Shoulder is a joint in which mobility is gained at the cost of stability. This makes it the joint which is most vulnerable for dislocations or subluxations. In few of these patients, the shoulder tends to dislocate or subluxate after the first dislocation even with trivial or no trauma [1].
Aetiology of shoulder dislocation is of two types, traumatic and atraumatic. Atraumatic dislocation occurs due to presence of tissue laxity. Whereas in some throwing athletes due to stretching of anterior capsule it can lead to shoulder dislocation which is called microtraumatic dislocation [1,2].
Recurrent Dislocating tendency patients present with more than three dislocation episodes. The first dislocation post heavy traumatic injury is followed by less distressful episodes. Few of these patients are able to reduce (put back the dislocated shoulder) on their own or with some assistance [2-4]. Young patients or the ones involved with heavy and active sport activities need surgical intervention to stabilise the same. Among the widely available options to treat recurrent shoulder dislocation, some are anatomic repairs and some are non-anatomic repairs.
In anatomical repair the detached capsule and labrum are repaired back to glenoid whereas in non-anatomical repair strengthening of anterior part of joint is done by different means.
In Modified Boytchev procedure rerouting the tip of coracoid process with conjoint tendon is done under subscapularis. Arthroscopic Bankart repair involves reattaching the over stretched or torn labrum and capsule with suture anchors [1,2,4].
The evidence regarding the relative effectiveness of modified boytchev vs arthroscopic bankart repair of recurrent anterior gleno-humeral instabilities remains unclear. The aim of this present study was to compare both of these procedures in terms of postoperative pain, movement and functional score and recurrence rates.
Materials and Methods
This Hospital based prospective observational study was carried out at the Department of Orthopaedic Surgery, SSKM Hospital and IPGME&R, Kolkata, West Bengal, India during the period of 20 months between January 2015 and August 2016.
Calculation of sample size: Based on past three years data, with in the study period, total number of operations by our unit for Anterior Shoulder dislocation was expected 100. As per published literature the most common type of dislocation is the anterior one approximating with 97% cases of all.
Considering 97% as prevalence, and 95% confidence interval, and 5% as margin of error, the sample size (n) was calculated as 30 using the formulae (Equation-1) with sample size correction (Equation-2) for small study population.
n_0=(Z^2*p*q)/l^2 ………..Equation-1
final sample size (n)=n_0/(1+ ((n_0-1))/N)……….Equation-2
Here, Z=1.96, p=prevalence (97%), q=1-p, l (Margin of error)=5, N=Study population (100)
Sample population, 15 for each operative procedure were selected consecutively for comparison purpose. Present study was mainly observational and descriptive in nature and more concerned with the generalisability of the findings, so authors did’nt go for power analysis since the statistical parametric hypothesis testing was not done.
Sample size was fixed at 30 cases total which were allocated in each group alternatively; 15 patients in each group after obtaining consent. Ethical committee clearance was taken from our institution (MEMO NO – INST/IEC/2015/094R DATED 15.01.2015).
All the cases of traumatic instability of shoulder who attended the outpatient department were judged by the following criteria to decide whether to include them or exclude them from the study group.
Inclusion criteria: Adult age group, recurrent anterior shoulder dislocation (>3 times), date of injury >3 weeks.
Exclusion criteria: Posterior instability, multi-directional instability, HILL-SACHS >25% of humeral head, bony bankart >25%, associated with cuff tear, Neuromuscular disorders and degenerative changes.
Study Procedure
The patients were asked to give a detailed history on the following points: Date of the first trauma incident/approximate time if exact date is not remembered (and therefore calculating the time duration between index injury and seeking of treatment), Nature of trauma. The relocation event: done when, by whom and how, Postreduction immobilisation, if any, and its nature, duration of immobilisation, Any history of shoulder exercise/ rehabilitation/physiotherapy at the end of immobilisation period. Any subsequent episode of dislocation, total number of such dislocations if at all.
