Introduction
While, Coronary Heart Disease (CHD) mortality rates have decreased in western countries over the past four decades, this disease remains responsible for ~1/3rd of all deaths over 35 years of age. In USA, CHD might manifest nearly in a half of all middle-aged men and about one third in middle-aged women. Any form of CHD will grow in nearly half of all middle-aged within the United States. The American Heart Association (AHA) 2016 Heart Disease and Stroke Statistics estimated that 15.5 million people living in the USA are prone to CHD. The lifetime risk of developing CHD with certain significant risk factors for US citizens is 37.5% for men and 18.3% for women. [1]
Pathologically, the individuals who are at high risk to develop CVDs or have experienced the same in past require early detection strategies and medical assistance. Most CVDs can be easily avoided by mere changing of lifestyle and the risk factors such as tobacco use, poor diet, obesity, physical inactivity, excessive use of alcohol etc. [2]. On the other hand, many factors might act as predictors of CVD in the general population [3].
Under the scientific investigations, the diagnosis of the disease severity and associated new marker may help in tracing the clinical significance of any specific disease. Accurate and early diagnosis is important to employ various effective therapeutic interventions which reduces both morbidity and mortality. Based on clinical signs and symptoms, the severity of Heart Failure (HF) is classified into four classes of increasing disease progression, according to the New York Heart Association classification [4].
Recently, natriuretic peptide system is a family of similar structure but genetically distinct peptides, which includes Atrial Natriuretic Peptide (ANP), B-Type Natriuretic Peptide (BNP) and C-type Natriuretic Peptide (CNP). These peptides are characterised by a common 17 amino acid ring structure with a disulfide bond between two cysteine residues [4].
Previously published studies believed that cardiac natriuretic peptides have high association with heart disease especially as a prognostic marker for IHD through being released from myocyte and stretch fibroblasts. BNP is “a peptide produced mainly by cells in the left ventricle of the heart, which is considered as a main pumping chamber responsible for sending oxygenated blood. The peptide is highly associated with blood volume, Blood Pressure (BP) etc. Small amounts of a precursor protein, pro-BNP, are continuously produced by the heart in an inactive form, which then split by an enzyme called corin to release into the blood as active hormone BNP and its inactive fragment” [5].
When heart diseases occur, a marked increase in circulating BNP or NT-proBNP also follows. This phenomenon reflects the diminished capacity of cardiac circulatory system to deliver oxygenated blood to the body which subsequently might lead to further complication to the heart [5].
The synthesis of BNP is from their prohormone (proBNP) which is comprised of 108 amino acids. When the peptides are released into the circulation, two unequal proportions would cleave: one is active part which consist of 32 amino acid BNP, that part represents the C-terminal fragment, and the other inactive part, 76 amino acid N-terminal fragments (NT-proBNP) [5]. Further, it was postulated that stress on cardiac wall is the main reason for increasing the synthesis and secretion of NT-proBNP [5,6].
In peripheral organ, there is increasing intracellular cyclic Guanosine Mono Phosphate (cGMP) production through binding of BNP to natriuretic peptide receptor type A [7]. The cardiac natriuretic peptides are considered as natural antagonists of both the rennin-angiotensin-aldosterone and sympathetic systems. They promote diuresis, act as vasodilators, and exert anti-mitogenic action on cardiovascular tissues [8].
Serum ANP and BNP were reported to increase in various pathological conditions, especially in case of increased ventricular wall tension, increased circulating blood volume and reduction in natriuretic peptide levels. ANP exists as the granules stored in atrium and is secreted by atrial stretch. However, the secretion of BNP is regulated by the metabolic level control, usually takes a long time to stimulate. The concentration of serum BNP in patients with HF and any myocardial injury is increased manifold, according to the New York Heart Association (NYHA) [9].
