Retention of Foetal Bone Fragments: A Cause of Secondary Infertility
Olatunji Okikiola Lawal1, Oluwasomidoyin Bello2, Gbolahan Oladele Obajimi3
1 Consultant, Department of Obstetrics and Gynaecology, University College Hospital, Ibadan, Oyo State, Nigeria.
2 Consultant, Department of Obstetrics and Gynaecology, University College Hospital, Ibadan, Oyo State, Nigeria.
3 Consultant, Department of Obstetrics and Gynaecology, University College Hospital, Ibadan, Oyo State, Nigeria.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Gbolahan Oladele Obajimi, PO BOX 29245, Secretariat, Ibadan, Oyo State, Nigeria.
E-mail: gbolahanobajimi@gmail.com
Foetal bone retention is a rare cause of infertility. They act as barriers within the endometrial cavity like an intrauterine device. Nonspecific clinical symptoms such as abnormal uterine bleeding, pelvic pain, vaginal discharge and dysmenorrhea may be present in some patients. Here, the present author reports a case of a 31-year-old female who presented with secondary infertility and a history of recurrent brownish vaginal discharge following voluntary termination of pregnancy 16 years earlier. Ultrasonography was suggestive of bone retention and further evaluation with hysteroscopy confirmed the diagnosis. She had successful removal of bone fragments and she was pregnant 6 months post-removal of bone fragments.
Hysteroscopy, Intrauterine bony fragments, Pelvic pain
Case Report
A 31-year-old P0+1 female presented to the gynaecology outpatient clinic with secondary infertility of 8 years. She got married in 2009 at 23 years and had not achieved conception despite regular unprotected sexual intercourse. She complained of recurrent brownish vaginal discharge of 16 years duration which resolved occasionally following antibiotic therapy and the last episode was about 4 months prior to presentation. She menstruated regularly with no dysmenorrhea and had never used any contraception. She had a history of voluntary termination of a 16-week-old pregnancy when she was 15-year-old. Termination was unsuccessful with intramuscular abortifacients. She subsequently had dilatation and evacuation. The abortion was complicated by haemorrhage and postabortal sepsis. She was transfused with 4 units of blood and had antibiotic therapy. She recovered from the sequelae, but her menses decreased from 5 to 3 days. Prior investigation for infertility at a private clinic did not reveal any abnormality as Hysterosalpingography (HSG), seminal fluid analysis and hormone profile done were deemed normal.
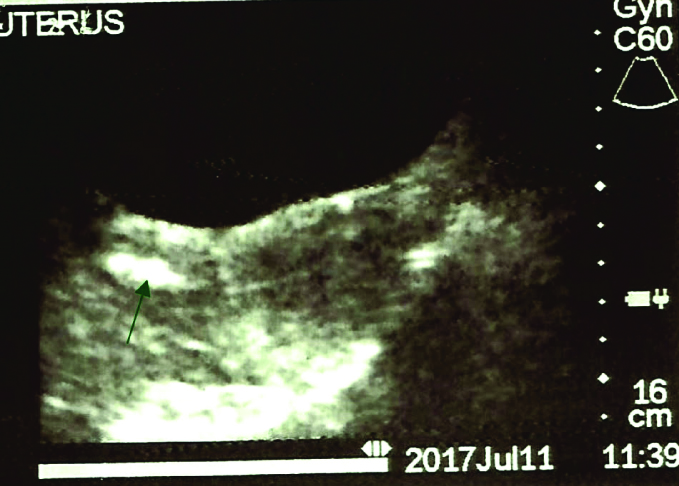
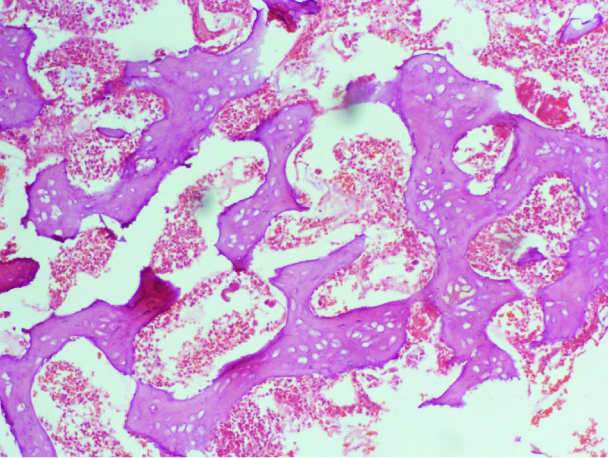
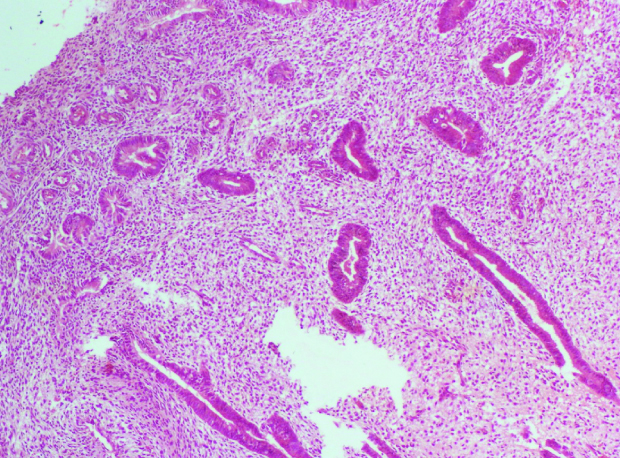
At presentation, speculum examination of the vagina and cervix revealed a smooth cervix; a tiny brownish hard tissue was seen at the external cervical os and sent for histology. Pelvic Ultrasonography (USS) done revealed a normal sized uterus and endocervical plaque probably bone fragment [Table/Fig-1]. Further evaluation of the endometrial cavity by hysteroscopy showed four bony fragments in the endocervical canal, which were removed. Mild adhesions were noted around the fundal region. She recovered without complications. The histology report [Table/Fig-2,3] revealed proliferative endometrium, fragments of bony tissue with marrow elements. She was reviewed at the gynaecological clinic 2 weeks following the procedure and there were no new complaints. At the sixth month, post-hysteroscopy, she presented with amenorrhoea of 6 weeks duration and a positive pregnancy test. Ultrasonography confirmed a viable 6-week intrauterine pregnancy. She was referred to the antenatal clinic for further management and her consent was obtained for the publication of the above findings.
