A substantial proportion of patients begin their dialysis with catheters and remain catheter dependent [1]. Tunneled Cuffed Catheters (TCCs) are the primary vascular access for patients who are unable to get an Arteriovenous Fistula (AVF). Sometimes, it is offered to patients with prolonged Acute Kidney Injury (AKI) or as a bridge to renal transplant [2]. Catheter Related Blood Stream Infection (CRBSI) is the major bane associated TCCs, but thrombosis is also significant cause of catheter loss (amounting up to 33% catheter losses) [3].
While early catheter dysfunction is mostly mechanical in nature, late flow disturbances are usually due to an intraluminal or tip thrombus or fibrin sheath formation. A line angiogram is required to differentiate between the two, but is unavailable at most centers [4]. It is convenient to use a thrombolytic agent before embarking upon more invasive and costly procedures. The 2006 Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines recommended trial of alteplase as fibrinolytic agent for late catheter dysfunction [5]. Other fibrinolytics that have been used for restoring line patency include urokinase, reteplase and tenecteplase. Urokinase was the most widely used and recommended drug but fell out of favour as manufacturing stopped in the US in 2004 [6]. It is still widely used in Europe [7]. Catheter lock and infusion protocols have been used with reasonable success [8-11]. Admitting a patient for thrombolytic administration, is often unacceptable to patients due to time and cost contraints. It means further time away from work and travel. It creates an undue burden on the hospital facilities too. The present study was a single center experience from a tertiary-care public sector teaching Institute in Western India of the estimation of the safety and efficacy of high dose urokinase lock on outpatient basis as rescue for blocked TCCs.
Materials and Methods
The present study was a prospective cohort study. All TCCs inserted between September 2017 and September 2018 (12 months) were prospectively followed till loss of catheter/patient or end of study (December 2018, 16 months). Informed written consent was obtained from all participants. Since the study didn’t involve any new intervention or experimental drug, it was exempted from ethical board review, as per the Institute protocol at the time. This study was planned to systematically assess the efficacy and safety of a prevalent practice. However, the Helsinki guidelines were followed and respected during the study.
Catheter site preference order was right internal jugular, left internal jugular, left femoral and right femoral veins. Partial or complete thrombosis of preferred veins was the standard indication for using less suitable sites. Catheter lock was routinely done with heparin (5000 U/mL). Prophylactic anticoagulation or thrombolytics were not used. All catheters with poor flow during dialysis were evaluated. Catheter dysfunction was defined as decrease in blood flow in either lumen from baseline, high pre-pump pressure (< -250 mm Hg) or failure to aspirate blood from either port. Two cut-offs of poor flow were used for intervention (250 mL/min and 200 mL/min) based on baseline flow.
All catheters without clear evidence of mechanical obstruction on a chest radiograph, with non-positional flow disturbance were presumed to be due to intraluminal or tip thrombus and were treated with urokinase lock. Patients with history of haemorrhagic cerebrovascular accident, uncontrolled hypertension (BP >180/110 mmHg), active internal bleeding, recent surgery (<2 weeks) and known allergy to urokinase were excluded. Relative exclusions were current anticoagulation with International Normalized Ratio (INR) >2.0, known bleeding diathesis. A prelock coagulation profile was checked in all cases using Prothrombin Time (PT) and activated Partial Thromboplastin Time (aPTT). An intraluminal lock with urokinase solution (50,000 Units in 0.5 mL with heparin 5000 U/mL) was used in each lumen. The dead volume of both the catheter lumina was used as fill volume and the solution was kept for 24 hours. Subsequently, the catheter was used for dialysis after withdrawing the lock solution. Repeat locks were used when required for same indications. If no flow was established after three locks, the catheter was removed and fresh access or renal replacement therapy option planned. No more than three locks was used in any patient.
Cause of catheter losses were recorded. CRBSI were defined as per North American Vascular Access Consortium definitions [12].
Statistical Analysis
Results were expressed as numbers, percentages, proportions and mean±SD as appropriate. Kaplan-Meier analysis and survival curves with log rank test were used to estimate the median catheter survival. Association between various factors and need for urokinase administration was evaluated using Mann-Whitney U and similar statistics as appropriate. Binary logistic regression were used to assess predictive value of various factors for urokinase salvage. A p-value <0.05 was considered statistically significant. Statistical analysis was performed with SPSS Statistics for Windows, version 20. (Armonk, NY: IBM Corp.)