The normal threshold of serum BNP concentration has been developed. A standard NTproBNP level based on the reference range of the Cleveland Clinic as: less than 125 pg/mL for patients aged 0-74 years and less than 450 pg/mL for patients aged 75-99 years. While the following NTproBNP rates as higher than 450 pg/mL for patients under 50 years of age or higher than 900 pg/mL for patients 50 years of age and older, suggests that the heart function is abnormal. Also, the concentration of serum BNP is affected by age, gender, renal failure and drug therapy [10].
The clinical application of NT-proBNP levels has found to be widely related to the severity of heart diseases. The increase in NT-proBNP levels would result into more stress to the cardiac wall and myocardial ischaemia. Research data showed the use of NT-proBNP level may be observed in three clinical settings namely: patients with acute dyspnoea, prior to discharge of in-patients hospitalised with acute HF, and the long-term management of patients with HF [11].
Other study has reported that any elevation in the levels of NT-proBNP within the normal range should be associated with increased risk of HF and this risk is enhanced in patients with diabetes mellitus [12].
Furthermore, type-2-diabetes and arterial hypertension were identified due to increasing concentration of NT-proBNP, which may serve as predictive implications for HF [13].
On the other hand, NT-proBNP has also showed a high risk factor in patients with multiple myeloma. Researchers recommend to add the NT-proBNP as a standard test for newly diagnosed myeloma [14].
Still, there is no clear definite data or research that highlights the difference in NT-proBNP levels in smokers, hypertensive and diabetic male patients with or without Acute Coronary Syndrome (ACS) that could be used as prognostic indicator.
The aim was to examine NT-proBNP levels in male patients with smoking, hypertension, and Diabetes mellitus with IHD, in comparison to the control group admitted to Cardiac Care Unit (CCU).
Materials and Methods
The present case-control study was conducted from February 2018 to June 2018 which included 90 subjects (sample size of the study were calculated based on Thompson SK equation which was more than 10% of the population) [15]. Subjects were divided into two groups: 60 male patients group were selected from CCU in AL-Hussein General Hospital in Kerbala, Iraq and 30 subjects as a healthy volunteer control. The study protocol was approved by the ethical research committee of Medicine College, University of Kerbala and Kerbala Health Directorate. Approvals were taken from the administration of Al-Hussein General Hospital and consent was obtained from all the patients and the controls.
The inclusion criteria were adult male patients with IHD who had attacks of angina or myocardial infraction, who were further diagnosed by two cardiologist on basis of their clinical manifestations, Electrocardiogram (ECG), and biochemical markers. The study included only male patients because women were highly exposed to endogenous oestrogens during their life which delay the manifestation of heart diseases.
Exclusion criteria were patients who had one or more of the following- renal disease, liver disease, diabetic nephropathy, cardiac defibrillation or HF.
The socio-demographic aspects (age) of the patients was collected through a self-reported technique (questionnaire) which also contained N- Number regarding their family history, smoking status, relevant medical and drug history.
BP was measured by well-trained staff members using a mercury sphygmomanometer with a subject in the sitting position after five minutes of rest. Blood samples were obtained from the antecubital vein after overnight fasting. Estimation of NT-proBNP was performed on MAGLUMI Fully-auto Sandwich Chemiluminescence Immunoassay (CLIA) analyser [16].
Thirty volunteer male control groups were selected as apparently healthy individuals who were free from any signs and symptoms of IHD and with negative troponin levels.
Statistical Analysis
Significant differences in continuous variables among the parameters were confirmed through analytical statistical tests such as t-test, and data between more than two groups were confirmed by the ANOVA test. The descriptive statistical calculations were performed using (Microsoft office Excel version 2016) software which calculated as (Mean±SD). Also, Boxplot was used to show the distribution of data across different groups. The p-values <0.05 were considered as statistically significant.
Results
Demographic data were initially described as mean value of groups [Table/Fig-1].