Study parameters- Side and number of dislocations, X-ray of the shoulder joint -pre and postoperative, preoperative MRI, range of motion of shoulder joint preoperative and postoperative, any recurrence and final functional comparison done by CMS.
After selection of the patients X-rays and MRIs were done and after getting anaesthetic clearance we proceeded for surgery.
Radiological Studies
X-Ray: Antero-posterior view of shoulder in 30° internal rotation, axillary lateral view and Stryker notch view of the affected shoulder was done to exclude any major bony pathology like Hill-Sachs and bony bankart lesion [2-4].
MRI: The Bankart lesion, which is essentially avulsion of antero-inferior glenoid labrum from the glenoid rim, was confirmed and any contusion of the posterior aspect of the humeral head (Hill-Sachs lesion) or any other associated pathology was also looked for, like a subtle fracture, rotator cuff pathologies, Humeral Avulsion of the Glenohumeral Ligament (HAGL) lesions, subscapularis tendon tear, posterior capsular lesions, degenerative changes and Superior Labral Anterior to Posterior (SLAP) lesions [4,6,7].
Cases Managed by Modified Boytchev Technique [2-4]
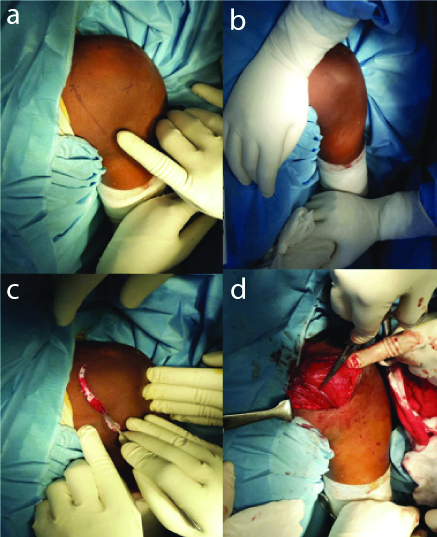
Patient positioning: Operation done under general anaesthesia [Table/Fig-1a] in supine position [Table/Fig-1b] through deltopectoral approach [Table/Fig-1c]. The anterior margin of deltoid muscle was exposed and sectioned transversely near its origin [Table/Fig-1d], while the pectoralis major was retracted medially to expose the horizontal part of the coracoid process [Table/Fig-2a].
Position of the patient, incision and exposure.
Retraction of pectoralis, drilling hole, creating tunnel in subscapularis and screw insertion.
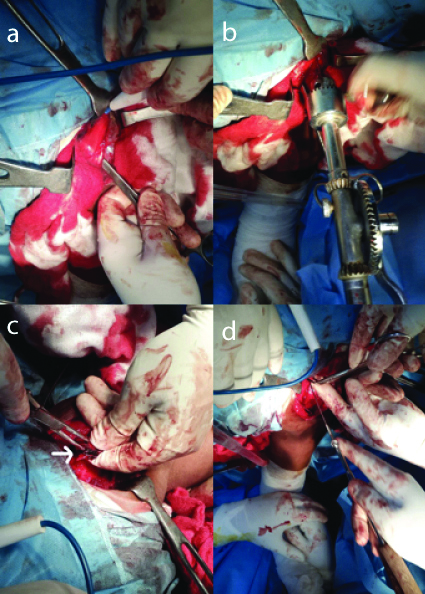
Drill-holing: The anterior end of horizontal part of the coracoid process along its axis is entered through an antero-posterior drill hole [Table/ Fig-2b]. Taking care to protect the musculo-cutaneous nerve, the anterior 2 cm of the coracoid process, along with the tendinous origin of the short head of biceps and the coracobrachialis was osteotomised and mobilised distally.
