Haemospermia- A Disorder of Male Sexual Health
Dwijesh Kumar Panda1
1 Consultant Lymphologist, Pathologist and Microbiologist, Department of Pathology and Medicine, Sanaria Lymphology Clinic and Research Centre, Bhubaneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dwijesh Kumar Panda, M5/12, Acharya Vihar, Bhubaneswar-751013, Odisha, India.
E-mail: doctordwijesh@gmail.com
The testicular involvement with lymphatic filariasis caused by Wuchereria bancrofti (95%) is common in the endemic zone of Odisha in India. Haemospermia is the presence of blood in ejaculation. It is relatively uncommon and may affect one in every 5,000 individuals. Blood in semen can be frightening, but the condition is usually benign. A case of haemospermia was presented with the complaint of pain and discomfort in the perineum for the last five years. Trans Rectal Ultrasonography (TRUS) did not reveal any pathology. The Contrast-Enhanced Magnetic Resonance Imaging (CE-MRI) showed haemorrhage in the left seminal vesicles. The serum Prostate-Specific Antigen (PSA) test was within the reference range and carcinoma of the prostate was ruled out. The positive monoclonal circulating adult filarial antigen test (OG4C3) confirmed the diagnosis. The patient was given anti-filarial treatment for six months. Blood in the semen disappeared, but sexual asthenia persisted.
Funiculitis, Seminogram, Seminal vesicle
Case Report
A 28-year-old unmarried male, the resident of Odisha, an endemic zone of lymphatic filariasis, presented to a urology clinic in January 2015 with the complaint of yellowish-red ejaculate, pain and discomfort since two months. He was advised to take Ofloxacin, a Fluoroquinolone antibiotic 400 mg twice daily after food for 10 days. The symptoms of pain and discomfort were relieved for one month and again after one month patient was unable to walk and drive for a period of five months. So, he consulted another urologist towards end of 2015 and got relieved. But the tenderness of the epididymis persisted along with yellowish-red ejaculate. In the meantime, he was treated by three medical, two Ayurvedic, and one homeopathic practitioner but there was no improvement.
In January 2018, patient reported to the author at Lymphology clinic with chief complaints of pain and discomfort in the perineum, unable to walk, drive and loss of libido. He observed 10 to 12 episodes of haemospermia during this interval of two years which increased frequently aggravating the suffering. The past and family history was not relevant. He was afebrile, non-diabetic and normotensive. Inspection revealed bilateral mild swollen testis and epididymis. On palpation, the spermatic cord, testis, and epididymis found tender on both sides. Both the testis and epididymis centrally placed without deviation and adherence to the surrounding tissue. Prothrombin Time (PT/INR) was 12 seconds (Normal- 10-14 secs) and INR 1.2. The activated Partial Thromboplastin Time (aPTT) was 28 secs (Normal- 25 to 36 secs). Both tests were done to rule out bleeding diathesis. Seminal fluid analysis was done. The rating was fertile with the presence of good numbers of red blood cells mixed with some pus cells. Detail investigations of blood, such as lipid profile, fasting blood sugar with HbA1C, liver function tests, and renal function tests were done after taking return informed consent from the patient and tests report were normal. TRUS and CE-MRI of the pelvis were done to find out the pathology.
TRUS revealed a healthy prostate. The bilateral seminal vesicles were enlarged in size with heterogeneous hypoechoic parenchymal echo and multiple internal cysts. The features were suggestive of bilateral chronic seminal vesiculitis. The sonographic evaluation of the abdomen and pelvis (Especially Genito-Urinary System) revealed normal conditions, as illustrated in [Table/Fig-1].
Trans Rectal Ultrasonography (TRUS) showing normal conditions.