Results
A total of 183 TCCs were inserted in 171 patients during the study enrollment. Seven catheters were lost to early complications. With 17 patients having incomplete data or being lost to follow-up, only 159 TCCs were included in the final evaluation. The baseline details of the patients are summed up in [Table/Fig-1].
Baseline characteristics of the study cohort.
| No. of catheters completing follow-up | 159 |
| Age {Mean(SD)} | 41.8 (16.9) years |
| Males | 88 (55.3%) |
| History of Deep Vein Thrombosis (provoked) | 53 (33.3%) |
| Antiplatelet drugs | 24 (15.1%) |
| Cause of renal failure |
| Diabetes | 60 (37.7%) |
| CKD of unknown aetiology | 47 (29.6%) |
| Obstructive uropathy | 21 (13.2%) |
| Postpartum AKI (Persistent AKI) | 10 (6.3%) |
| Posttransplant | 8 (5%) |
| Others | 13 (8.2%) |
| Site of TCC placement |
| Internal jugular vein, Right | 106 (66.7%) |
| Internal jugular vein, Left | 30 (18.9%) |
| Femoral vein, Left | 20 (12.6%) |
| Femoral vein, Right | 3 (1.8%) |
| Reason for TCC insertion |
| Suboptimal veins | 76 (47.8%) |
| Previous AVF Failure, Primary | 23 (14.5%) |
| Previous AVF Failure, Secondary | 13 (8.2%) |
| Prolonged AKI/Graft Failure | 22 (13.7%) |
| Severe limb oedema/thrombophlebitis | 12 (7.5%) |
| Awaiting AVF/Transplant | 13 (8.2%) |
| Follow-up | 5-437 days |
Of the 159 catheters, poor blood flow episodes were reported in 59 patients. Flow dyfunction without evidence of mechanical obstruction, needing urokinase salvage occurred in 57 (35.9%) amounting to 2.66 episodes per 1000 catheter-days. Two patients had catheter kink, which were managed by catheter replacement. Most common presentation was absent blood flow in one lumen [Table/Fig-2]. Blood flow threshold for urokinase administration in majority of cases was, when it fell below 200 ml/min. Urokinase lock was used in all catheters using the protocol described.
Patterns of catheter flow dysfunction and loss.
| Parameters |
|---|
| Mean time to flow dysfunction | 113.5±76.3 days (Range 13-323 days) |
| Mean time to catheter loss due to poor flow | 139.8±90.4 days (Range 16-384 days |
| Patterns of flow dysfunction | N=57 |
| No flow in one lumen | 28 |
| No flow in either lumen | 17 |
| Decreased flow in both lumen | 12 |
| Blood flow | 5 |
| <200 ml/min | 7 |
| Cause of catheter loss | N=120 (with overlap) |
| Death with working catheter | 35 (29.2%) |
| AV fistula available | 27 (22.5%) |
| Transplant | 9 (7.5%) |
| CRBSI | 30 (25%)*† |
| Inadequate flow | 22 (18.3%)* |
| Recovery from RRT need | 6 (5%) |
| Others | 6 (5%) |
RRT: Renal replacement therapy; CRBSI: Catheter related blood stream infection
*There was overlap of CRBSI and inadequate flow with other catheter outcome; †CRBSI was defined as per north american vascular access consortium definitions [12]
Mean time to first episode of catheter dysfunction was 113.5±76.3 days but range was very variable (8-384 days). Patency was improved in 48 (84.2%) cases (defined as at least 50 ml/min improvement and blood flow above 200 mL/min) while completely restored in 41 (71.9%) cases (blood flow >250mL/min or previously known values) after single use of urokinase lock. Repeat locks were required in 17 (29.8%) patients, 2 locks in 11 (19.2%) patients and 3 locks in 6 (10.5%) patients.
At the end of the follow-up period, 39 (24.5%) catheters out of 159 recruited were functioning, while 120 were lost. Causes of cathter loss has been shown in [Table/Fig-2]. Of all cathter losses, 22 (18.33%) catheters were lost due to flow related issues. Mean time to all-cause catheter loss and catheter loss due to flow dysfunction were 118±74.3 days (range 5-399) and 145.8±78.5 days (Range 16-323 days), respectively. The difference was not statistically significant (p=0.11). Sixteen catheters (10%) were lost to inadequate flow in isolation, while 6 catheters had overlap with other catheter outcomes (1 death, 3 CRBSI, 1 AVF creation and 1 recovery from dialysis dependency).
