A widely studied method of objective assessment of cataract is Scheimpflug imaging system which is based on Scheimpflug principle, introduced by Theodor Scheimpflug [4-7]. The first Scheimpflug imaging system used for investigation of the crystalline lens in-vivo was developed by Brown N [8]. It uses a camera which rotates and captures images in different meridians and creates three-dimensional images of crystalline lens [9]. The latest development among ophthalmic camera systems based on Scheimpflug’s principle is the Pentacam HR (Oculus, Wetzlar, Germany). Pentacam HR acquires a total of 50 images in approximately 2 seconds by a rotating Scheimpflug camera measurement and displays objective image of anterior chamber structure including lens density evaluation [10]. The Scheimpflug camera is a digital Charge-Coupled Device (CCD) camera along with synchronous pixel sampling feature. A blue Light Emitting Diode (LED) with a wavelength of 475nm, devoid of the UV fraction forms the light source. Out of the two cameras in the system, one camera located in the centre, detects the size and orientation of the pupil, and controls fixation while the second camera mounted on the rotating wheel, captures images from the anterior segment of eye. This arrangement gives a complete picture from the anterior surface of the cornea to the posterior surface of the lens [11]. To avoid shadows from nose, the camera takes slit images from 0 to 180 degrees and these images combine to form a 360 degree image of the anterior segment of eye.
Scheimpflug images allow for an automatic and objective quantification of the lens density. For the measurement of lens density, the programme quantifies lens density on a scale 0-100 (0=no cloudiness and 100=completely opaque lens) using the individual image. Peak values at one point of the nucleus of the individual images are measured along with mean and maximum density of nucleus. Standard Deviation (SD) is calculated automatically by the lens densitometry programme for a specific area drawn on the Scheimpflug image. Pentacam Nuclear Staging (PNS) is a built in lens densitometry software and it provides average and maximal lens density with a cataract grading score from grade 0 to 5 [12]. Both repeatability and validity of lens densitometry derived from Pentacam were assessed by several studies and have been shown to be high [13,14].
For grading the lens opacity, Scheimpflug photography, which depends on morphological lens changes, is known to have greater precision than LOCS III [15]. In addition, it allows to identify even the minute changes in cataract progression than LOCS III [16]. This Scheimpflug technology also provides an opportunity to analyse the relationship between the densitometric measurements on Pentacam and phacoemulsification parameters [17]. One limitation of Scheimpflug imaging system is that the posterior structure of the lens is concealed by the refractive and obscuring effect of the anterior opacified structure of the lens [18].
In present era, the knowledge about lens density could help to enhance the ability to estimate the ultrasound power needed during the phacoemulsification. In other words, quantitative measurement of cataract is also vital in predicting the dynamics during phacoemulsification surgery. Pre-operative assessment of cataract has the potential to better organise and customise operative plan on an individual basis. The optimisation in phacoemulsification energy dissipated during cataract surgery could potentially lead to better visual outcomes and lower trauma to the eye especially corneal endothelium. Lower levels of ultrasound power may help in reducing endothelial cell damage and thereby, results in clearer post-operative cornea. Therefore, it is reasonable to plan the operation with the lowest level of ultrasound energy needed to extract cataract with certain density profile [19].
The purpose of current study, therefore, was to correlate Scheimpflug imaging system parameters (like Nuclear Lens Density (NLD), Average Lens Density (ALD) and PNS score) with phacodynamics (phacoemulsification energy and phacoemulsification time) in assessment of age-related cataract and subsequently the ease of cataract surgery and anticipated complications.
Materials and Methods
This prospective interventional study was performed in Department of Ophthalmology, Government Medical College, Amritsar, India, between February 2016 and July 2017. A total of 100 eyes of 100 patients with age-related cataract were enrolled in the study after random selection.
Ethics approval (letter no- BFUHS/2K16p-TH/12527) was obtained from Hospital Institutional Review Board and study was conducted in adherence with Declaration of Helsinki. Written informed consent was obtained from all patients. Patient had the right to opt out of study at any time during the course of study without having to give reasons for doing so. Patients above 40 years with age-related cataract were included. No patients had history of active periocular and adnexal infection, pre-existing corneal opacity, previous intra-ocular surgery, ocular trauma or disorders other than cataract causing low vision (glaucoma, uveitis, Fuch’s endothelial dystrophy, retinal detachment or uncontrolled diabetes mellitus).
