The Percutaneous Tracheostomy (PCT) is an elective procedure, which can be performed by an anesthesiologist, at the bed side. It has many benefits over surgical tracheostomy [1]. This is very useful procedure and is performed in critically ill patients, under prolonged mechanical ventilation [2]. Most of these patients are haemodynamically unstable, with inotropes and vasopressors, so keeping the duration of the procedure very minimal, holds priority.
This is essential because, these critically ill patients might not tolerate the insertion of FOB and thereby, resulting in hypoxia. In sepsis patients with Adult Respiratory Distress Syndrome (ARDS) there is a possibility of alveolar recruitment upon FOB introduction and during the dilatation process, leading to dangerous hypoxia. Moreover, the positioning of neck [3] made by placing the sandbag under the shoulder, for a prolonged duration, can compromise the preload, resulting in hypotension. Nevertheless, the risk versus benefit shifts in favour of tracheostomy, which can markedly improve the clinical outcome. The time taken for the PCT must be kept minimum, because the hypoxic complication increases with the duration of the procedure in sick patients [4].
Ciaglia’s technique, employs percutaneous seldinger method, using the tapered horn dilator for dilating the tracheal aperture over the guidewire for tracheostomy tube insertion. Whereas in Griggs technique a specialised GWDF, is used for dilatation.
This study was designed to overcome the difficulty which was encountered during tapered horn dilatation in the Ciaglia technique alone in certain patients. In such patients to achieve proper dilatation, this step has to be repeated many times when difficulty was encountered, which is not acceptable in critically ill patients. This paved the way to adopt this combined technique. When combining these two techniques by first dilatating with GWDF creates a dilation aperture through which the tapered horn dilator can be passed with ease and also creates a circular stoma for smooth insertion of tracheostomy tube. The complication rates were minimum in a comparative study between Ciaglia technique and Combined Ciaglia with Griggs technique [5].
The aim of the present study was to evaluate the ease of insertion, timing of the procedure and complications when combining Griggs and Ciaglia technique for performing PCT under fiberoptic guidance.
Materials and Methods
This was a prospective observational study, conducted on 250 critically ill surgical gastroenterology patients (on mechanical ventilation), that required tracheostomy consecutively. The study was conducted between the period of December 2017 to December 2019, which was ethically approved by the Institutional Ethical Committee (S. no 9001). Informed written consent was obtained from next of the kin of the patients.
Inclusion criteria: Patients on prolonged ventilatory support, airway protection, weaning from mechanical ventilation.
Exclusion criteria: Patients with difficult airway, severe coagulopathy.
The study was conducted in the Intensive Care Unit (ICU), by a team of eight anesthesiologists with same level of experience in PCT, with no observer bias.
Each anesthesiologist had a minimum experience of performing 50 PCT’s each in human patients and also experience of performing 10 PCT’s in cadavers and the team of eight anesthesiologists had conducted PCT workshops for anaesthesia and critical care postgraduates in state conferences.
Among the team of eight anesthesiologists, one anesthesiologist performed the procedure, one anesthesiologist took the role of FOB insertion and airway maintenance, two anesthesiologists were involved in the whole critical care management of the patient, two anesthesiologists were recording study parameters and two anesthesiologists were involved in the post-operative follow-up in turns.
Patient data: Patient data like age, sex, Body Mass Index (BMI) (the weight of the patient recorded at the time of admission to the hospital was taken for calculation of the BMI), acute physiology and chronic health score, number of days on orotracheal intubation, indication for tracheostomy were recorded [6].
Routine laboratory parameters like haemoglobin, complete blood counts, renal function tests, liver function tests and coagulation profile were recorded. Chest X-ray was taken daily.
Preprocedural preparation: All patients were sedated with Propofol (3 mg/kg), Fentanyl 3 mg/kg and Midazolam (2 mg). Titrated atracurium was used to achieve absence of spontaneous respiration and physical movement. All patients received inspired oxygen concentration (Fio2) of 100% during the procedure.
Tracheostomy tubes of 8 mm or 8.5 mm and 7 mm or 7.5 mm (inner diameter), were kept ready for male and female patients, respectively. Cuff patency was checked, and the lubricated cuff was deflated and smoothened towards the flange. The PCT set was sequentially arranged in the order of their insertion, as following 1: 2,00,000 Adrenaline, 14G Needle with Plastic cannula assembly, guidewire, Scalpel, 14G Plastic dilator, Griggs forceps, Guiding catheter, Tapered horn dilator, Introducer, Tracheostomy, Lignocaine gel.
Procedure: A patient was positioned by placing a pillow under the shoulders with the neck extended and relevant landmarks namely cricoid cartilage, thyroid cartilage, tracheal rings and suprasternal notch, were marked. Scout scan, which is the screening ultrasound was performed to look for the presence of enlarged thyroid, aberrant blood vessels like anterior jugular veins and inferior thyroid veins.