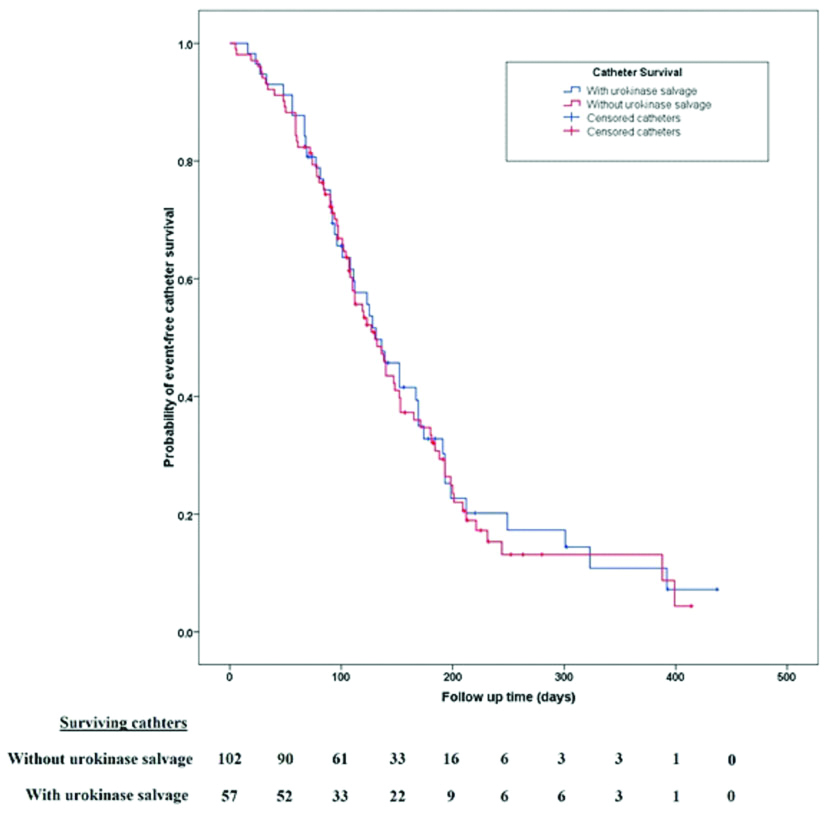
Overall survival of catheters needing urokinase salvage was not inferior to those not needing such rescue (Log rank=0.077, p=0.78; [Table/Fig-3]). Urokinase therapy was needed more frequently in left sided or femoral catheters, rather than right internal jugular catheters, but the difference failed to reach statistical significance (Urokinase salvage needed in 32 of 106 right internal jugular TCCs vs. 25 of 53 at all other sites, p=0.053). Binary logistic regression was carried out to evaluate the effect of various factors (age, gender, site of catheter insertion, cause of opting a TCC, dialysis in-house vs. peripheral units and Split tip vs. staggered tip) on catheter thrombosis. The only significant factor was TCC insertion for prolonged AKI or graft failure (p=0.028). None of the other factors were predictive of flow-related catheter dysfunction [Table/Fig-4].
Survival of catheters with thrombolytic lock vs. those not needing such rescue.
Predictive value of baseline factors towards need for urokinase rescue.
| Variables | Comparison | Test statistic | Relevance* |
|---|
| Age | Age distribution | 0.063 | NS |
| Gender | Male vs. female | 0.762 | NS |
| Catheter type | Split tip vs. staggered tip | 0.951 | NS |
| Center type | Peripheral units vs. In-house dialysis | 0.790 | NS |
| Catheter site | Right internal jugular vs. others | 0.067 | NS |
| Reason for TCC | Non recovering AKI | 0.028 | Significant |
| Primary/Secondary AVF failure | 0.940 | NS |
| Pretransplant | 0.062 | NS |
| Poor veins/Thrombophlebitis | 0.472 | NS |
AKI: Acute kidney injury; AVF: Arteriovenous fistula; TCC: Tunneled cuffed catheter; *p-value of <0.05 was considered as statistically significant; NS- Non Significant
There were no background alteration of coagulation times (PT or APTT) in any patient. None of the patients in the cohort experienced any major or minor bleeding or allergic reaction to urokinase. Second and third administration of urokinase was also uneventful in all cases.