Characteristics of study participants.
| Variables | Parameters | Patients N=60 | Control N=30 |
|---|
| Demographics | Age (years) Mean±SD | 53.76±11.38 | 48.2±8.47 |
| Medical history/Patients sub-groups | Hypertension (Yes/No) | 31/29 | 8/22 |
| Diabetics mellitus (Type II) (Yes/No) | 27/33 | 0/30 |
| Smoking (Yes/No) | 46/14 | 14/16 |
| Troponin I (ng/mL) | 108.86 | 6.38 |
| NT-pro BMP | 249.89 | 62.35 |
| Body mass index (kg/m2) | 27.75 | 29.41 |
N: Number; SD: Standard deviation
The association of elevated NT-proBNP levels on patient’s conditions and their history of disease is demonstrated in [Table/Fig-2,3 and 4].
Statistical descriptive of NT-proBNP levels among asymptomatic IHD with/without smoking state and control.
| Mean±SD | p (T<=t) one-tail |
|---|
| Smokers patients vs Non-smoker patients |
| Smoker patients | 229.54±123.81 | 0.403 |
| Non-smoker patients | 219.52±199.02 |
| Non-smokers patients vs Non-smoker control |
| Non-smoker patients | 219.52±199.02 | 0.011* |
| Non-smoker controls | 46.30±25.83 |
SD: Standard deviation; p-values less than 0.05, statistically significant.
Statistical descriptive of NT-proBNP levels among asymptomatic IHD with/without diabetics Mellitus and control.
| Mean±SD | p (T<=t) one-tail |
|---|
| DM patients vs Non-DM patients |
| DM patients | 211.88±165.13 | 0.42 |
| Non-DM patients | 229.16±127.89 |
| Non-DM patients vs Non-DM control |
| Non-DM patients | 229.16±127.89 | 0.004* |
| Non-DM controls | 62.35±28.89 |
SD: Standard deviation; p-values less than 0.05, statistically significant.
Statistical descriptive of NT-proBNP levels among asymptomatic IHD with/without hypertensive and control.