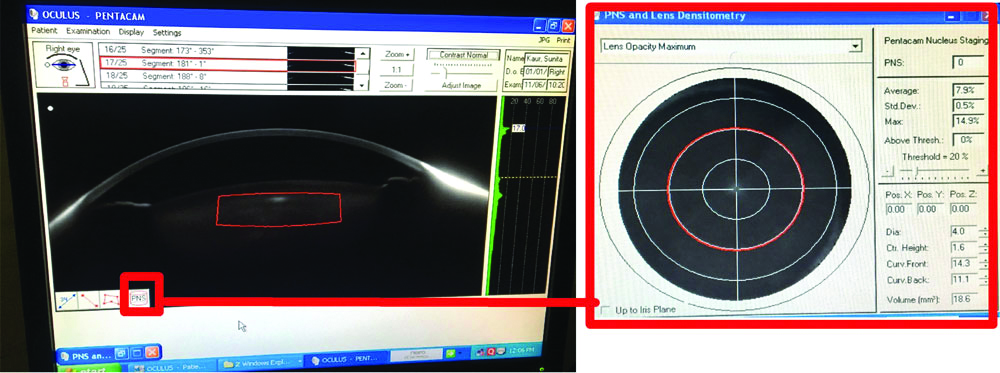
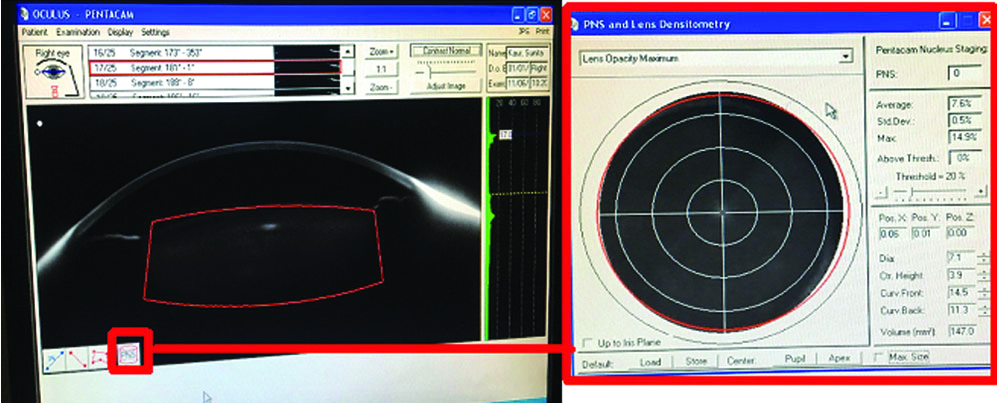
All patients underwent comprehensive ocular examination including Uncorrected Visual Acuity (UCVA) and Best Corrected Visual Acuity (BCVA) measurement on Snellen’s chart, slit-lamp examination (TOPCON SL-D7, Tokyo, Japan), Goldmann applanation tonometry, fundoscopy, keratometry (URK-700, Daejeon, Korea), ultrasonic biometry (Appascan AME-01A, Chennai, India). After detailed ocular examination of the presenting eye, evaluation of cataract was done using Pentacam HR after pupillary dilatation using combination of topical 0.8% tropicamide and 5% phenylephrine eye drop. All Scheimpflug images were taken in the same room under dark conditions to avoid undesired reflexes in the images. The patient was seated comfortably with his/her chin on chin rest and forehead against the forehead strap and was asked to fixate straight ahead on a fixation target for the duration of the scan (2 seconds). Pentacam’s automatic release mode was used to reduce operator-dependent variability. Scheimpflug option on display was selected. Three different densitometric analyses modes were available in Scheimpflug imaging system namely linear mode, Region of Interest (ROI) mode, and automatic 3D mode by PNS software. For the 3D mode system, PNS automatically generates a cylindrical template for the density measurement. There were two templates used in the study for 3D mode. One template of 4 mm diameter was selected and placed in the centre of nucleus. It was called as PNS measured nuclear lens density (hereby called as NLD) [Table/Fig-1]. Other template used in the study measured the average lens density and was called as ALD [Table/Fig-2]. The minimum and the maximum value of Nuclear and ALD ranged from 0 to 100, and the PNS grading score ranged from 0 to 5. A threshold value of 20% was considered during image acquisition in 3D mode. All Pentacam measurements were performed by a single observer (SJ) thereby minimising inter-observer variation.
Nuclear lens density on Scheimpflug imaging and PNS.
Average lens density on Scheimpflug imaging and PNS.