A tunnel between the shoulder capsule and the subscapularis muscle was created by splitting the fibres of the subscapularis muscle just proximal to its lower border, taking care not to damage the anterior circumflex humeral vessels [Table/Fig-2c]. The isolated coracoid process was passed through and fixed to the predrilled proximal counterpart of the coracoid process with a proper length 3.5 mm AO screw [Table/Fig-2d] while the arm was maintained in full internal rotation.
Closure: After haemostasis wound closure done with a suction drain, the arm was immobilised in complete internal rotation.
Postoperative management and rehabilitation: First dressing changed at 48 hours. Follow-up after 14 days for stitch removal with a plain X-ray of the operated shoulder, antero-posterior and lateral view. Rehabilitation and exercises started after stich removal.
Cases Managed by Arthroscopic Bankart Repair [6,7]
Patient positioning: Operated in the lateral decubitus. The usual mode of anaesthesia was interscalene block followed by general anaesthesia. The shoulder was positioned in 60° of abduction and 10° of flexion.
Posterior portal placement: The posterior portal was made in the “soft spot” about 2 cm inferior and 2 cm medial to the postero-lateral angle of the acromion.
Anterior portal: We placed the anterior portal by outside-in technique.
Preparation of the scapular neck: Introducing a sharp chisel/elevator the labrum was peeled off the bone. The bone surface was roughened with a rasp. Typically, we used three positions for suture anchors at 1, 3 and 5 o’clock for a right shoulder, and 11, 9 and 7 o’clock for left.
Drill-holing and anchor placement: Drill holes for the suture anchors were placed through the glenoid articular surface approximately 1 to 2 mm from the lateral glenoid margin, on the face of glenoid, and always using drill-sleeves [Table/Fig-3]. As mentioned, usually three anchors were placed [Table/Fig-3]. The most inferior (and the most difficult) anchor was placed earliest.
Fixation of anchors, taking bite in the anterior capsule and placing the knots.
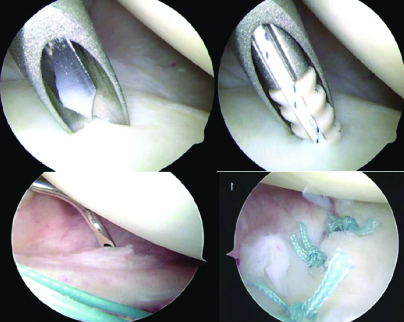
Suture-passing: While taking the bite, it was important that a considerable amount of labral tissue was roped in, to get the ‘nice and round’ bump. On taking a satisfactory bite, a limb of the suture anchor was caught by the retriever in the same go and brought out through the tissue. This would serve as the future ‘post’. Now, a suture retriever (without hook) was introduced through the antero-inferior portal and both limbs were taken out. We were ready for knot-tying [Table/Fig-3].
Knot tying: First, traction was applied to eliminate any twist in the limbs. The strand that came through the tissue was the post. The threads were adjusted so that post was one third and the knotting strand was two third in relative length. A half hitch was then placed and pushed through the knot pusher right inside. This first knot brought the labrum to the glenoid. The knot was secured by ‘past-pointing’. Then, another half-hitch was given in the same direction. A total of 6 half hitches were given [6-8]. The above process was repeated for the other two anchor placements [Table/Fig-3].
Closure: Portals were closed with one or two bites of monofilament sutures. Arm sling applied.
Postoperative management: First dressing changed at 48 hours. Follow-up after 14 days for stitch removal with a plain X-ray of the operated shoulder, antero-posterior and lateral view. Finger, wrist and elbow mobilisation started as soon as the effect of anaesthesia wanes away. Pendulum exercises started from 2nd postoperative day. Upto 90° abduction allowed in two weeks. Full abduction achieved in four weeks and rotational exercises started after four weeks. Patients were advised to wear the sling upto four weeks.
Statistical Analysis
The quantitative data were collected in Microsoft Excel software and was analysed using SPSS version 25. Data were represented using tables and graphs. Chi-Square test was used to ascertain statistical significance between categorical variables. The p-value <0.05 were considered as significant association.