| Mean±SD | p (T<=t) one-tail |
|---|
| HT patients vs Non-HT patients |
| HT patients | 232.42±190.56 | 0.402 |
| Non-HT patients | 212.55±117.54 |
| Non-HT patients vs Non-HT control |
| Non-HT patients | 212.55±117.54 | 0.014* |
| Non-HT controls | 59.53±32.55 |
SD: Standard deviation; p-values less than 0.05, statistically significant.
The [Table/Fig-2] illustrated the difference in the concentration of NT-proBNP by comparing within the smokers, non-smokers, and with healthy control. [Table/Fig-3] showed the difference in the concentration of NT-proBNP among diabetic patients, non-diabetic patients and non-diabetic healthy control. [Table/Fig-4] showed the difference in the concentration of NT-proBNP within hypertensive patients, non-hypertensive patients and with non-hypertensive healthy control.
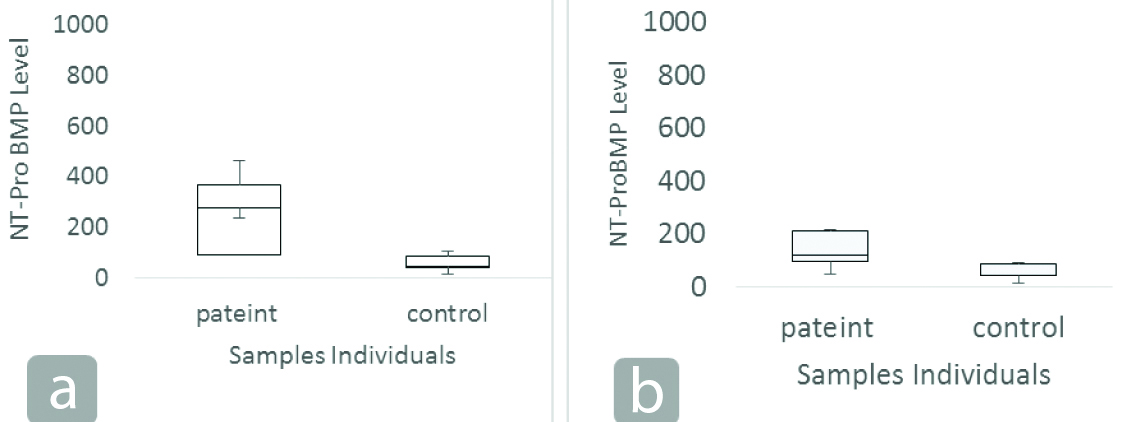
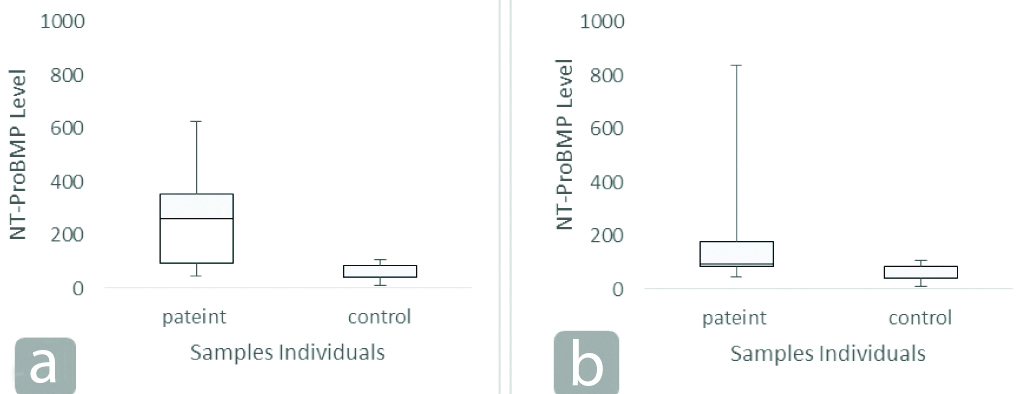
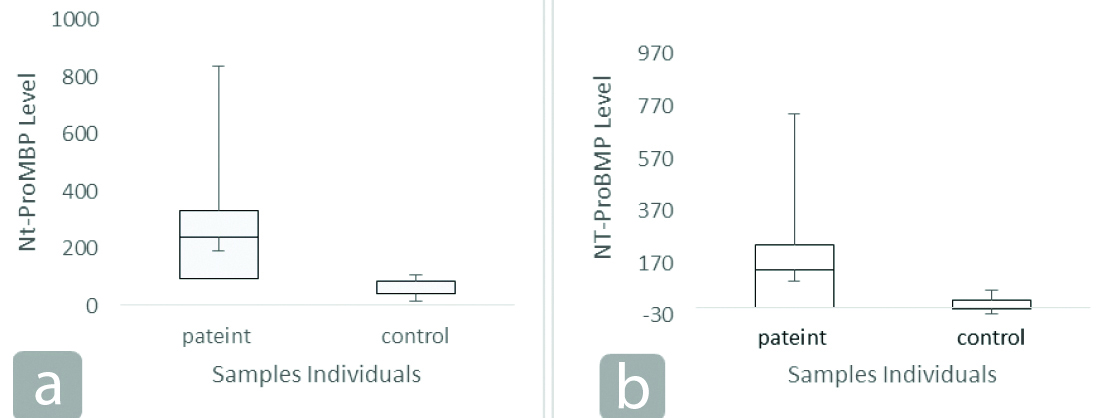
For multiple trials of the NT-proBNP measurements within the study groups, Boxplots was made to illustrate the distribution of data in a group. This further showed how Nt-proBNP values were spaced out in different sets of data within different patient’s conditions with control group [Table/Fig-5,6 and 7].
Box Plots of the NT-proBNP levels: (a) Comparison between IHD patients with diabetic and health control; (b) Comparison between IHD patients without diabetic and health control.
Box Plots of the NT-proBNP levels: (a) Comparison between IHD patients with hypertension and health control; (b) Comparison between IHD patients without hypertension and health control.
