Imaging Findings of Inferior Vena Cava Web Associated with Primary Budd Chiari Syndrome- A Case Report in Elderly Male
Shyam Kumar Nandhakumar1, Amirthaganesh Balasubramanium2, Prabhu Sugumaran3, Lokesh Kumar Thilagaraj4, Armel Arputha Sivarajan5
1 Postgraduate Resident, Department of Radiodiagnosis, Mahatma Gandhi Medical College and Research Institute, SBV University, Pondicherry, India.
2 Professor and Head, Department of Cardiology, Mahatma Gandhi Medical College and Research Institute, SBV University, Pondicherry, India.
3 Associate Professor, Department of Radiodiagnosis, Mahatma Gandhi Medical College and Research Institute, SBV University, Pondicherry, India.
4 Associate Professor, Department of Radiodiagnosis, Mahatma Gandhi Medical College and Research Institute, SBV University, Pondicherry, India.
5 Assistant Professor, Department of Radiodiagnosis, Mahatma Gandhi Medical College and Research Institute, SBV University, Pondicherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Amirthaganesh Balasubramanium, Professor and Head, Department of Cardiology, Mahatma Gandhi Medical College and Research Institute, Sri Balaji Vidyapeeth, Puducherry, India.
E-mail: amirtha2001@rediffmail.com
Budd Chiari Syndrome (BCS) is characterised by obstruction of hepatic venous outflow and Inferior Vena Cava (IVC) causing portal hypertension. The gold standard imaging for such a case is Contrast Enhanced Computed Tomography (CECT). The conventional treatment of BCS involves systemic thrombolysis, surgical shunt (transjugular intrahepatic portosystemic shunt) or IVC venoplasty with stenting with or without hepatic venoplasty. A case of 60-year-old male who presented with complaints of 3 months history of right loin pain and nocturia, who was later diagnosed with BCS with IVC web is presented. The clinical history was atypical whilst the Imaging findings of multiple venous collaterals on CECT abdomen and echogenic IVC thrombus traced till Right Atrium (RA) on longitudinal grey scale Ultrasonogram (USG) aided in diagnosis. The percutaneous interventional procedure of IVC venoplasty with stenting was done and patient recovered with good prognosis.
Contrast enhanced computed tomography, Hepatic venous outflow, Ultrasonogram, Venoplasty with stenting
Case Report
A 60-year-old male patient presented with complaints of right loin pain since 3 months and nocturia since 2 months. The pain was moderate dull aching, not associated with any aggravating or relieving factors and localised to right side loin region. A previous history of varicose veins, treated 1 year back on right lower limb was present. On clinical examination, there was no evidence of icterus, abdominal distention and hepatomegaly. The examination showed dilated tortuous veins in lateral abdomen and periumbilical region, tenderness elicited on right loin region and presence of right lower limb varicosity. The hepatojugular venous reflex was absent. The case was under diagnostic workup with suspicion of alcoholic liver disease, cirrhosis, subacute BCS, Right-sided heart failure and Metastatic liver disease were listed under differential diagnoses. The routine investigations like haemogram, coagulogram, renal and liver function tests, serum electrolytes were unremarkably normal. Routine urinary examination and microscopy also revealed no abnormalities. The imaging namely USG abdomen and CECT was performed for further evaluation.