Results
The mean age group of the cases operated by arthroscopic bankart was around 25 with the lowest age being 18 as was decided by selection criteria and highest being 39 [Table/Fig-4].
Distribution of mean age in two groups.
| Group | Number | Mean | SD | Minimum | Maximum | Median | p-value |
|---|
| ARTH.BAN. | 15 | 25.3333 | 5.6146 | 18 | 39 | 25 | 0.1605 |
| MOD.BOY. | 15 | 22.6667 | 4.4508 | 18 | 32 | 22 |
Insignificant p-value (0.456) again shows that the two groups were similar with regards to their side distribution. On the whole among 30 cases 40% had pathology on the left side and 60% on the right side [Table/Fig-5].
Distribution of pathological side in two groups.
| Side | |
|---|
| Sur#Done | Left | Right | Total |
|---|
| ARTH.BAN. | 5 | 10 | 15 |
| Row % | 33.3 | 66.7 | 100 |
| Col % | 41.7 | 55.6 | 50 |
| MOD.BOY. | 7 | 8 | 15 |
| Row % | 46.7 | 53.3 | 100 |
| Col % | 58.3 | 44.4 | 50 |
| Total | 12 | 18 | 30 |
| Row % | 40 | 60 | 100 |
| Col % | 100 | 100 | 100 |
ROW=The calculated percentage of the value among row; COL=The calculated percentage of the value among column.
Out of 15 cases there was no general surgical complication in the arthroscopic bankart group whereas 2 out of 15 (13.3%) had superficial infection which responded to oral antibioitics and healed completely. These two were the cases for which surgical time was greater than two hours in modified boytchev group. They had to stay in the hospital for a longer duration and the outcome of CMS was also decreased as compared to other cases. This probably shows the increased chance of infection with open procedures and more so with increased duration of surgery. No neuro vascular injury or any other general surgical complication apart from superficial infection was encountered by us in present study [Table/Fig-6].
Distribution of general surgical complication in two groups.
| SUR#DONE |
|---|
| Complication | ARTH.BAN. | MOD.BOY. | Total |
|---|
| Number | 15 | 13 | 28 |
| Row % | 53.6 | 46.4 | 100 |
| Col % | 100 | 86.7 | 93.3 |
| Superficial infection | 0 | 2 | 2 |
| Row % | 0 | 100 | 100 |
| Col % | 0 | 13.3 | 6.7 |
| Total | 15 | 15 | 30 |
| Row % | 50 | 50 | 100 |
| Col % | 100 | 100 | 100 |
ROW=The calculated percentage of the value among row; COL=The calculated percentage of the value among column. Chi-square value: 2.1429, p-value: 0.1432359093
Out of 15 patients in arthroscopic group 2 (13.4%) had recurrence, one had apprehension and one had mild subluxutation. The patient having an apprehension gave a history of trauma postoperatively to the affected shoulder due to his negligence at home so may be that trauma attributed to the recurrence in the case. Out of 15 patients in modified boytchev group only 1 (6.7%) had recurrence with positive apprehension. This data probably shows the decreased rate of recurrence in modified boytchev attributing to the greater resistance to dislocation it imparts by its non-anatomic technique [Table/Fig-7].
Distribution of recurrence in two groups. ROW= The calculated percentage of the value among row; COL= The calculated percentage of the value among column.
| SUR#DONE |
|---|
| Recurrence | ARTH.BAN. | MOD.BOY. | Total |
|---|
| A=Apprehension positive | 1 | 1 | 2 |
| Row % | 50 | 50 | 100 |
| Col % | 6.7 | 6.7 | 6.7 |
| N= No recurrence | 13 | 14 | 27 |
| Row % | 48.1 | 51.9 | 100 |
| Col % | 86.7 | 93.3 | 90 |
| S= Subluxation positive | 1 | 0 | 1 |
| Row % | 100 | 0 | 100 |
| Col % | 6.7 | 0 | 3.3 |
| Total | 15 | 15 | 30 |
| Row % | 50 | 50 | 100 |
| Col % | 100 | 100 | 100 |
Chi-square value: 1.0370, p-value: 0.5954
The distribution of the preoperative external rotation was similar in both the groups (insignificant p-value – 0.0844). The mean preoperative external rotation in the arthroscopic bankart group was around 37 degrees and 40 degrees in the modified boytchev group [Table/Fig-8].