Discussion
Although TCCs have partially succeeded in overcoming certain drawbacks of non-tunneled catheters, poor overall survival have been reported unanimously [13,14]. The most important step before and after placement of a catheter would be to establish a permanent access. Those who are eligible for transplant must be expeditiously evaluated. Those who are still eligible for an AVF should be managed accordingly. Meticulous catheter care during and after dialysis sessions can’t be overemphasised. In this study, 53 (33.3%) patients needed catheters to be inserted at sites other than the right internal jugular vein. All such patients had partial or complete thrombosis of the right internal jugular vein. Femoral sites were used only when neither of the internal jugulars were available for catheter placement. Thus access planning needs to begin far earlier.
Thrombosis related TCC dysfunction has been variedly defined. Estimated incidence also varies considerably. A catheter is labeled dysfunctional when the peak flow during dialysis falls below a threshold (250 mL/min). High arterial pressures (<−250 mm Hg) and high venous pressures (>250 mm Hg) are also indicative of catheter dysfunction [5,15]. Catheter thrombosis has been reported in 0.5-3 episodes per 1000 catheter days and may lead to catheter loss in up to 17-33% [3,16]. Thrombosis rate (2.66 per 1000 catheter days) in the present study was comparable to previous reports. Catheter loss due to thrombosis (13.8%) was lower, possibly because overall survival of catheters was low and infection rates were high (3.74 episodes per 1000 cathter days) leading to rapid attrition of catheters.
In India, where cost is a major hindrance, urokinase is relatively inexpensive and easily available than other fibrinolytic agent, like Alteplase which is used as infusion of 2-2.5 mg is available as 20mg and 50mg vials and needs to be stored as frozen aliquots to make it cost effective. There is risk of wastage or contamination (if stored) associated with its use. Urokianse is available in more dose appropriate packaging [17]. Although the lyophilised preparation available undergoes a meticulous process of testing for transmissible infections, there is a theoretical risk of transmission of viral infections.
The success of urokinase in catheter clearance ranges from 70-90% [4]. Haire WD et al., reported a 59% catheter patency after urokinase compared to 89% with alteplase. The incubation period was two hours and 10000U of urokinase was used [18]. Van Hulle F et al., group reported success rate of 84% for blood flow and 90% for pump pressures after the first lock [9]. Other studies have reported 40-100% restoration of catheter patency [8,19]. With incremental doses, using locking and infusion protocols, a study showed that higher doses were more effective in restoring catheter flow [20]. The observations of the present study (patency rate of 84.2%) were in agreement with previously published data.
In this cohort, TCC insertion for prolonged AKI was the only factor predictive of requirement of urokinase therapy. This may be attributed to the more frequent use of heparin free or tight heparin schedules in such patients. Non-right sided catheters (which are typically needed when right internal jugular vein is partially or completely thrombosed, showing a possible tendency towards thrombosis) didn’t show statistically significant association. Also, association between primary or secondary AVF failure (possible clinical predictors of underlying hypercoagulable states) and need for urokinase salvage was not seen in this study (p=0.94).