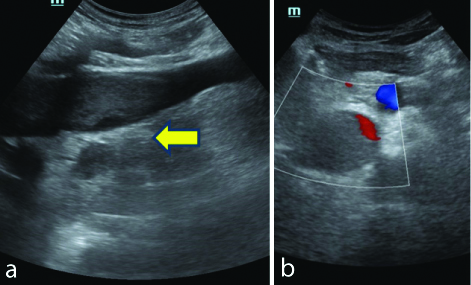
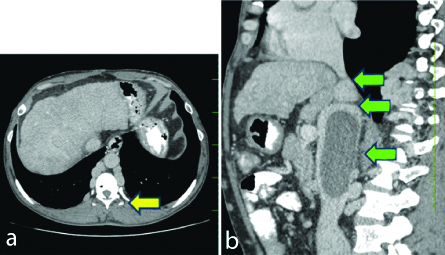
The USG abdomen revealed suprarenal IVC demonstrating echogenic thrombus (9 cm) extending till RA [Table/Fig-1a]. No flow was noted within the IVC on Doppler study [Table/Fig-1b]. A CECT was done after USG, which revealed an IVC Web at the supra and infrahepatic junction with post-stenotic IVC dilatation and long segment IVC thrombus (likely secondary to chronic venous stasis) with multiple venous collaterals [Table/Fig-2a]. The liver showed coarse pattern with surface nodularity, possibly evolving cirrhosis and associated splenomegaly was present. The features of portal hypertension i.e., dilated portal vein, oesophageal varices were also found. A thin membrane was noted in the junction of supra and infrahepatic part of IVC (2 cm below the RA) suggestive of IVC web [Table/Fig-2b]. The IVC web was causing stenosis (8 mm caliber) with post-stenotic IVC dilatation (maximum caliber 41 mm) with notable tortuosity. Long segment (for a length=9 cm) intraluminal filling defect involving suprarenal and infrarenal IVC (for a length ~3 cm below the renal vein insertion) noted suggestive of thrombosis. Dilated iliac veins and hemiazygous veins noted. Multiple venous collaterals noted in the retrocaval, infrahepatic, coronary ligament, oesophageal and paraoesophageal (varices), gastric and paragastric, paravertebral venous plexus, abdominal wall (anterior and lateral abdominal wall subcutaneous plane and intramuscular plane). Right, Middle and left hepatic vein are narrow in caliber at its termination to IVC (which is not clearly delineated and shows some soft tissue density)-possibility of hepatic outflow venous obstruction to be considered. The clinical data and imaging findings were consistent with that of IVC web associated with BCS.
a) Grayscale USG Abdomen showing IVC hyperechoeic lesion extending till Right Atrium (RA) suggestive of a thrombus. The yellow arrow signifies IVC hyperechoiec lesion extending till RA suggestive of thrombus; b) No flow on Doppler settings.
a) Axial CECT abdomen showing multiple Para esophageal and paravertebral collaterals (Yellow arrow); b) Sagital CECT abdomen demonstrating IVC web, poststenotic dilatation and echogenic thrombus seen in IVC (Green arrows).
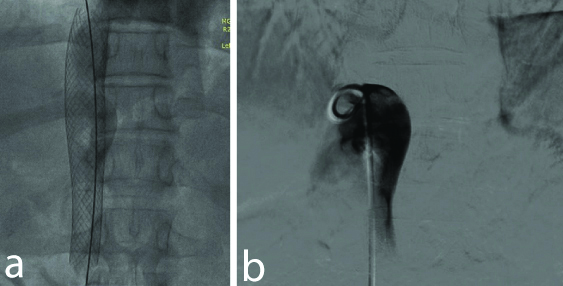
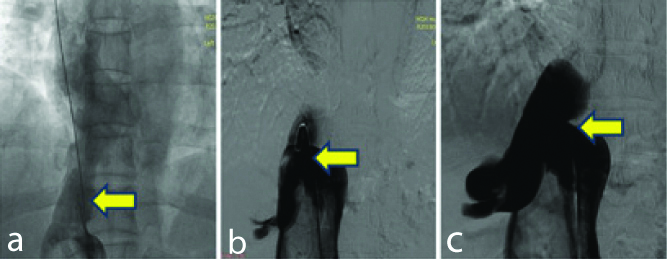
The case was treated with IVC venoplasty with stenting [Table/Fig-3a,b]. The procedure involved right femoral venous approach, a 12 F cook sheath introduced and positioned in IVC. Venogram showed dilated IVC with thrombus and narrowing of IVC 3-5 cm below the IVC- RA junction with thick membrane. There were no antegrade flows across the IVC into RA. There were extensive collaterals and dilated hepatic veins. There was gross dilatation of IVC 5-10 cm below the membrane and measured around 40 mm diameter. An initial attempt to perforate the membrane using soft end of straight Teflon and J terumo wire had failed. Then the membrane was perforated using back end of exchange length Teflon wire using 8 F dilator support. Then wire was advanced into Superior vena cava via main pulmonary artery and wire end reversed. Teflon wire was parked in left axillary vein and the membrane was dilated using 14 F Mullins Dilator, then the membrane was sequentially dilated using 22 mm × 40 mm Atlas Balloon at 6 atm pressure for one minute. Digital subtraction angiography [Table/Fig-4a-c] was done to measure IVC size, which showed narrowest part ranging around 16 mm, size of IVC at RA junction approximately 22 mm and length of IVC till thrombus part is around 40 mm. The IVC was stented using 24 × 70 mm self-expanding wall stent (Boston Scientific) from IVC-RA junction. Final Venogram showed well expanded stent with good IVC flow into RA. Patient had tolerated the procedure with no post-procedural complications. Patient was followed-up for 3 months, 6 months and then one year and was found asymptomatic during follow-up appointments.