Distribution of mean external rotation preoperative in two groups.
| Group | Number | Mean | SD | Minimum | Maximum | Median | p-value |
|---|
| ARTH.BAN. | 15 | 37.3333 | 5.3807 | 30.0000 | 46.0000 | 36.0000 | 0.0844 |
| MOD.BOY. | 15 | 40.2667 | 3.3693 | 36.0000 | 48.0000 | 40.0000 |
The comparison of the final external rotation showed a significant difference between the two groups (significant p-value- 0.006). The mean final external rotation was higher in the arthroscopic bankart group with 71.6 degrees as compared to 63.733 degrees in the modified boytchev group [Table/Fig-9]. The preoperative CMS was distributed similarly in both the groups (insignificant p-value- 0.1518) [Table/Fig-10]. The comparison between the CMS at six months postoperative was significant (p-value-0.0456) between the two groups [Table/Fig-11].
Distribution of mean external rotation final in two groups.
| Group | Number | Mean | SD | Minimum | Maximum | Median | p-value |
|---|
| ARTH.BAN. | 15 | 71.6000 | 8.2184 | 48.0000 | 78.0000 | 74.0000 | 0.0060 |
| MOD.BOY. | 15 | 63.7333 | 6.1350 | 50.0000 | 70.0000 | 66.0000 |
Distribution of mean CMS preoperative in two groups.
| Group | Number | Mean | SD | Minimum | Maximum | Median | p-value |
|---|
| ARTH.BAN. | 15 | 45.3333 | 6.2868 | 36.0000 | 58.0000 | 44.0000 | 0.1518 |
| MOD.BOY. | 15 | 48.2667 | 4.4636 | 40.0000 | 58.0000 | 49.0000 |
Distribution of mean CMS six months in two groups.
| Group | Number | Mean | SD | Minimum | Maximum | Median | p-value |
|---|
| ARTH.BAN. | 15 | 79.4000 | 11.9929 | 56.0000 | 95.0000 | 80.0000 | 0.0456 |
| MOD.BOY. | 15 | 71.0000 | 9.8995 | 55.0000 | 91.0000 | 71.0000 |
The comparison of the final CMS between the two groups also came out to be very significant with the arthroscopic bankart group having a mean of 90.2667 as compared to modified boytchev group having a mean of 83.6667. Though there were two cases of recurrence as compared to one case in modified boytchev technique, the increased final CMS overall in the arthroscopic bankart shows the increased range of motion and better shoulder function the patients have as compared to modified boytchev group [Table/Fig-12]. Finally, there were 9 excellent (60%), 4 good (26.7%), 1 fair (6.7%) and 1 poor (6.7%) CMS grading in arthroscopic bankart group [Table/Fig-13]. In modified boytchev group there were 6 excellent (40%), 6 good (40%), 3 fair (20%) and 0 poor CMS grading.