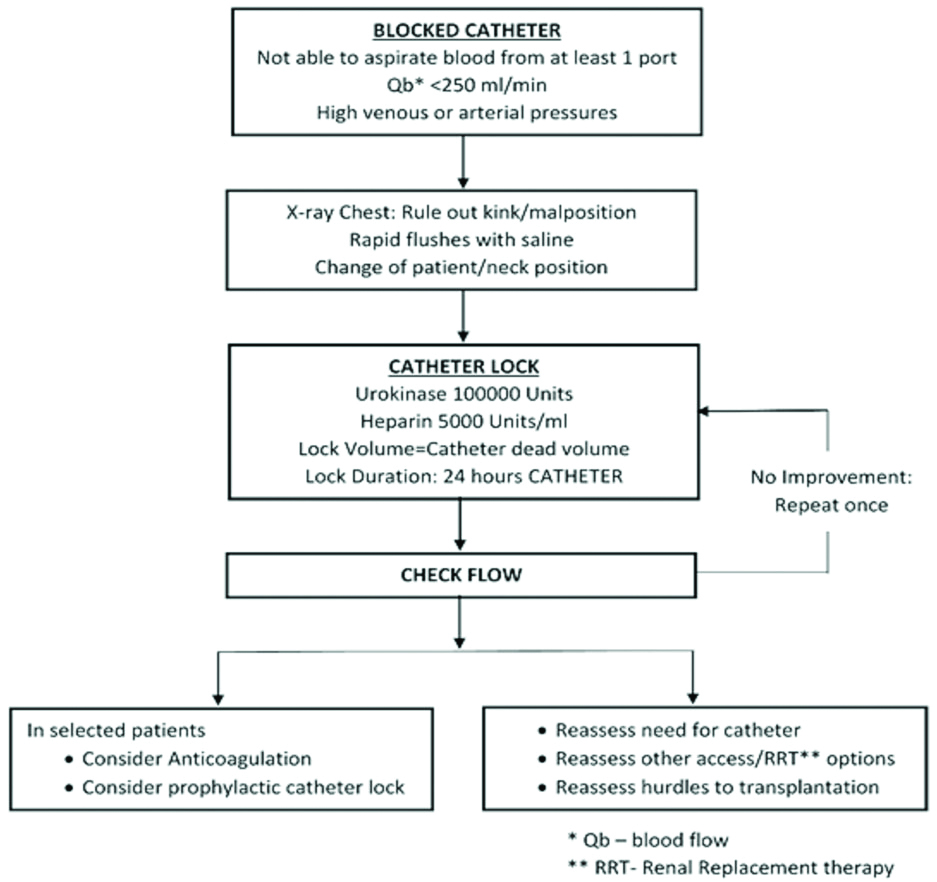
Urokinase administration is safe. Allergic reaction and bleeding is distinctly rare. All studies reported zero bleeding and allergic reactions with outpatient administration of urokinase lock or infusion [4,7,21]. No episodes of any adverse reactions with urokinase lock were observed. Prothrombin Time (PT) and activated Partial Thromboplastin Time (aPTT) were routinely checked before administration of urokinase. Background derangement of coagulation is known to occur due to leakage of heparin locks that is used as standard of care [22]. However, no instance of significant coagulopathy (aPTT >1.5 times baseline or >50s) in the present cohort. When interventional radiology services are not available, a step wise approach to a blocked catheter is suggested as shown in [Table/Fig-5] [15,23]. Paramedical staff maybe trained to actively screen patients eligible for thrombolytic therapy using a checklist as provided in [Table/Fig-6] [24,25].
Stepwise approach to a TCC with flow dysfunction.
Checklist before planning urokinase lock [24,25].
| Absolute contraindications |
| History of haemorrhagic cerebrovascular accident |
| Uncontrolled hypertension (BP>180/110 mmHg) |
| Active internal bleeding |
| Recent surgery (<2 weeks) |
| Known allergy to urokinase |
| Relative contraindications |
| Current anticoagulation with INR >2.0 |
| Known bleeding diathesis |
Limitation(s)
The study presents the results of a relatively small cohort. As patients were dialysed in different centers attached to the Institute and in the hospital of Institute (hub-and-spoke model of healthcare delivery), the referral and intervention (urokinase lock) was not uniform. This may have confounded the efficacy outcomes. Also, the cause of catheter dysfunction was not clearly delineated by a line-angiogram before urokinase administration.
Conclusion(S)
The study found urokinase lock, used on outpatient basis safe and efficacious. The overall survival of catheters needing thrombolytic lock was non-inferior to catheters not needing such salvage. Background alteration of coagulation profile from standard heparin locking of TCCs was not found. Thus, when intervention radiology services are not available, urokinase lock can be safely used by dialysis units without any undue risk to the patient. In view of the excellent safety profile of the intervention, direct in-hospital medical supervision is not needed.
RRT: Renal replacement therapy; CRBSI: Catheter related blood stream infection
*There was overlap of CRBSI and inadequate flow with other catheter outcome; †CRBSI was defined as per north american vascular access consortium definitions [12]
AKI: Acute kidney injury; AVF: Arteriovenous fistula; TCC: Tunneled cuffed catheter; *p-value of <0.05 was considered as statistically significant; NS- Non Significant