Box Plots of the NT-proBNP levels: (a) Comparison between IHD patients currently smoking and health control; (b) Comparison between non-smoker IHD patients and health control.
Discussion
Recently, NT-proBNP is the most useful biochemical markers. Serum concentration of NT-proBNP levels should be interpreted with the clinical presentation of the patients with reference to their age consideration. These levels were determined to be prognostic indicator thereby, affecting therapeutic decisions. The peptide hormone was used to investigate their level in IHD patients with/without presence of co-morbidity factors, thus classifying patients into sub-groups based on their conditions and other history diseases.
Results did not showed statistically significant difference between NT-proBNP levels in diabetic IHD patients as compared with non-diabetic patients. The main findings of the present study are illustrated in [Table/Fig-2,3, and 4] which showed significant increased levels of NT-proBNP among asymptomatic IHD without multifactorial intervention such as type 2 diabetic, HT and being active smoker. The concentration of NT-proBNP in patients under the study was about three-four fold higher as compared to the control subjects with p-value <0.01.
[Table/Fig-5a,b] demonstrated the unequal distribution of data regarding patients of IHD with/without diabetic. Each box represents the range of NT-proBNP levels in both groups. The black line within the box represents the mean of data and the whiskers represent the minimum and maximum outliers. There was a greater variability for NT-proBNP levels in IHD patients with diabetes mellitus area-mean as well as larger outliers when compared to control. Increasing level of NT-proBNP may be contributed to high glucose levels by inducing the hypertonic state, which make the NT-proBNP a good biochemical prognostic marker for cardiovascular events especially in patients with diabetes mellitus [17]. On the other hand, NT-proBNP plays a crucial role in the regulation of metabolism in diabetes mellitus patients through the proposed suggestion that highlights the role of insulin resistance in the secretion and activity of NT-proBNP [18].
Conversely, Lazo M et al., and Miyashita K et al., studied the role of increased levels of NT-proBNP as a prevention for developing insulin resistance in diabetes mellitus patients by stimulating the lipolysis process, promoting and inducing the secretion of adipokine. Both the prospective studies, inversely reported the association of BNP with the risk of diabetes across sex, race and obesity patients subgroups [19,20].
Furthermore, generally speaking, NT-proBNP is released as a response to changes in pressure within heart. These changes can be related to HF and other cardiac problems. Therefore, results were illustrated that patients with hypertension have high levels of NT-proBNP as well as larger outliers comparing to control [Table/Fig-6a,b]. In term of the arterial hypertension, natriuretic peptides were reported to have a complex role as a robust chemical marker which might induce the cardiac damage [9] through their role in both main mechanism of controlling vasodilation and diuresis [21]. On the other hand, NT-proBNP promoted the vessel wall stress which might increase the risk of hypertension in atherosclerosis risk patients [22]. In the setting of IHD, increased NT-proBNP levels resulted from the damage of ventricular and auricular wall stress which induced vasodilation. Many studies reported the contribution of multi-factors which might increase the blood vessel pressure; among which NT-proBNP was the main factor through promoting the norepinephrine release and, impacting sodium homeostasis [23,24].
Along with many other risk factors such as age, ethnicity, family history, genetic factors, socioeconomic factors, increasing BMI and other lifestyle behaviour, these factors could work together as good predictors for the development of hypertension in older adults [25]. NT-proBNP showed an opposite effect to the natriuretic peptides namely ANP, regarding the controlling of arterial BP. The mechanism was clearly confirmed by gene-targeted mice, which showed the role of both renin concentration and natriuretic peptide system through indirectly regulating BP via controlling extracellular volume by targeting vasculature diuresis [26].