All patients underwent phacoemulsification with posterior chamber Intraocular Lens (IOL) implantation under peribulbar anaesthesia by a single surgeon. A 2.8 mm clear corneal incision was made in temporal quadrant. Hydroxypropyl methyl cellulose 2% was used to reform and stabilise anterior chamber besides protecting corneal endothelium. Continuous curvilinear capsulorrhexis of approximately 5.0-5.5 mm in diameter was created, and cortical cleaving hydrodissection was then performed. Nucleus was emulsified using stop-and-chop or phaco-chop technique depending on type of cataract. After irrigation and aspiration of cortex, a single piece foldable (acrylic) IOL was implanted in capsular bag with the help of injector. Adequate hydration of main tunnel and sideport incision was done. At conclusion of surgery, phaco power and time required for phaco (phaco time) were noted.
Post-operatively, combination of topical Prednisolone acetate 1% (6 times a day) and Moxifloxacin 0.5% eye drops (4 times a day), and Nepafenac 0.1% (3 times a day) were administered. Steroid drops were gradually tapered every week over six weeks and finally discontinued. After surgery, patients were followed on day 1, 7, 14, 28 day, 8 weeks and 12 weeks for visual acuity, slit lamp examination and Intraocular Pressure (IOP) measurement using non-contact tonometer in the initial two weeks and by applanation tonometry later. Refraction was done at day 28, 8 and 12 weeks.
Statistical Analysis
The data from present study was systematically collected, compiled and statistically analysed to draw relevant conclusions. Statistical analysis was performed using SPSS Version 17 (SPSS, Chicago, Illinois, USA). The relationship between Pentacam parameters with phacoemulsification power and time was evaluated by Pearson correlation analysis (r) and regression analysis. Statistical analysis of post-operative complications (corneal oedema and IOP) with Pentacam and phacoemulsification parameters was done using student-t test. The value was determined and evaluated for level of significance. A p-value of <0.05 was considered statistically significant and p-value of >0.05 was considered non-significant. Power analysis of the study was done to calculate the power of study by taking α error at 0.05. Effect size was calculated and it was seen that in this study the power was 100%.
Results
In present study, mean age of patients undergoing surgery was 58.21±9.24 years (range- 42 to 80 years). There were 55 male and 45 females. The mean PNS score obtained using Pentacam was 2.38±1.43 (range, 0-5), mean NLD was 17.60±6.81 (range, 8.70-48.1) and mean ALD 13.37±5.25 (range, 7.8-41.8). In this study, mean phacoemulsification power used was 50.25±7.31 (range, 40-70) and mean time was 14.1±6.60 seconds (range, 4-40 seconds). Out of 100 patients, post-operative corneal oedema was present in 20 (20%) patients and IOP was raised in 4 (4%) patients.