The Endotracheal Tube (ETT) was withdrawn, by an assisting anaesthesiologist under bronchoscopy visual control, so that half of the cuff was visible above the vocal cords. The anterior neck was prepared with povidone iodine and draped with sterile sheets. The site of insertion was one finger breadth above the suprasternal notch. A 3-5 mL of 1% lidocaine with adrenaline (1:200 000) was infiltrated subcutaneously to minimise the bleeding.
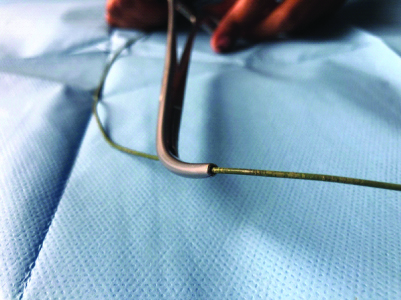
The trachea was punctured with a 14-gauge cannula on needle in a posterior-caudal under bronchoscopy, visualisation needle was removed, after successful placement of the tracheal cannula, at 12’O clock position. A ‘J’ tip guidewire was passed through the cannula into the lumen of trachea and leaving the guidewire behind, the cannula was withdrawn. Next the 14 G lubricated plastic dilator was advanced over the guidewire and gently screwed and removed. So as to create a channel for introducing the Griggs forceps [Table/Fig-1].
Griggs forceps- guidewire dilating forceps.
The guidewire dilating forceps (Griggs forceps) with its handle closed, was advanced over the guidewire until resistance was felt. The forceps handle was now opened to dilate the anterior tracheal wall, in the midline around the guidewire. The forceps handle must be opened in a controlled manner without excessive force. After formation of stoma, the GWDF was removed in the open position, leaving the guidewire in-situ. Next, the lubricated tapered horn dilator was preloaded over the long guiding catheter upto the black safety ridge. The whole unit of the tapered horn dilator [Table/Fig-2] with the guiding catheter was inserted over the guidewire using a firm and steady screwing movement, thereby creating a circular stoma. The tracheostomy tube over a well-lubricated introducer was then inserted through the tracheal stoma. The assembly of introducer, the guidewire, and the guiding catheter assembly were then removed as a whole unit leaving the tracheostomy tube in situ.
Tapered horn dilators preloaded over the guiding catheter.

After placement of the tracheostomy tube, tracheal suction was performed, the tracheal cuff was inflated with air and ventilation of the patient’s lungs was resumed through the tracheostomy tube. Fiberoptic bronchoscope was removed, followed by the ETT. FOB was then introduced inside the tracheostomy tube to make sure that there was adequate distance between the tip of the tracheostomy tube and the carina. Air entry into the lungs was confirmed by chest auscultation and EtCo2 trace and a chest radiograph was ordered.
Parameters Noted
1. Duration and ease of insertion
The time taken to perform the procedure (needle insertion to successful placement of tracheostomy tube) was noted. During the process the following observations were made-difficulty in dilating the tracheal stoma, number of attempts at stoma dilation, insertion of tracheostomy tube. The stoma was labelled under-dilation if it required more than one attempt and the cannulation was then considered difficult.
2. Complications during procedure
1. Bleeding from the procedure:
50% soaked 10×10 inch gauze holds 5 mL blood [6], accordingly, bleeding was classified into four grades, based on the quantity of blood loss in the tracheal aspirate: Grade I (5 mL), Grade II (6-10 mL), Grade III (11-50 mL or 10 mL), Grade IV (50 mL).
2. Hypoxia (Spo2-95%),
3. Hypercarbia (5 mm increase in ETco2 from the baseline),
4. Hypotension (20% decrease in systolic pressure),
5. Hypertension (20% increase in systolic pressure),
6. Technical difficulties were recorded.
The stoma dilation was classified as adequate dilation (stoma restricted to the anterior wall of the trachea), over-dilation (stoma margins extending to more than half of the anterior circumference), or near total transection (when more than two-thirds of the tracheal circumference was dilated) [7].
3. Post-operative complications
Complications like bleeding, pneumothorax, pneumomediastinum, infection at the stoma site, post-operative pneumonia, accidental tracheal decannulation were observed. Any occurrence of difficulty in reintroduction of tracheostomy tube in the event of tracheostomy tube block by blood or mucus was observed in the post-operative period.
Tracheostomy tube was decannulated once the patient met the decannulation criteria-surgical condition stabilised, fit to be shifted to ward, airway reflexes intact, speaking valve trial passed.
Using an adhesive plaster, strapping was done at the decannulation site. After strapping, immediately the patients were able to vocalise normally. In less than a week, the stoma got healed and closed by itself without the need for suturing. The adhesive plaster was used for strapping and was removed after 48 hours.
The patients were followed-up after tracheostomy tube removal in the ward and also after discharge. The following parameters were observed like nature of the tracheostomy scar, change in voice and difficulty in breathing.
Statistical Analysis
Analysis was done using Statistical software SPSS version 16.0. All continuous variables were expressed as mean and standard deviation. All categorical variables were expressed as percentages and proportions.
