local vaginal wall which is incised in a U shaped manner and the edges sutured to each other to form a tube. This was the choice of reconstruction in index patient. Vaginal advancement flaps are used when periurethral scarring is extensive. Other options in extensive urethral loss are bladder flap urethroplasty and augmentation using buccal mucosal flap [1].
Gormley EA published a series of 12 patients who underwent vaginal inlay flap urethroplasty. Ten patients had relief of their symptoms. One patient underwent recur dilation three weeks following the primary procedure. An additional patient required cystoscopy and catheter placement 58 weeks after the primary procedure [5].
The technical challenges in obstetric fistula are because ischaemic process covers a large area. The reconstructed urethra losses its muscular tone and does not coapt during periods of increased abdominal pressure. Tissue ischemia at sphincteric area may lead to SUI. Roenneburg ML and Wheeless CR observed SUI in 17% of genitourinary fistulas due to obstetric cause [6]. In a study by Hilton P, 11% of patient had SUI after successful urethral reconstruction [7]. Patients with sphincteric incontinence should undergo simultaneous anti-incontinence procedure along with urethral reconstruction. As SUI can be masked by UVF, it becomes all the more important to search for it and repair concurrently. This prevents reoperation for SUI in already ischaemic field. Pushkar DY et al., reported 50% of operated UVF to have SUI. This was corrected in a second session with 52% success rate [8].
As index patient was suspected to have sphincteric deficiency, we opted for pubovaginal sling instead of mid urethral sling. Local vaginal flaps and autologous rectus sheath are preferred options for pubovaginal sling. Alternate options include fibromuscular slings created by plication of ischiocavernosus muscle [3]. Even though harvesting of rectus sheath is thought to cause additional morbidity, index patient had short postoperative inpatient stay of five days and no wound infection occurred.
Conclusion(s)
Obstructed labour causes ischaemic injury over a large area due to field effect. UVF along with SUI can exist simultaneously. Underlying SUI can be masked in proximal urethral fistulas. In cases of complete urethral loss sling procedure can be performed along with fistula repair and thus second anti-incontinence procedure can be avoided.
Authors declaration: The following case report was presented as moderated poster titled “USE OF VAGINAL FLAPS IN URETHRAL RECONSTRUCTION FOLLOWING COMPLETE URETHRAL LOSS AS A RESULT OF OBSTETRIC INJURY: CASE REPORT” at SUZICON 2016 held in Mahatma Gandhi Medical College and research institute and Pondicherry renal sciences society during 8-10 July 2016. The images are taken from the same poster.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jan 20, 2020
Manual Googling: May 09, 2020
iThenticate Software: May 27, 2020 (10%)
[1]. Faiena I, Koprowski C, Tunuguntla H, Female urethral reconstructionJournal of Urology 2016 195(3):557-67.10.1016/j.juro.2015.07.12426478448 [Google Scholar] [CrossRef] [PubMed]
[2]. Rangnekar N, Ali NI, Kaul S, Pathak H, Role of the martius procedure in the management of urinary-vaginal fistulasJournal of the American College of Surgeons 2000 191(3):259-63.10.1016/S1072-7515(00)00351-3 [Google Scholar] [CrossRef]
[3]. Abdelbary AM, Martius flap and anterior vaginal wall sling for correction of urethrovaginal fistula (UVF) associated with stress urinary incontinence (SUI) after vaginal deliveryAfrican Journal of Urology 2012 18(4):175-79.10.1016/j.afju.2012.10.004 [Google Scholar] [CrossRef]
[4]. Browning A, Prevention of residual urinary incontinence following successful repair of obstetric vesico-vaginal fistula using a fibro-muscular slingBJOG: An International Journal of Obstetrics and Gynaecology 2004 111(4):357-61.10.1111/j.1471-0528.2004.00080.x15008773 [Google Scholar] [CrossRef] [PubMed]
[5]. Gormley EA, Vaginal flap urethroplasty for female urethral stricture diseaseNeurourology and Urodynamics 2010 29(S1)10.1002/nau.2081420419801 [Google Scholar] [CrossRef] [PubMed]
[6]. Roenneburg ML, Wheeless CR, Traumatic absence of the proximal urethraAmerican Journal of Obstetrics and Gynecology 2005 193(6):2169-72.10.1016/j.ajog.2005.08.05316325636 [Google Scholar] [CrossRef] [PubMed]
[7]. Hilton P, Urodynamic findings in patients with urogenital fistulaeBr J Urol 1998 81(4):539-42.10.1046/j.1464-410x.1998.00596.x9598624 [Google Scholar] [CrossRef] [PubMed]
[8]. Pushkar DY, Dyakov VV, Kosko JW, Kasyan GR, Management of urethrovaginal fistulaEuropean Urology 2006 50:1000-05.10.1016/j.eururo.2006.08.00216945476 [Google Scholar] [CrossRef] [PubMed]