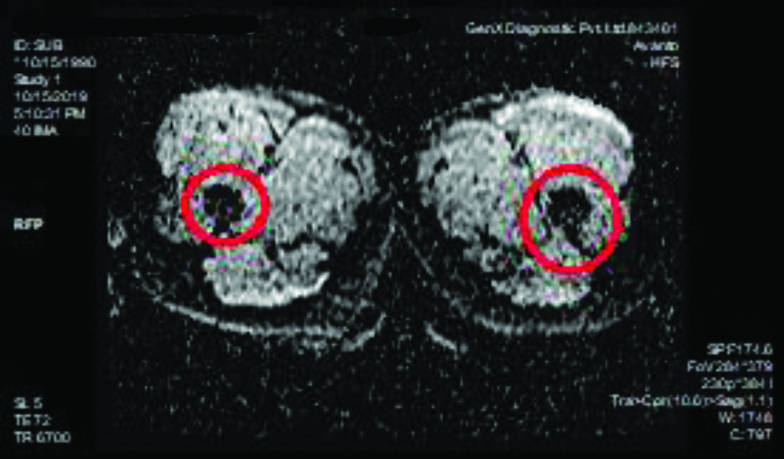
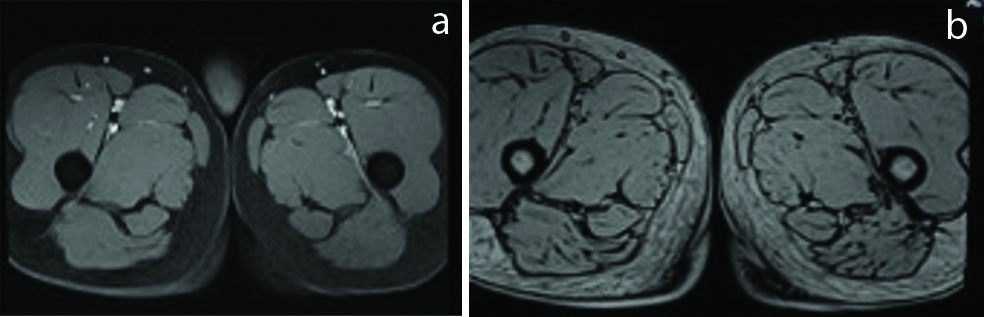
CE-MRI of the pelvis revealed haemorrhage in the left seminal vesicle [Table/Fig-2] and prostate appeared normal [Table/Fig-3].
Haemorrhage in the left seminal vesicle (red circles).
CE-MRI pelvis showing normal prostrate.
The Nucleic Acid Amplification Test (NAAT) of seminal fluid did not detect the nucleic acid sequence of Mycobacterium tuberculosis. The culture of semen was done and Enterococcus spp. was isolated. The count was 10,000 CFU/ML and sensitive to Linezolid, Vancomycin, and Teicoplanin. Urine culture was sterile. The PSA was measured to help detect prostate cancer. The total value was 2.29 ng/mL (Ref. less than 4.00 ng/mL). The serum Alpha-Fetoprotein (AFP) was tested to rule out testicular tumours. The result was 0.1 ng/mL (Ref: 0.5-6.7 ng/mL). The serum testosterone was 324 ng/dL, within the reference range of 164.94-753.38 ng/dL.
The serum adult filarial circulating antigen test OG4C3 (ELISA) was positive in 2048 Antigen Units (AU). (Reference value: up to 128 AU is considered normal). This test confirmed the diagnosis of lymphatic filariasis. All other biochemical and haematological parameters were found to be normal. A provisional diagnosis of Seminal vesiculitis due to Wuchereria bancrofti infection was made. The patient was treated with Doxycycline 200 mg once after dinner for three months, Diethylcarbamazine citrate 100 mg three times daily after food for three weeks and Albendazole weekly once after dinner for one month. Clinical improvement was noticed after one month. Three courses of the regimen were repeated. No relapse reported yet. Clinical symptoms almost disappeared but sexual asthenia persisted.
Discussion
Lymphatic filariasis is the second leading cause of disability worldwide. Globally, 120 million people are infected in 83 countries. It is caused by Wuchereria bancrofti (95%) inhabiting the lymphatic system and causing damage and blockage of the lymphatic vessels [1]. Haemospermia is the presence of blood in ejaculation. It is a benign symptom with many possible causes that often given rise to worry [2]. The probable cause may be a bacterial or parasitic infection. Haemospermia appears in the younger age group from 25 to 40 years of age. So, the chances of malignancy of prostate/seminal vesicles are remote. Erectile and ejaculatory dysfunction is a common disorder of men. Infectious conditions account for approximately 40% of haematospermia cases [3]. The prevalence of haemospermia is estimated at 1:5000 among urological patients [4]. The exact cause cannot be found in as many as 70% of patients because a single episode of haemospermia is usually benign [5]. Infection and inflammation are considered to be the main causes. Neoplasm of the seminal vesicle can present as haemospermia [6]. Systemic diseases (malignant hypertension, liver dysfunction, dyslipidemia or bleeding diathesis) may also be the cause of blood in semen ejaculation. Seminal vesicle dilatation, cyst, or calculi is a strong suspicion of haemospermia. Infection of the testis, epididymis, and spermatic cord is known as orchitis, epididymitis, and funiculitis respectively. All these organs are anatomically continuous with common lymphatics. So the involvement of one organ affects the other three [6]. The infection might have spread to the seminal vesicle to cause silent haemospermia [7].
