Ocular Surface Squamous Neoplasia: Monotherapy with Mitomycin C
Manu Sharma1
1 Medical Officer, Department of Health and Family Welfare, Civil Hospital, Kangra, Himachal Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Manu Sharma, Village and Post Office Gaggal, Tehsil and District Kangra, Kangra-176209, Himachal Pradesh, India.
E-mail: drmanu.sharma26@gmail.com
Ocular Surface Squamous Neoplasia (OSSN) is a neoplasm of ocular surface present in the interpalpebral area having feeder vessel. It is more common in middle age group and present as a mass lesion or chronic ocular irritation. Treatment is chemo reduction, surgical excision, cryotherapy and excision with adjuvant chemotherapy. There is high rate of recurrence in OSSN. Here, a case of 79-year-old female patient with painless mass over conjunctiva and cornea was presented. The mass was whitish, shiny and placoid extending from 9 o’clock to 5 o’clock position covering half of the corneal surface with feeder vessel. Gelatinous or leucoplakic OSSN was managed with chemoreduction and monotherapy with mitomycin C. No recurrence was reported during more than 2 years follow-up at the peripheral health institution.
Chemoreduction, Cryotherapy, Ocular squamous neoplasia
Case Report
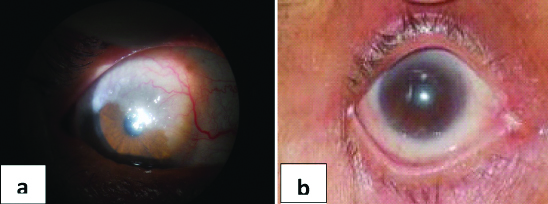
A 79-year-old female presented at peripheral health institution in May 2017 with complaints of enlarging painless mass over conjunctiva and cornea of right eye since 4 months. It was associated with redness, watering and progressive diminution of vision in the right eye since 4 months duration. She consulted many private clinics and even medical college but, they all referred her to higher centre. Due to financial reasons, she was not able to visit higher centre and came for opinion at peripheral health institution. There was no relevant systemic and family history. On examination of right eye, 6/60 visual acuity with whitish, shiny, placoid mass lesion was present on conjunctival and corneal surface extending from 9 o’clock to 5 o’clock position, covering half of the corneal surface with feeder vessel [Table/Fig-1a] and clinically making possibility of gelatinous OSSN. Rest of the details like anterior chamber, lens status and fundus examination was normal. Left eye examination was normal. So, from the history and examination, final diagnosis of gelatinous OSSN was made. Treatment with Mitomycin-C 0.04% i.e., chemoreduction alone, in week on-week off cycles for 6 weeks was done. Mitomycin was prepared weekly and given to patient (kept in refrigerator). During treatment, side effects of mitomycin-C like conjunctival hyperemia and superficial punctate keratitis were noticed and managed with lubricants. Lesion was completely resolved within 6 weeks period [Table/Fig-1b] with no recurrence in more than 2 years of follow-up.
a) Pre-treatment photograph showing placoid mass lesion extending from 9 o’clock to 5 o’clock with feeder vessel; b) Post-treatment photograph showing complete resolution of lesion.
Discussion
OSSN ranges from dysplastic lesions to invasive Squamous Cell Carcinoma (SCC) of cornea and conjunctiva [1]. There are numerous risk factors, including immunosuppression, genetic predisposition, ultraviolet exposure, Human Papillomavirus infection (HPV infection) and smoking which have been related with OSSN [1]. It is mostly unilateral, seen in middle age and older patients. OSSN most commonly present near the limbus in the interpalpebral area. Both bulbar and palpebral conjunctiva can be involved although involvement of bulbar conjunctiva is much more common. As in present case, patient was old age and lesion was near the limbus, in interpalpebral area, involving both cornea and conjunctiva. It may present with well defined margins or poorly demarcated as in diffuse variety making identification very difficult. Dilated feeder vessels are usually seen. Patient may present with symptoms due to ocular surface mass like chronic ocular irritation, foreign body sensation and redness or asymptomatic [2].