Results
Basic Demographic Details of the Study
In the study population majority of them were males (72%). They belonged predominantly to 35 to 55 years age group (55.6%). Based on BMI 4% were obese, and 45.6% were overweight [Table/Fig-3].
| Parameters | Values N(%) |
|---|
| Sex | Males | 180 (72%) |
| Females | 70 (28%) |
| Age category (Years) | 25-35 | 22 (8.8%) |
| 35-55 | 139 (55.6%) |
| 55-65 | 57 (22.8%) |
| 65-75 | 32 (12.8%) |
| Body mass index (kg/m2) | 18-23 | 114 (45.6%) |
| 23-25 | 48 (19.2%) |
| 25-30 | 78 (31.2%) |
| 30-40 | 10 (4%) |
Duration
The mean procedure time was 2 minutes and 24 seconds. Out of the 250 patients in whom PCT was done, 230 procedures were done in less than two minutes. For 10 patients mean duration of the procedure was approximately six minutes, who were moderately obese with BMI 34 had short neck. Two patients had ETT expulsion, during the procedure, so the ETT was guided and positioned over the FOB, which made the procedure last approximately five minutes, these two patients were also included in the study.
In eight patients who suffered ARDS secondary to sepsis, intraprocedural desaturation with an oxygen saturation between 80-86% occurred. In these patients it took approximately 12 minutes, to finish PCT because the procedure has to be stopped till safer oxygenation was achieved. Of the 20 patients (obesity-10, expelled ETT- 2 and ARDS with desaturation- 8) had delayed duration of procedure of mean 7 minutes and 45 seconds.
Complications During Procedure
During the study, incidence of hypercarbia, hypertension was nil. Hypotension was present in 12 cases, two were on vasopressors and were managed with increasing the vasopressor infusion rates. The most common grade of blood loss was Grade I. Adequate stoma dilatation were observed which made the tracheostomy tube insertion easy in all patients.
Post-operative Complications
Incidence of post-operative bleeding, pneumothorax or pneumomediastinum was nil. Post-operatively, there was no difficulty in changing the tracheostomy tube. There was no incidence of wound infection in the tracheostomy site.
Post-operative pneumonia occurred in nine patients, between 4 to 6 weeks but this observation could be due to variable perioperative factors like pre-operative smokers, COPD, ventilator associated pneumonia, etc.
Patients were vocalised without any hoarseness. The voice quality was similar to the pre-operative state. No breathing difficulty was observed. The tracheostomy scar was cosmetically acceptable.
Discussion
The important factor which paved the way for this study design was the need to overcome the difficulty which was encountered during tapered horn dilatation in the Ciaglia technique, when employed alone, for performing PCT. The time delay which occurred due to repeated manipulations for dilating the trachea can be detrimental in critically ill patients because they are prone to haemodynamic instability. When combining Griggs and Ciaglia techniques, first dilatation with GWDF creates a dilation aperture through which the tapered horn dilator can be passed with ease and also creates a circular stoma for smooth insertion of tracheostomy tube.
Moreover, if only Griggs technique is employed, a circular stoma is less likely, because only a transverse dilatation is facilitated by the GWDF. This is because, Griggs forceps if dilated in a vertical fashion, might lead on to tracheal ring fracture. A circular stoma enhances the smoothness of tracheostomy tube insertion, which can be achieved by the Ciaglia technique using Blue rhino tapered dilator [8,9]. This combined technique has decreased the duration of the procedure to less than two minutes. In all the cases blue rhino and the tracheostomy tube insertion were inserted in the 1st attempt.
In the randomised control study conducted by Ambesh SP et al., comparing Ciaglia and Griggs technique in 60 patients the mean duration of the procedure was 7.7 minutes in Ciaglia’s group and 6.5 minutes in Griggs technique. In that study, two patients of the Ciaglia group, the operator had difficulty in passing the tracheostomy tube after the first attempt and required redilation. On a few occasions, the operator had lost his grip over the tapered horn dilator during the stoma dilation. In the Griggs group, it was difficult to judge the formation of adequate size of tracheal stoma. In 21 patients, the tracheostomy tube was inserted on the first attempt at tracheal dilation whereas nine patients required a second attempt [10]. Direct visualisation with bronchoscopy enhances the margin of safety by preventing serious complications such as false passage, pneumothorax, posterior tracheal wall tears and subcutaneous emphysema [11].
In the present study of 250 patients, 20 patients had delayed duration of procedure with a mean of 7 minutes and 45 seconds; 230 patients had a mean duration of procedure of 2 minutes and 24 seconds; the complications observed were negligible in all patients. So, this procedure can be adopted safely in the anesthesiologist’s critical care practice.
Limitation(s)
Since study groups, of PCT employing sole Griggs and Ciaglia’s technique alone were not compared, the statistical significance could not be derived in this study. Being an observational study, with the experience of this combined technique in 250 patients with negligible complications, this technique maybe advocated.
Conclusion(s)
Based on the study experience it can be suggested that combining Griggs and Ciaglia’s technique to perform PCT reduces the time of the procedure, it is safer and it enhances the ease of insertion of the tracheostomy tube. Proper patient selection and attention to the technical details are essential elements in the successful placement of tracheostomy tube.