Pelvic ultrasound scan showing bright echoes in the uterine cavity (arrow).
Photomicrograph showing well organised trabeculae of bony tissue (magnification x 100).
Photomicrograph showing predominantly proliferative endometrial glands. Note the cellular stroma. (magnification x 100).
Discussion
This case report highlights the unusual occurrence of secondary infertility following foetal bone retention from complications of unsafe abortion. It emphasises the importance of a detailed history, speculum examination and targeted investigations in the diagnosis and management. It further emphasises the usefulness of hysteroscopy in the evaluation of the uterine cavity in the management of infertility.
Infertility refers to the inability of a couple to achieve conception after twelve months of regular unprotected sexual intercourse. The ability to procreate remains a fundamental part of human existence and couples who are unable to do so, experience both physical and psychological problems from either infertility or its treatment [1]. In the United States of America, about 1.3 million women are treated annually for infertility, while 2% undergo treatment with Assisted Reproductive Technology [2]. In Sub-Saharan Africa, it is estimated that as high as 40% of women may suffer from infertility [3], while in Nigeria, infertile clients account for about 26-48% [4,5]. Unlike high income countries, secondary infertility is more prevalent in low income countries which have a high rate of puerperal sepsis, unsafe abortion, and pelvic inflammatory disease. This has been related to poor obstetric services, restrictive abortion laws, low contraceptive prevalence and poorly treated sexually transmitted infections [6]. In 2012 alone, it was estimated that over one million induced abortions occurred in Nigeria [7] and were mostly carried out in unsafe conditions. Available data also suggest that over a quarter of a million women suffer serious health challenges following unsafe abortion in Nigeria [7].
Bone retention was suspected because the patient had a complicated second trimester abortion, coupled with the removal of a partly expelled bone fragment from the external os. This contrasts with a case series by Graham O et al., where bone retention was suspected following ultrasound diagnosis of abnormal bright echoes within the uterine cavity of eleven women evaluated for infertility [8]. Interestingly, all the women studied were of West African descent, mostly Nigerians, and the unsafe abortions were performed in their countries of origin. Nigeria has a high abortion rate, despite the social, political and religious restrictions. Most of these abortions are done clandestinely by unskilled personnel in unhygienic environments predisposing the women to complications as documented in this report.
The pathophysiology of infertility in bone retention bears similarity to that of an intrauterine contraceptive device in-situ. They affect the physical, chemical, and hormonal milieu in the endometrium of the uterus preventing implantation of an embryo [9]. Other problems that have been reported include abnormal vaginal discharge, pelvic pain and dysmenorrhoea [10]. This patient had a history of recurrent brownish vaginal discharge, but no pelvic pain or dysmenorrhea. Additionally, a study by Izhar R et al., reported heavy menstrual flow as a presenting complaint which was not present in this patient [11].