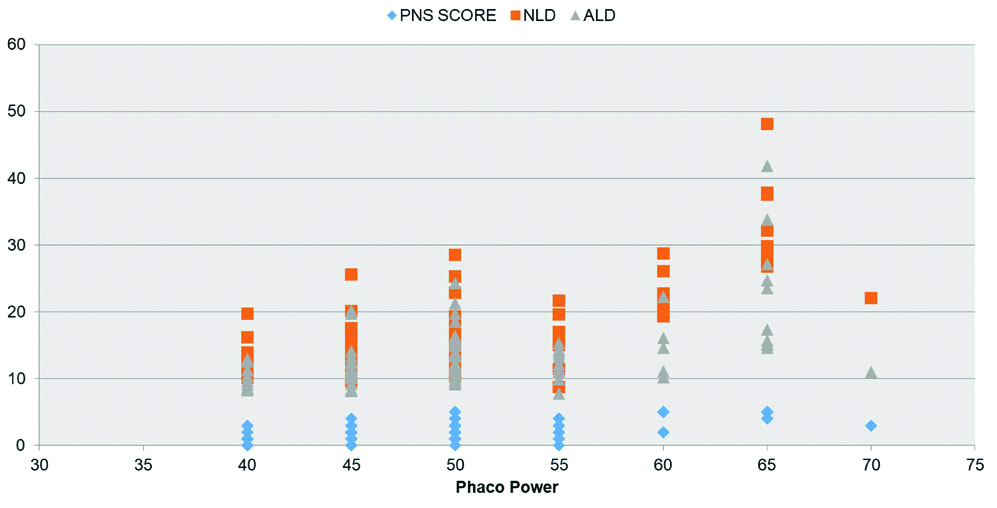
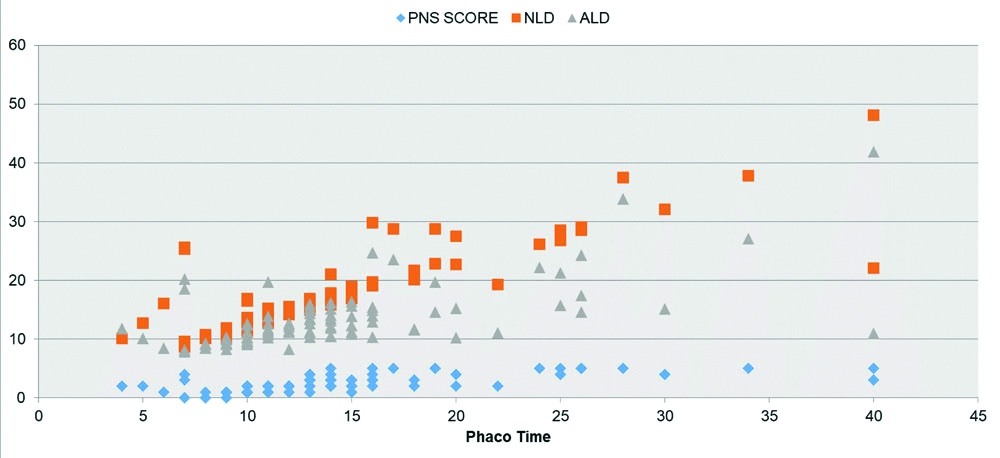
In the study, NLD, ALD and PNS score showed a strong positive linear correlation with phacoemulsification power (r=0.712; p<0.001, r=0.530; p<0.001, r=0.624; p<0.001, respectively) [Table/Fig-3] and time (r=0.842; p<0.00, r=0.653; p<0.001, r=0.679; p<0.001 respectively) [Table/Fig-4]. Regression equation for phaco power is given as-Power=38.042 + (PNS x 0.784) + (NLD × 0.921) - (ALD × 0.442) (Overall r=0.733 and r2 value is 0.523) and for phaco time is given as-Time=0.254-(PNS × 0.047) + (NLD × 1.036) - (ALD × 0.320) (Overall, r=0.852 and r2 value is 0.718). Adjusted r2 value is given as 0.523 and 0.718 which shows that there’s a significant correlation among Scheimpflug parameters and phaco parameters.
Correlation between Scheimpflug parameters (NLD, ALD, PNS score) and Phacoemulsification power.
Correlation between Scheimpflug parameters (NLD, ALD, PNS score) and Phacoemulsification time.
Post-operative corneal oedema had significant correlation with PNS score, NLD, phacoemulsification power and time but did not show significant correlation with ALD [Table/Fig-5]. Post-operative increased IOP did not show significant correlation with Pentacam and phacoemulsification parameters [Table/Fig-6]. No other post--operative complications such as shallow anterior chamber, iris prolapse, decentered IOL, IOL induced uveitis, cystoid macular oedema and endophthalmitis occurred during the period of consideration in present study.
Comparison of Scheimpflug parameters (PNS score, NLD, ALD) and phacoemulsification parameters (power and time) with post-operative corneal oedema. Group A: Corneal oedema absent, Group B: Corneal oedema present.
| Parameters | Group | No. of patients | Mean±SD | t-value | p-value |
|---|
| PNS score | A | 80 | 2.16±1.32 | -3.169 | 0.002 |
| B | 20 | 3.25±1.55 |
| NLD | A | 80 | 16.46±6.16 | -3.556 | 0.001 |
| B | 20 | 22.19±7.50 |
| ALD | A | 80 | 13.07±5.35 | -1.160 | 0.249 |
| B | 20 | 14.59±4.76 |
| Phaco energy | A | 80 | 48.19±5.63 | -6.572 | <0.001 |
| B | 20 | 58.25±7.82 |
| Phaco time | A | 80 | 12.67±5.23 | -4.762 | <0.001 |
| B | 20 | 19.80±8.42 |
p-value of <0.05 considered statistically significant
Comparison of Scheimpflug parameters (PNS score, NLD, ALD) and phacoemulsification parameters (power and time) with post-operative Intraocular Pressure (IOP). Group A: Normal IOP, Group B: Increased IOP.