Morphologically, three types of lesions are seen: 1) Gelatinous type (leukoplakic or papilliform) has shiny velvety surface and tufted vessels. 2) Nodular type is elevated well circumscribed focal mass with mulberry appearance; 3) Diffuse type exhibit radial growth pattern in which margins are not well defined and it imitates like chronic blepharoconjunctivitis. These lesions are indolent, usually slow growing and prone to recurrences [3]. Diagnosis usually made by Impression cytology, Histopathology, Ultrasound Biomicroscopy (UBM), Anterior Segment Optical Coherence Tomography (ASOCT), Confocal microscopy and Magnetic resonance imaging (MRI) orbit for advanced tumours with proptosis [4-6] In the present case, diagnosis was made only on clinical basis, as all these diagnostic modalities were not available. Treatment consists of surgical treatment, cryotherapy, radiotherapy and medical therapy. Medical therapy includes topical chemotherapy with Mitomycin-C (MMC), 5-Fluorouracil (5-FU) and immunotherapy with interferon-alpha 2b [7]. MMC is an anti-metabolite that alkylates DNA and disrupts the production of RNA, isolated from streptomyces caespitosus and it is an effective treatment for OSSN. MMC for OSSN is administered as topical medication as, it is relatively unstable in solution, therefore requires refrigeration and weekly replacement of the medication. In the present case, authors used sole therapy with mitomycin C as other options were not accessible. Although, there was minimal data suggesting of cases treated with mitomycin C chemotherapy alone, in review of literature [8-10] Gupta A and Muecke J, in their prospective study on OSSN, included 91 primary or recurrent Conjunctival-Corneal Intraepithelial Neoplasia (CCIN) lesions [8]. Out of these, 73 cases of localised non-invasive CCIN and eight cases of recurrent CCIN were treated with surgical excision and/or cryotherapy followed by adjuvant topical chemotherapy with mitomycin C (0.04% four times a day for two to three 1 week cycles) and 10 cases of diffuse CCIN were treated with mitomycin monotherapy (0.04% two-three 1 week cycles as primary treatment). Hirst LW included 48 patients of biopsy proven non-invasive OSSN in their study [9]. Twenty patients were given placebo drops and showed no improvement, 24 of 26 resolved completely with mitomycin C (0.4 mg/ml) used four times a day for three week. Recurrence was seen only in 2 patients with no side effects of topical mitomycin C. Frucht Pery J et al., and Daniell M et al., used mitomycin C monotherapy for OSSN in 0.02% or 0.04% concentrations [10,11]. Only 2 cases of OSSN had recurrence and few side effects of topical mitomycin C like conjunctival hyperemia and ocular allergy was observed. These were self limiting and no serious side effects like scleral melt were noticed. The two main dosages used for treatment are 0.02%, which is given continuously for 28 days or until clinical resolution, or 0.04%, given in week on- week off cycles until resolved [10,11]. Recurrence rate with these treatment strategies has ranged between 0 and 17%. Time to resolution ranged from 4 days to 14 weeks, with an average of 4-5 weeks for resolution. As in the present case, mitomycin C (0.04%) monotherapy alone in 6 week period (week on-week off cycle means 3 weeks of drug) lead to complete resolution of OSSN with no residual drug related side effects. MMC has thus been found to be effective as primary treatment for OSSN. Serious side effects particularly scleral melt and limbal stem cell deficiency have been reported during previous uses in pterygium and glaucoma surgery. Other side effects include Conjunctival hyperemia, ocular allergy, superficial punctate keratitis, ocular pain and epiphora were self limiting [11-13].