Association between smoking status and increasing NT-proBNP levels in IHD patients has not yet been fully examined, particularly from biochemical viewpoint. Current results showed a greater variability for NT-proBNP levels in IHD patients with smoking habit as compared to the control [Table/Fig-7a,b]. As a normal effect of smoking, cigarette smoking induces excess vasoconstriction and accelerates atherosclerosis of coronary arteries which may decrease coronary blood flow and cause subclinical myocardial ischemia. The association between smoking status and increasing NT-pro-BNP was documented through inflammatory markers and hypertension [27].
However, many other mechanisms might be involved in the association between smoking and hypertension such as alteration of some genotypes by environment interactions, non-genetic factors such as ecto-5’- nucleotidase, xanthine oxidase etc., [28-30]. Blood level of carbon monoxide, a major chemical compound in cigarette smoke, may also induce hypoxemia and myocardial hypoxia [31]. These conditions in turn suggest that increased cardiac overload can lead to subsequent increase in secretion of NT-proBNP. Increased NT-proBNP levels might be a good indicator for the severity of heart diseases. However, many offending agents might interfere with the progress in such cases.
Limitation(s)
The limitations of the study include the smaller sample size of the study, not highlighting the role of NT-proBNP as a predictive marker for mortality and HF especially in regard to ACS and all the confounding and offending factors were not assessed.
Conclusion(s)
The present study demonstrated that NT-proBNP is a vital prognostic and monitoring tool for IHD patients, assessing disease progress and the stability of heart function. In future, further studies need to emphasise the role of NT-proBNP as a predictive markers for mortality and HF specially after, ACS and just not get restricted to the recurrent ischemic events. Many offending agents should be under consideration due to their interference with the progress of such cases like: site of ACS (lateral, internal MI and unstable angina), duration of case (extent of infraction), time of intervention, time of sampling, time of acute presentation (in such patients there was delay in diagnosis).
N: Number; SD: Standard deviation
SD: Standard deviation; p-values less than 0.05, statistically significant.
SD: Standard deviation; p-values less than 0.05, statistically significant.
SD: Standard deviation; p-values less than 0.05, statistically significant.
[1]. Sanchis-Gomar F, Perez-Quilis C, Leischik R, Lucia A, Epidemiology of coronary heart disease and acute coronary syndromeAnn Transl Med 2016 4(13):25610.21037/atm.2016.06.3327500157 [Google Scholar] [CrossRef] [PubMed]
[2]. Ambrose JA, Singh M, Pathophysiology of coronary artery disease leading to acute coronary syndromesF1000 Prime Rep 2015 7:0810.12703/P7-0825705391 [Google Scholar] [CrossRef] [PubMed]
[3]. Khadem Ansari MH, Rasmi Y, Rahimi Pour A, Jafarzadeh M, The association between serum apolipoprotein AI and apolipoprotein B and the severity of angiographical coronary artery diseaseSingapore Med J 2009 50(6):610-13. [Google Scholar]
[4]. Nakao K, Ogawa Y, Suga SI, Imura H, Molecular biology and biochemistry of the natriuretic peptide system. I: Natriuretic peptidesJ Hypertens 1992 10(9):907-12.10.1097/00004872-199209000-00001 [Google Scholar] [CrossRef]