a) IVC venoplasty; b) stenting was done.
Digital subtraction angiography showing the of IVC narrowest part ranging around 16 mm (arrows).
Discussion
BCS can be described as a diverse group of diseases characterised by hepatic venous outflow obstruction at the IVC or level of hepatic veins which leads to portal hypertension. Timely analysis of BCS is essential for establishing appropriate treatment [1]. Therefore, imaging studies combined with clinical data are often essential for reaching a definitive diagnosis. Evaluation of extent of occlusion of hepatic veins, inferior venacava and presence of intrahepatic collateral vessels is most important part of imaging examinations of patients with BCS [1,2].
The syndrome has a reported epidemiology of 1 out of 100,000 individuals and is more common in females. Anatomically, the right hepatic vein drains directly into the IVC, left and middle hepatic veins often unite to drain [1]. This BCS will show tissue hypertrophy and the perfusion changes in the caudate lobe of liver on imaging. Hepatic vein outflow obstruction leads to amplified hepatic pressure, resulting in collateral venous circulation, increased sinusoidal pressure and portal vein thrombosis. The result is liver cell failure [1,2]. Primary BCS is due to intrinsic thrombosis or vessel webs. Secondary BCS is caused by external infectious (tuberculosis/aspergillosis/parasites) or neoplastic compression or metastasis occurring from hepatocellular carcinoma/ renal cell carcinoma/ retroperitoneal sarcomas [1,2]. The current case had aetiology of vessel web (IVC web) which is a post-thrombotic squeal after vessel occlusion. Patients with BCS characteristically have abdominal distension, pain, ascites, hepatomegaly, and absent hepatojugular venous reflex. However, the present case showed tenderness (loin region) and nocturia only.
Considering secondary BCS all possible investigation should be done to rule out fatal malignancies, which were done and found negative for the present case. Imaging is an essential diagnostic tool when clinical presentation is atypical as in this case. Direct sonographic analysis of the IVC can also reveal enlargement, stenosis, or obstruction of the IVC by a thrombus or web in suspected BCS [3,4]. The current case showed altered echo pattern of liver, surface nodularity and IVC web associated collaterals were noted in gray scale USG. CT and MR angiography provide preoperative assessments for BCS, possible missed secondary BCS features or interventional planning. CT angiography was used in the present case with interventional surgical correction (IVC venoplasty and stenting) [1,5]. Functional MR (perfusion assessments) would indicate on possible vessel occlusion/webs. Such advanced imaging was not necessitated, and the diagnosis was established by routine USG and CT angiography in the present case [4].
The treatment options for the primary BCS range from interventional angioplasty to liver transplant [6,7]. The present case was treated with IVC venoplasty with stenting. Thrombosis or infection may occur as a consequence of interventional procedure, which had not occurred in our case.
Bayraktar UD et al., had described in their review, that three syndromes to have similar presentation namely: Veno-Occlusive Disease (VOD) at the level of sinusoids and terminal venues, the BCS from hepatic veins to the superior end of IVC and Venous obstruction at the level of heart referred to as Congestive Hepatopathy (CH) [8]. A case report of a female with a diagnosis of cryptogenic cirrhosis for several years was found to have BCS due to an IVC web after a radiological diagnostic work up [9]. The similar management protocol was followed as in the above case. This undermines need for strict clinical and radiological examinations.