Seminal vesiculitis was a positive finding in this case. The patient belongs to an endemic zone of lymphatic filariasis, and the moderately positive filarial antigen assay (OG4C3- ELISA) confirms the aetiology. In the present case, the patient was a microfilaraemic. The circulating adult filarial antigen level (2048 AU) helped in the diagnosis. The sensitivity of the test is more than 90% and specificity about 95% [8]. In one study of 282 microfilaremic individuals in Brazil, the sensitivity of the OG4C3 at microfilarial densities of <1, 1 to 30, and >30 microfilariae per mL of blood were 72, 98, and 100%, respectively [9]. The OG4C3 (ELISA) assay can also be used as a cure marker. The serum values of circulating filarial antigen gradually decreased after three months of treatment [10].
TRUS was done to get the picture of organs in the pelvis such as prostate, seminal vesicle and surrounding tissue. CE-MRI helped to visualise the separation of arteries and veins and enhanced the quality of image for more accuracy in the diagnosis.
The patient was treated with Doxycycline for three months and he responded to the treatment, as evidenced by the absence of red blood cells in his ejaculate for the last one year. The cause of sexual asthenia could not be corroborated as the serum testosterone level was normal. However, chronic epididymal-funicular-orchitis might be the cause of sexual asthenia [11].
Conclusion(s)
Haemospermia is often idiopathic and challenging to treat. Adult patients coming from an endemic area of lymphatic filariasis with the symptom of blood in the seminal fluid must be tested for OG4C3 to exclude filarial infection. The diagnosis of inflammatory vesiculitis due to filarial aetiology helped in appropriate treatment in this case. The CE-MRI of the pelvis revealed bleeding in the seminal vesicle. The circulating adult filarial antigen test indicated to reach the diagnosis and provided appropriate treatment.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 13, 2020
Manual Googling: May 05, 2020
iThenticate Software: May 15, 2020 (12%)
[1]. World Health Organization. Global program to eliminate lymphatic filariasis: Progress report, 2017. https://apps.who.int/iris/bitstream/handle/10665/275719/WER9344.pdf?ua=1 (Accessed on July 01, 2019) [Google Scholar]
[2]. Freedman DO, de Almeida Filho PJ, Besh S, Maia e Silva MC, Braga C, Maciel A, Lymphoscintigraphic analysis of lymphatic abnormalities in symptomatic and asymptomatic human filariasisJ Infect Dis 1994 170:92710.1093/infdis/170.4.9277523538 [Google Scholar] [CrossRef] [PubMed]
[3]. Pani S, Pani’s filariasis3rd edNew DelhiJaypee Brothers [Google Scholar]
[4]. Leary FJ, Aguilo JJ, Clinical significance of hematospermiaMayo Clin Proc 1974 49:815-17. [Google Scholar]
[5]. Wilson C, Boyd K, Mohammed A, Little B, A single episode of haemospermia can be safely managed in the communityInt J Clin Pract 2010 64:1436-39.10.1111/j.1742-1241.2009.02242.x20716149 [Google Scholar] [CrossRef] [PubMed]
[6]. Gattoni F, Avogadro A, Sacrini A, Blanc M, Pozzato C, Spagnoli I, Transrectal prostate echography in the study of hemospermia. An assessment of an 85 patient caseloadRadiol Med 1996 91:424-28. [Google Scholar]
[7]. Bhaduri S, Riley VC, Haematospermia associated with malignant hypertensionSex Transm Infect 1999 75(3):20010.1136/sti.75.3.20010448405 [Google Scholar] [CrossRef] [PubMed]
[8]. Lalitha P, Ravichandran M, Suba S, Kaliraj P, Narayanan RB, Jayaraman K, Quantitative assessment of circulating antigens in human lymphatic filariasis: a field evaluation of monoclonal antibody-based ELISA using blood collected on filter stripsTrop Med Int Health 1998 3(1):41-45.10.1046/j.1365-3156.1998.00170.x [Google Scholar] [CrossRef]
[9]. Weil GJ, Ramzy RM, Diagnostic tools for filariasis elimination programsTrends Parasitol 2007 23:7810.1016/j.pt.2006.12.00117174604 [Google Scholar] [CrossRef] [PubMed]
[10]. Rocha A, Addiss D, Ribeiro ME, Norões J, Baliza M, Medeiros Z, Evaluation of the Og4C3 ELISA in Wuchereria bancrofti infection: Infected persons with undetectable or ultra-low microfilarial densitiesTrop Med Int Health 1996 1:859-64.10.1111/j.1365-3156.1996.tb00123.x8980602 [Google Scholar] [CrossRef] [PubMed]
[11]. Trojian TH, LishnTrojian TH, Lishnak TS, Heiman D, Epididymitis and orchitis: An overviewAm Fam Physician 2009 79:583 [Google Scholar]