[5]. McKie PM, Cataliotti A, Sangaralingham SJ, Ichiki T, Cannone V, Bailey KR, Predictive utility of atrial, N-terminal pro-atrial, and N-terminal pro-B-type natriuretic peptides for mortality and cardiovascular events in the general community: A 9-year follow-up studyMayo Clin Proc 2011 86(12):1154-60.Elsevier10.4065/mcp.2011.043722134933 [Google Scholar] [CrossRef] [PubMed]
[6]. Weber M, Hamm C, Role of B-type natriuretic peptide (BNP) and NT-proBNP in clinical routineHeart 2006 92(6):843-49.10.1136/hrt.2005.07123316698841 [Google Scholar] [CrossRef] [PubMed]
[7]. Pandey KN, Guanylyl cyclase/natriuretic peptide receptor-A signaling antagonizes phosphoinositide hydrolysis, Ca(2+) release, and activation of protein kinase CFront Mol Neurosci 2014 7:75Published 2014 Aug 2210.3389/fnmol.2014.0007525202235 [Google Scholar] [CrossRef] [PubMed]
[8]. Richards AM, Doughty R, Nicholls MG, MacMahon S, Sharpe N, Murphy J, Plasma N-terminal pro-brain natriuretic peptide and adrenomedullin: Prognostic utility and prediction of benefit from carvedilol in chronic ischemic left ventricular dysfunctionJ Am Coll Cardiol 2001 37(7):1781-87.10.1016/S0735-1097(01)01269-4 [Google Scholar] [CrossRef]
[9]. Hall C, Essential biochemistry and physiology of (NT-pro) BNPEur J Heart Fail 2004 6(3):257-60.10.1016/j.ejheart.2003.12.01514987573 [Google Scholar] [CrossRef] [PubMed]
[10]. Daniels LB, Maisel AS, Natriuretic peptidesJ Am Coll Cardiol 2007 50:2357-68.10.1016/j.jacc.2007.09.02118154959 [Google Scholar] [CrossRef] [PubMed]
[11]. Rivera M, Taléns-Visconti R, Salvador A, Bertomeu V, Miró V, de Burgos FG, NT-proBNP levels and hypertension. Their importance in the diagnosis of heart failureRev Esp Cardiol 2004 57(5):396-402.10.1016/S0300-8932(04)77124-9 [Google Scholar] [CrossRef]
[12]. Nguyen K, Bertoni A, Budoff M, deFilippi C, Fan W, Lombardo D, NT-proBNP predicts risk for developing heart failure and cardiovascular disease events according to glucose status in the multi-ethnic study of atherosclerosis (MESA)Circulation 2018 138(Suppl_1):A12904 [Google Scholar]
[13]. Troebs SO, Schwuchow S, Grosch M, Göbel S, Diestelmeier S, Schulz A, Determinants of early diastolic strain rate and its relation to NT-proBNP in heart failureCirculation 2018 138(Suppl_1):A14967 [Google Scholar]
[14]. Milani P, Vincent Rajkumar S, Merlini G, Kumar S, Gertz MA, Palladini G, N-terminal fragment of the type-B natriuretic peptide (NT-proBNP) contributes to a simple new frailty score in patients with newly diagnosed multiple myelomaAm J Hematol 2016 91(11):1129-34.10.1002/ajh.2453227508522 [Google Scholar] [CrossRef] [PubMed]
[15]. Thompson SK, Sampling 2012 3rd ed:59-60.10.1002/9781118162934 [Google Scholar] [CrossRef]
[16]. Nambi V, Liu X, Chambless LE, De Lemos JA, Virani SS, Agarwal S, Troponin T and N-Terminal Pro-B-Type natriuretic peptide: A biomarker approach to predict heart failure risk-The atherosclerosis risk in communities studyClin Chem 2013 59(12):1802-10.10.1373/clinchem.2013.20363824036936 [Google Scholar] [CrossRef] [PubMed]
[17]. Peng Q, Hu W, Su H, Yang Q, Cheng X, Levels of B-type natriuretic peptide in chronic heart failure patients with and without diabetes mellitusExp Ther Med 2013 5(1):229-32.10.3892/etm.2012.76023251273 [Google Scholar] [CrossRef] [PubMed]