Conclusion(s)
Mitomycin C chemoreduction alone can achieve success in treatment of OSSN and one must try it as sole therapy when other resources are not available.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Feb 04, 2020
Manual Googling: May 11, 2020
iThenticate Software: May 23, 2020 (13%)
[1]. Lee GA, Hirst LW, Ocular surface squamous neoplasiaSurv Opthalmol 1995 39:429-50.10.1016/S0039-6257(05)80054-2 [Google Scholar] [CrossRef]
[2]. Basti S, Mascal MS, Ocular surface squamous neoplasiaCornea 2003 22(7):687-704.10.1097/00003226-200310000-0001514508267 [Google Scholar] [CrossRef] [PubMed]
[3]. Rudkin A, Dodd T, Mueske JS, The differential diagnosis of localised amelanotic limbal lesions: A review of 162 consecutive excisionsBr J Ophthalmol 2011 95(3):350-54.10.1136/bjo.2009.17218920837790 [Google Scholar] [CrossRef] [PubMed]
[4]. Nolan GR, Hirst LW, Wright RG, Application of impression cytology to the diagnosis of conjuctival neoplasmsDiag Cytopathol 1994 11:246-49.10.1002/dc.28401103107867466 [Google Scholar] [CrossRef] [PubMed]
[5]. Kieval JZ, Karp CL, AbouShousha M, Galor A, Hoffman RA, Dubovy SR, Ultra-high resolution optical coherence tomography for diffrentiation of ocular surface squamous neoplasia and pterygiaOphthalmology 2012 119(3):481-86.10.1016/j.ophtha.2011.08.02822154538 [Google Scholar] [CrossRef] [PubMed]
[6]. Xu Y, Zhou Z, Xu Y, Wang M, Liu F, Qu H, The clinical value of in vivo confocal microscopy for diagnosis of ocular surface squamous neoplasiaEye 2012 26(6):781-87.10.1038/eye.2012.1522402703 [Google Scholar] [CrossRef] [PubMed]
[7]. Mittal R, Rath S, Vemuganti GK, Ocular surface squamous neoplasia- Review of etio-pathogenesis and an update on clinico-pathological diagnosisSaudi J Ophthalmol 2013 27:177-86.10.1016/j.sjopt.2013.07.00224227983 [Google Scholar] [CrossRef] [PubMed]
[8]. Gupta A, Muecke J, Treatment of ocular surface squamous neoplasia with mitomycin CBr J Ophthalmol 2010 94(5):555-58.10.1136/bjo.2009.16829420447963 [Google Scholar] [CrossRef] [PubMed]
[9]. Hirst LW, Randomised Controlled trial of topical miyomycin C for ocular surface squamous neoplasia: Early resolutionOphthalmology 2007 114(5):976-82.10.1016/j.ophtha.2006.09.02617241666 [Google Scholar] [CrossRef] [PubMed]
[10]. Frucht-Pery J, Sugar J, Baum J, Sutphin JE, Pe’er J, Savir H, Mitomycin C treatment for conjunctival- Corneal intraepithelial neoplasia: A multicenter experienceOphthalmology 1997 104(12):2085-93.10.1016/S0161-6420(97)30055-4 [Google Scholar] [CrossRef]
[11]. Daniell M, Maini R, Tole D, Use of mitomycin C in the treatment of corneal conjunctival intraepithelial neoplasiaClin Exp Ophthalmol 2002 30:94-98.10.1046/j.1442-6404.2002.00497.x11886411 [Google Scholar] [CrossRef] [PubMed]
[12]. Wilson MW, Hungerford JL, George SM, Madreperla SA, Topical mitomycin C for the treatment of conjuctival and corneal epithelial dysplasia and neoplasiaAm J Ophthalmol 1997 124:303-11.10.1016/S0002-9394(14)70822-0 [Google Scholar] [CrossRef]
[13]. Nanji AA, Sayyad FE, Karp CL, Topical chemotherapy for ocular surface squamous neoplasiaCurr Opin Ophthalmol 2013 32:1558-61. [Google Scholar]