Wang R et al., in a study of 41 cases of BCS had concluded that Interventional therapy is the first therapeutic choice for BCS patients with IVC thrombosis of Type I, Type II or Type III with acute thrombosis. For the patients of Type III with an obsolete thrombus (as in the current case), surgical shunts or conservative treatment were indicated [10].
Conclusion(s)
Primary BCS may present with clinically atypical symptoms, which may need imaging based studies to confirm the diagnosis simultaneously ruling out possible secondary BCS. The treatment may need interventional angioplasty and stenting with a synergistic effort of radiologists and interventional cardiologists.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 16, 2020
Manual Googling: May 06, 2020
iThenticate Software: May 25, 2020 (12%)
[1]. Bozorgmanesh A, Selvam DA, Caridi JG, Budd-Chiari syndrome: hepatic venous web outflow obstruction treated by percutaneous placement of hepatic vein stentSemin Intervent Radiol 2007 24(1):100-05.10.1055/s-2007-97120021326746 [Google Scholar] [CrossRef] [PubMed]
[2]. Bogin V, Marcos A, Shaw-Stiffel T, Budd-Chiari syndrome: In evolutionEur J Gastroenterol Hepatol 2005 17(1):33-35.10.1097/00042737-200501000-0000715647637 [Google Scholar] [CrossRef] [PubMed]
[3]. Bargallo X, Gilabert R, Nicolau C, García-Pagán JC, Ayuso JR, Brúet C, Sonography of Budd-Chiari syndromeAJR Am J Roentgenol 2006 187(1):W33-41.10.2214/AJR.04.091816794137 [Google Scholar] [CrossRef] [PubMed]
[4]. Bansal V, Gupta P, Sinha S, Dhaka N, Kalra N, Vijayvergiya R, Budd-Chiari syndrome: Imaging reviewBr J Radiol 2018 91(1092):2018044110.1259/bjr.2018044130004805 [Google Scholar] [CrossRef] [PubMed]
[5]. Liu SY, Xiao P, Cao HC, Jiang HS, Li TX, Accuracy of computed tomographic angiography in the diagnosis of patients with inferior vena cava partial obstruction in Budd-Chiari syndromeJ Gastroenterol Hepatol 2016 31(12):1933-39.10.1111/jgh.1342027118067 [Google Scholar] [CrossRef] [PubMed]
[6]. Sanchez-Recalde A, Sobrino N, Galeote G, Orbe LC, Merino JL, Sobrino JA, Budd-Chiari syndrome with complete occlusion of the inferior vena cava: Percutaneous recanalization by angioplasty and stentingRev Esp Cardiol 2004 57(11):1121-23.10.1016/S0300-8932(04)77248-6 [Google Scholar] [CrossRef]
[7]. Zhang CQ, Fu LN, Zhang GQ, Zhang GQ, Jia T, Liu JY, Long-term effect of stent placement in 115 patients with Budd-Chiari syndromeWorld J Gastroenterol 2003 9(11):2587-91.10.3748/wjg.v9.i11.258714606103 [Google Scholar] [CrossRef] [PubMed]
[8]. Bayraktar UD, Seren S, Bayraktar Y, Hepatic venous outflow obstruction: Three similar syndromesWorld J Gastroenterol 2007 (13):1912-27.10.3748/wjg.v13.i13.191217461490 [Google Scholar] [CrossRef] [PubMed]
[9]. Nnaemeka A, Ira M, James P, Chronic inferior vena caval web as a rare cause of cirrhosisAm J Gastroenterol 2013 108:S15010.14309/00000434-201310001-00508 [Google Scholar] [CrossRef]
[10]. Wang R, Meng Q, Qu L, Wu X, Sun N, Jin X, Treatment of Budd-Chiari syndrome with inferior vena cava thrombosisExp Ther Med 2013 5(4):1254-58.10.3892/etm.2013.9612359649 [Google Scholar] [CrossRef] [PubMed]