The diagnosis was confirmed at hysteroscopy, and the remaining bony fragments were removed at the same procedure. Hysteroscopy is the procedure of choice for diagnosis and treatment; however, it is expensive and not widely available in developing countries such as Nigeria. HSG has a limited role in diagnosing retained foetal bone. The pick-up rates are low, and pathologies are easily missed [8]. This patient had HSG which was reported as normal despite the presence of bony fragments, underscoring the irrelevance of HSG in making a diagnosis. In developing countries like Nigeria, ultrasonography is a readily available tool for diagnosis. The patient regained fertility and was pregnant by the sixth month of review post-hysteroscopy. This was similar to findings by Srofenyoh EK et al., in Ghana and Mahdavi A et al., in Iran with return to fertility observed within 6 months of removal of the foetal bony fragments [12,13]. It was suggested that retained foetal bony fragments should be considered an important differential in women presenting with secondary infertility with a history of mid-trimester abortion. An important concern, however, has been the increased incidence of spontaneous miscarriages experienced by patients who conceive following a background history of foetal bone retention [14]. This patient was referred to the antenatal clinic for further specialised care.
Conclusion(s)
Foetal bone retention within the uterine cavity is an unusual cause of secondary infertility. A history of second trimester abortion with ultrasonography suggestive of intrauterine pathology warrants further evaluation of the uterine cavity by hysteroscopy to rule out rare but treatable pathologies such as retained bony fragments. Fecundability improves and fertility usually returns within 6 months following definitive treatment. Hysteroscopy remains an invaluable tool in establishing diagnosis and instituting appropriate care. There is an unmet need for hysteroscopic services in many developed countries, hence the need for advocacy and appropriate health care funding.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 05, 2020
Manual Googling: May 02, 2020
iThenticate Software: May 15, 2020 (9%)
[1]. The psychological impact of infertility and its treatment. Medical interventions may exacerbate anxiety, depression, and stressHarv Ment Health Lett 2009 25(11):01-03. [Google Scholar]
[2]. Katz P, Showstack J, Smith JF, Nachtigall RD, Millstein SG, Costs of infertility treatment: Results from an 18-month prospective cohort studyFertil Steril 2011 95(3):915-21.10.1016/j.fertnstert.2010.11.02621130988 [Google Scholar] [CrossRef] [PubMed]
[3]. Kleinman RL, Senanayake P, Epidemiology of infertility-a report of IPPF Panel of Experts on Infertility 1978 22-24:08-11. [Google Scholar]
[4]. Adegbola O, Akindele MO, The pattern and challenges of infertility management in Lagos, NigeriaAfr Health Sci 2013 13(4):1126-29.10.4314/ahs.v13i4.3724940341 [Google Scholar] [CrossRef] [PubMed]
[5]. Adeyemi AS, Adekanle DA, Afolabi AF, Pattern of gynaecological consultations at Ladoke Akintola University of Technology Teaching HospitalNiger J Clin Pract 2009 12(1):47-50. [Google Scholar]
[6]. Audu BM, Massa AA, Bukur M, Clinical presentation of infertility in Gombe, North-Eastern NigeriaTrop J Obstet Gynaecol 2003 20(2):93-96.10.4314/tjog.v20i2.14408 [Google Scholar] [CrossRef]
[7]. Bankole A, Adewole IF, Hussain R, Awolude O, Singh S, Akinyemi JO, The incidence of Abortion in NigeriaInt Perspect Sex Reprod Health 2015 41(4):170-81.10.1363/intsexrephea.41.4.017026871725 [Google Scholar] [CrossRef] [PubMed]
[8]. Graham O, Cheng LC, Parsons JH, The ultrasound diagnosis of retained foetal bones in West African patients complaining of infertilityBJOG 2000 107(1):122-24.10.1111/j.1471-0528.2000.tb11588.x10645871 [Google Scholar] [CrossRef] [PubMed]
[9]. Lewis V, Khan-Dawood F, King M, Beckmann C, Dawood MY, Retention of intrauterine foetal bone increases menstrual prostaglandinsObstet Gynecol 1990 75:561-63. [Google Scholar]
[10]. Topçu HO, Şimşek BŞ, Taşdemir U, Güzel AI, Doğanay M, Retention of foetal bones 8 years following termination of pregnancyJ Exp Ther Oncol 2014 10(4):267-69. [Google Scholar]
[11]. Izhar R, Husain S, Tahir S, Husain S, Secondary infertility due to retained foetal bones diagnosed via saline sonographyJ Coll Physicians Surg Pak 2016 26(10):861-62. [Google Scholar]
[12]. Srofenyoh EK, Addison M, Dortey B, Kuffour PA, Intrauterine retained fetal bones as a cause of secondary infertilityGhana Med J 2006 40(3):105-09.10.4314/gmj.v40i3.5526217299576 [Google Scholar] [CrossRef] [PubMed]
[13]. Mahdavi A, Kazemian S, Koohestani E, Secondary infertility due to intrauterine foetal bone retention: A case report and review of literatureInt J Reprod Biomed 2019 17(8):591-94.10.18502/ijrm.v17i8.482531583377 [Google Scholar] [CrossRef] [PubMed]
[14]. Khan SN, Modi M, Hoyos LR, Imudia AN, Awonuga AO, Bone in the endometrium: A reviewInt J Fertil Steril 2016 10(2):154-61. [Google Scholar]