Distribution of mean CMS final in two groups.
| Group | Number | Mean | SD | Minimum | Maximum | Median | p-value |
|---|
| ARTH.BAN. | 15 | 90.2667 | 8.6970 | 66.0000 | 98.0000 | 95.0000 | 0.0363 |
| MOD.BOY. | 15 | 83.6667 | 7.7152 | 71.0000 | 92.0000 | 83.0000 |
Distribution of CMS grading in two groups.
| SUR#Done |
|---|
| Grading | ARTH.BAN. | MOD.BOY. | Total |
|---|
| Excellent | 9 | 6 | 15 |
| Row % | 60 | 40 | 100 |
| Col % | 60 | 40 | 50 |
| Fair | 1 | 3 | 4 |
| Row % | 25 | 75 | 100 |
| Col % | 6.7 | 20 | 13.3 |
| Good | 4 | 6 | 10 |
| Row % | 40 | 60 | 100 |
| Col % | 26.7 | 40 | 33.3 |
| Poor | 1 | 0 | 1 |
| Row % | 100 | 0 | 100 |
| Col % | 6.7 | 0 | 3.3 |
| Total | 15 | 15 | 30 |
| Row % | 50 | 50 | 100 |
| Col % | 100 | 100 | 100 |
ROW=The calculated percentage of the value among row; COL=The calculated percentage of the value among column
Discussion
The aim of the study was to evaluate the efficacy and functional outcomes of modified boytchev vs arthroscopic bankart repair in recurrent shoulder dislocation. So, in present study the average age and the male predominance of the study population is comparable to study done by Chatterjee ND et al., may be because both studies are conducted in eastern part of the country [2].
In this study, right side was commonly affected which is supported by studies done by Garg AK et al., and Chandra R et al., [3,4]. The mean number of dislocations was around seven in his study population. Study done by Garg AK et al., had a slightly higher mean dislocation number of 18.22±12.08, this might be due to slightly higher study population in them [3].
In present study, 2 patients out of 15 operated by modified boytchev group had superficial infection which was resolved by antibiotics. The rate of infection in this study was comparable to studies of Chatterjee ND et al., (5 out of 42) and Garg AK et al., (4 out of 48) [2,3], however in contrast to these studies there was no neurovascular injury in present study as we had followed strict measures and safety intraoperatively to avoid that.
In the meta-analysis study done by Lenters TR et al., they also found that arthrsoscopic procedures had more rates of recurrent instability as compared to open procedures like modified boytchev which supports findings of this study also [6]. The mean final external rotation was higher in the arthroscopic bankart group which is similar to the findings of the study by Jorgensen U et al., done in Copenhagen [7].
In this study, the comparison of the final CMS between the two groups also came out to be very significant (p-value 0.036) with better score in the arthroscopic bankart group. This findings are comparable to the findings of the studies [6-9] wherein the functional shoulder scores were better in the arthroscopic group, this might be because arthroscopy being a minimal invasive procedure so the iatrogenic tissue damage and postoperative stiffness is minimum.
Limitation(s)
The limitation of this study is the deficiency of a long term follow-up and inability to include large number of patients.
Conclusion(s)
From all the observations it can be concluded that the modified boytchev technique, a time tried and trusted technique and arthroscopic bankart repair technique, a technique derived from the modern era of arthroscopic orthopaedic surgery are efficient techniques and do their job commendably in cases of recurrent dislocation of shoulder.
In today’s world where young individuals especially females, give importance to cosmesis; arthroscopic procedures lie at an advantage over open procedures like modified boytchev where there is a long scar as compared to small healed entry port sites.
Also, in this study the rate of infection was more in modified boytchev technique due to it being an open procedure, the postoperative external rotation was restricted and CMS were lower when compared to arthroscopic bankart repair; but it had a lower rate of recurrence when compared to arthroscopic group.
Modified boytchev technique still provided the patients a reasonable function and relief at low cost when compared to the costly and technically demanding arthroscopic surgery specially in respect to Indian patients, but a study with a greater number of subjects and a longer follow-up would have given a stronger evidence.
ROW=The calculated percentage of the value among row; COL=The calculated percentage of the value among column.
ROW=The calculated percentage of the value among row; COL=The calculated percentage of the value among column. Chi-square value: 2.1429, p-value: 0.1432359093
Chi-square value: 1.0370, p-value: 0.5954
ROW=The calculated percentage of the value among row; COL=The calculated percentage of the value among column