| Parameters | Group | No. of patients | Mean±SD | t-value | p-value |
|---|
| PNS score | A | 96 | 2.32±1.41 | -1.979 | 0.051 |
| B | 4 | 3.75±1.50 |
| NLD | A | 96 | 17.41±6.79 | -1.389 | 0.168 |
| B | 4 | 22.22±6.43 |
| ALD | A | 96 | 13.40±5.34 | 0.233 | 0.817 |
| B | 4 | 12.77±2.78 |
| Phaco energy | A | 96 | 50.05±7.05 | -0.991 | 0.324 |
| B | 4 | 53.75±13.15 |
| Phaco time | A | 96 | 13.87±6.53 | -1.683 | 0.095 |
| B | 4 | 19.50±6.95 |
p-value of <0.05 considered statistically significant
A total of 90 patients (90%) had UCVA between 6/60-6/12, 9 patients (9%) had UCVA less than 6/60 and 1 patient (1%) had UCVA better than 6/12 at 1 week. At 4 weeks, 78 patients (78%) had UCVA between 6/60-6/12, 9 patients (19%) had UCVA better than 6/12 and 3 patients (3%) had UCVA less than <6/60. 81 patients (81%) had UCVA 6/60-612, 19 patients (19%) had UCVA better than 6/12 and no patients with UCVA less than 6/60 at 12 weeks. In addition, 95 patients (95%) patients had BCVA better than or equal to 6/12 and 5% patients (5%) had BCVA less than 6/12 at 4 weeks. However, at 12 weeks 100% patients showed BCVA of 6/12 or better. 95 (95%) patients had refractive error within -1.0 to +1.0 dioptre.
Discussion
The aim of the present study was to evaluate the correlation of age-related cataract using Scheimpflug imaging system (Pentacam) with phacoemulsification parameters. A positive correlation was found between the Scheimpflug parameters and phacoemulsification parameters. As the density of lens increases, more phaco power is likely to be used and consequently more time is required for nucleus emulsification.
Nixon DR found that pre-operatively adjusted phacoemulsification parameters based on PNS scores helped improve overall phacoemulsification energy, time and fluids used in eye [20]. Gupta M et al., found that Scheimpflug maximum nuclear density had a stronger correlation with phacoemulsification power and total ultrasound energy (Z=3.77; p=0.01, Z=2.56; p=0.01) as compared to Lens Opacities Classification System III (LOCS III) [21]. In a study by Kim JS et al., it was found that phacoemulsification parameters had a stronger relationship with lens nuclear density (r=0.797) than with LOCS III Nuclear Opacity (NO) and Nuclear Color (NC) scores (r=0.614, r=0.637, respectively) [22]. Faria-Correia F et al., showed that 3D derived and ROI derived average and maximum lens density correlation with cumulative dissipated energy and total ultrasound time of phacoemulsification [23]. In contrast to the study, Faria-Correia F et al., showed that in age-related nuclear cataract PNS score did not correlate with effective phacoemulsification time as they considered only mild nuclear cataract in their study (rho=0.124, p=0.390) [24]. Al-Khateeb G et al., showed that as the lens density increased, cumulative dissipated energy also increased and ALD showed a significant correlation. They found a moderate correlation of PNS grades with cumulative dissipated energy and total ultrasound time [25]. Demircan S et al., also found significant correlation between phacoemulsification dynamics and Pentacam lens densitometry values [26]. Lim SA et al., analysed nuclear cataract based on patients age and found that Scheimpflug lens density correlated better than LOCS III in patients over 70 years of age [27]. Lim SA et al., also found a significant positive correlation of Scheimpflug lens density and cumulative dissipated energy [28].
According to WHO classification, the study showed a good visual outcome (good: 6/6-6/18; borderline: <6/18-6/60; poor: <6/60) after phacoemulsification. Therefore, it can be concluded that timely intervention for cataract can lead to improved visual outcomes. In the study phacoemulsification was uneventful. This is in consistent with study by Kim JS et al., in which no intraoperative complications occurred [22]. In the study, post-operative corneal oedema had significant correlation with Scheimpflug parameters, phaco power and time. Hence, it can be concluded that with increasing density and PNS score on Scheimpflug imaging system, more power is required during phacoemulsification and therefore this post-operative complication may be predicted.
For that reason, adjusting phacoemulsification parameters based on pre-operative grading of cataract is a promising way to improve overall efficiency of the surgery- allowing antecedent determination of probable intraoperative phacoemulsification parameters and post-operative complications. Timely intervention for cataract and incorporating Scheimpflug imaging system in the diagnostic evaluation of every cataract case undergoing surgery, can lead to improved visual outcomes.
Limitation(s)
One limitation encountered in this study was exclusion of those cataract patients from analysis with respect to PNS where the software was not able to analyse the data. For the above, it can be postulated that fixation to light source is essential for proper analysis by PNS software. Another limitation is that Pentacam is an expensive tool for cataract grading, so may not be available in resource limited settings.
Conclusion(s)
PNS software is a useful additional tool for evaluation of cataract. It offers objective measurements of lens density. Pre-operatively, it can help in predicting phacodynamics (phacoemulsification power and time). Phacoemulsification parameters individualised for each patient lead to use of accurate amount of phacoemulsification energy, resulting in quicker and better visual rehabilitation besides avoiding intraoperative complications.
p-value of <0.05 considered statistically significant
p-value of <0.05 considered statistically significant