[18]. Mizuno Y, Harada E, Katoh D, Kashiwagi Y, Morikawa Y, Nakagawa H, Cardiac production of B-type natriuretic peptide is inversely related to the plasma level of free fatty acids in obese individuals-possible involvement of the insulin resistanceEndocr J 2012 :EJ12-0239. [Google Scholar]
[19]. Lazo M, Young JH, Brancati FL, Coresh J, Whelton S, Ndumele CE, NH2-terminal pro-brain natriuretic peptide and risk of diabetesDiabetes 2013 62(9):3189-93.10.2337/db13-047823733199 [Google Scholar] [CrossRef] [PubMed]
[20]. Miyashita K, Itoh H, Tsujimoto H, Tamura N, Fukunaga Y, Natriuretic peptides/cGMP/cGMP-dependent protein kinase cascades promote muscle mitochondrial biogenesis and prevent obesityDiabetes 2009 58(12):2880-92.10.2337/db09-039319690065 [Google Scholar] [CrossRef] [PubMed]
[21]. Jeppesen JL, Nielsen SJ, Torp-Pedersen C, Hansen TW, Olsen MH, Berg ND, Genetic variation in the natriuretic peptide system, circulating natriuretic peptide levels, and blood pressure: An ambulatory blood pressure studyAm J Hypertens 2012 25(10):1095-100.10.1038/ajh.2012.9622785411 [Google Scholar] [CrossRef] [PubMed]
[22]. Bower JK, Lazo M, Matsushita K, Rubin J, Hoogeveen RC, Ballantyne CM, N-terminal pro-brain natriuretic peptide (NT-proBNP) and risk of hypertension in the Atherosclerosis Risk in Communities (ARIC) studyAm J Hypertens 2015 28(10):1262-66.10.1093/ajh/hpv02625783741 [Google Scholar] [CrossRef] [PubMed]
[23]. Levin ER, Gardner DG, Samson WK, Natriuretic peptidesN Engl J Med 1998 339:321-28.10.1056/NEJM1998073033905079682046 [Google Scholar] [CrossRef] [PubMed]
[24]. Felder RA, White MJ, Williams SM, Jose PA, Diagnostic tools for hypertension and salt sensitivity testingCurr Opin Nephrol Hypertens 2013 22(1):6510.1097/MNH.0b013e32835b369323197156 [Google Scholar] [CrossRef] [PubMed]
[25]. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Executive summary: Heart disease and stroke statistics-2015 update: A report from the American Heart AssociationCirculation 2015 131(4):434-41.10.1161/CIR.0000000000000157 [Google Scholar] [CrossRef]
[26]. Demerath T, Staffel J, Schreiber A, Valletta D, Schweda F, Natriuretic peptides buffer renin-dependent hypertensionAm J Physiol Renal Physiol 2014 306(12):F1489-98.10.1152/ajprenal.00668.201324717731 [Google Scholar] [CrossRef] [PubMed]
[27]. Ambrose JA, Barua RS, The pathophysiology of cigarette smoking and cardiovascular disease: An updateJ Am Coll Cardiol 2004 43(10):1731-37.10.1016/j.jacc.2003.12.04715145091 [Google Scholar] [CrossRef] [PubMed]
[28]. Cheung BM, Ong KL, Tso AW, Leung RY, Xu A, Cherny SS, C-reactive protein as a predictor of hypertension in the Hong Kong Cardiovascular Risk Factor Prevalence Study (CRISPS) cohortJ Hum Hypertens 2012 26(2):108-16.10.1038/jhh.2010.12521270838 [Google Scholar] [CrossRef] [PubMed]
[29]. Li MD, Cheng R, Ma JZ, Swan GE, A meta-analysis of estimated genetic and environmental effects on smoking behavior in male and female adult twinsAddiction 2003 98(1):23-31.10.1046/j.1360-0443.2003.00295.x12492752 [Google Scholar] [CrossRef] [PubMed]
[30]. Hameed RM, Mehdi WA, Mehde AA, Biochemical significance of Ecto-5’- Nucleotidase, Xanthine Oxidase, and Glutathione S-Transferase determinations in sera of cigarette and water pipe young men smokersMed J Babylon 2019 16(1):70-76.10.4103/MJBL.MJBL_2_19 [Google Scholar] [CrossRef]
[31]. Leone A, Biadi O, Balbarini A, Smoking and cardiovascular system: Cellular features of the damageCurr Pharm Des 2008 14(18):1771-77.10.2174/13816120878474669918673180 [Google Scholar] [CrossRef] [PubMed]