Rare Cause of Hemifacial Spasm: Diagnosed on Magnetic Resonance Imaging
Madhurima Sharma1, Munish Dev2
1 Consultant, Department of Radiology, Imaging World Diagnostic Centre, Ahmedabad, Gujarat, India.
2 Consultant, Department of Cardiology, Apex Heart Institute, Ahmedabad, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Madhurima Sharma, Imaging World Diagnostic Centre, Amrapali Axiom, Bopal, Ahmedabad, Gujarat, India.
E-mail: madhurimashrm88@gmail.com
Magnetic resonance angiography, Vertebral artery, Vertebrobasilar dolichoectasia
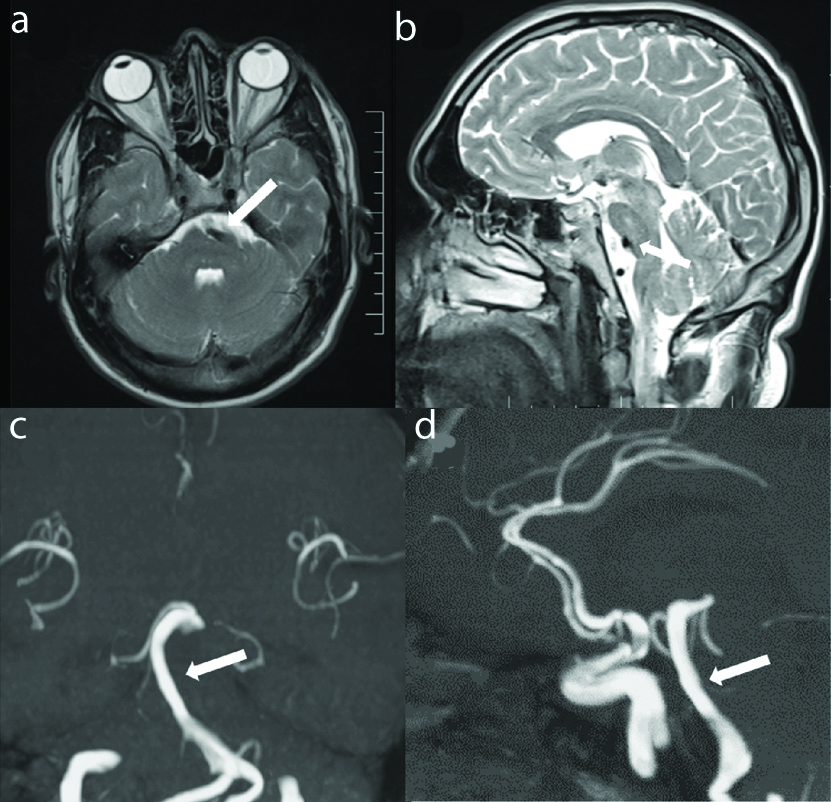
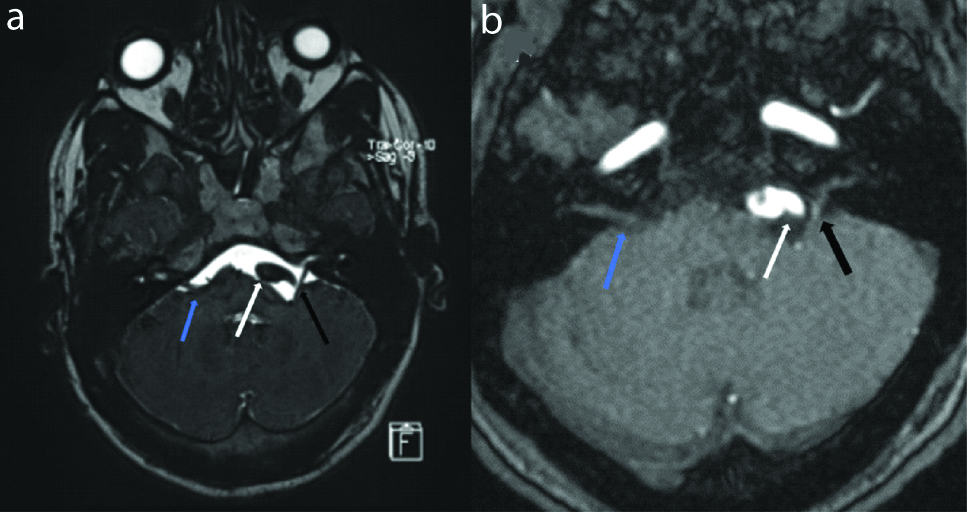
A 36-year-old hypertensive male presented with involuntary twitching involving left side of face for last 3 days. On neurological examination, left hemifacial spasm was present. Rest of neurological examination including cranial nerve examination was within normal limits. Patient underwent Magnetic Resonance Imaging (MRI) of brain with angiography of intracranial vessels. On T2 weighted images, prominent flow void of basilar artery was seen causing indentation upon anterior aspect of pons with resultant deformation [Table/Fig-1a,b]. Pons and medulla however showed normal signal intensity. Sampling Perfection with Application optimized Contrasts using different flip angle Evolution (SPACE) sequence and 3D Time of Flight (TOF) MR angiography showed dilated and tortuous bilateral vertebral arteries and basilar artery. Basilar artery measured ~6.2 mm in maximum caliber and showed abnormal lateral course (slightly lateral to clival margin) with presence of high bifurcation at the level of third ventricle [Table/Fig-1c,d]. Right vertebral artery was elongated and seen crossing the midline towards left side. Left vertebral artery was also tortuous and more lateral in course resulting in displacement of left facial nerve with compression upon root exit zone [Table/Fig-2]. Right 7th, 8th nerve complex was normal. Bilateral 5th, 9th and 10th nerves were normal in their intracranial course and morphology. Based upon these findings, a diagnosis of vertebrobasilar dolichoectasia, causing compression upon left facial nerve was made. Patient was offered option of botulinum toxin injection for symptomatic relief. However, patient refused the injection and was lost to follow-up.
(a-d): Axial (a) and sagittal (b) T2 weighted images showing prominent flow void of basilar artery (white arrow) causing indentation upon anterior aspect of pons. Coronal (c) and sagittal (d) reformatted images of TOF MR angiography showing mildly dilated and tortuous basilar artery (white arrow) with abnormal lateral course and high bifurcation. These findings are suggestive of vertebrobasilar dolichoectasia.
(a,b): Axial SPACE and axial TOF MR angiography image at the level of cerebellopontine angle shows tortuous left vertebral artery (white arrow) causing displacement and stretching of left facial nerve with compression upon root exit zone (black arrow). Also note normal course of facial nerve on right side (blue arrow).
Hemifacial spasm is characterised by involuntary tonic-clonic contractions of muscles supplied by facial nerve. It can result from compression of ipsilateral facial nerve by a vascular loop or cerebellopontine angle mass [1]. Facial nerve has its nucleus in pons with nerve fibers exiting from inferior border of pons. Nerve root entry or exit zone is the transition point from central to peripheral myelin and is most susceptible for vascular compression [2,3]. It is postulated that pulsatile compression by the vessel produced demyelination at root entry zone of the nerve leading to abnormal transmission of impulses [4]. Direct compression of facial nerve by dilated vertebral artery is rare, accounting for 0.7% cases of hemifacial spasm in a previous study [5].
Vertebrobasilar Dolichoectasia (VBD) is characterised by abnormal dilatation, elongation and tortuosity of vertebrobasilar system [6]. Diagnosis of VBD is made when basilar artery measures ~4.5 mm in maximum caliber (typically measured at the level of mid-pons on axial images), lies lateral to clival margin and shows high bifurcation above the level of floor of third ventricle [6]. Patients with VBD are often elderly hypertensive males predominant left sided involvement [2]. In the present case, manifestation of VBD at a younger age could be seen. A congenital vascular anomaly is thought to be responsible for dolichoectasia in these cases [7]. In most of the cases VBD remains asymptomatic and is detected as incidental finding. Symptomatic cases of VBD can present with ischemic stroke, intraparenchymal, subarachnoid haemorrhage or compressive symptoms due to mass effect on adjacent brainstem and cranial nerves [6]. Treatment of hemifacial spasm due to VBD can be medical or surgical. Medical treatment consists of botulinum toxin injection, which provides symptomatic relief with effect lasting 4-6 months [8]. Surgical treatment consisting of microvascular decompression is the definitive treatment. However, it carries the risk of hearing impairment and facial nerve palsy [9].
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 26, 2020
Manual Googling: May 09, 2020
iThenticate Software: May 25, 2020 (8%)
[1]. Abdel Hamid M, John K, Rizvi T, Huff N, Hemifacial spasm due to vertebrobasilar dolichoectasia: A case reportRadiology Case Reports 2015 10(4):65-67.10.1016/j.radcr.2015.08.00626649123 [Google Scholar] [CrossRef] [PubMed]
[2]. Aga P, Parashari U, Parihar A, Yadav R, Singh R, Kohli N, Simultaneous involvement of fifth and seventh nerves by vertebrobasilar dolichoectasia presenting as painful tic convulsif-Demonstrated by MR imagingNeurology India 2010 58(1):16310.4103/0028-3886.6039420228501 [Google Scholar] [CrossRef] [PubMed]
[3]. Woolfall P, Coulthard A, Pictorial review: Trigeminal nerve: Anatomy and pathologyBr J Radiol 2001 74(881):458-67.10.1259/bjr.74.881.74045811388997 [Google Scholar] [CrossRef] [PubMed]
[4]. Smoker WR, MJ Price, WD Keyes, JJ Corbett, LR Gentry, High-resolution computed tomography of basilar arteryAJNR 1986 7(1):55-60. [Google Scholar]
[5]. Han IB, Chang JH, Chang JW, Huh R, Chung SS, unusual causes and presentations of hemifacial spasmNeurosurgery 2009 65(1):130-37.10.1227/01.NEU.0000348548.62440.4219574834 [Google Scholar] [CrossRef] [PubMed]
[6]. Samim M, Goldstein A, Schindler J, Johnson MH, Multimodality imaging of vertebrobasilar dolichoectasia: Clinical presentations and imaging spectrumRadiographics 2016 36(4):1129-46.10.1148/rg.201615003227315445 [Google Scholar] [CrossRef] [PubMed]
[7]. Hegedus K, Ectasia of basilar artery with special reference to possible pathogenesisSurg Neurol 1985 24(4):463-69.10.1016/0090-3019(85)90309-X [Google Scholar] [CrossRef]
[8]. Czyz CN, Burns JA, Petrie TP, Watkins JR, Cahill KV, Foster JA, Long-term botulinum toxin treatment of benign essential blepharospasm, hemifacial spasm, and Meige syndromeAm J Ophthalmol 2013 156(1):173e-177.e2.10.1016/j.ajo.2013.02.00123541393 [Google Scholar] [CrossRef] [PubMed]
[9]. Mikami T, Minamida Y, Akiyama Y, Wanibuchi M, Sugino T, Houkin K, Microvascular decompression for hemifacial spasm associated with the vertebral arteryNeurosurg Rev 2013 36(2):303-09.10.1007/s10143-012-0425-y23053242 [Google Scholar] [CrossRef] [PubMed]