Liver transplantation is the only solution or treatment of decompensated chronic liver disease and it becomes more difficult when there is shortage of organ donor leading to mortality. Here an unusual case of a 62 year old male patient of decompensated chronic liver disease with Hepatocellular Carcinoma (HCC) is reported who underwent a Deceased Donor Liver Transplant (DDLT). Intraoperatively patient was found to have a new onset Inferior Vana Cava (IVC) thrombosis, which posed technical difficulty in caval anastomosis and risk of thrombus propagation with standard techniques. Patient also had azygous continuity, where azygous vein was tortuous and was draining entire abdominal, pelvic and lower limb venous return into systemic circulation. Hence, piggyback reconstruction was used; the native vena cava was ligated infra hepatically and allowed azygous to remain sole drainage. This reduced risk of future thrombus propagation into IVC, also eliminated risk of unhealthy vascular anastomosis. There are very few case reports regarding azygous continuity in liver transplant surgery. As per the literature search this is the first case such reconstruction in setting of DDLT from India.
Azygous vein, Hepatocellular carcinoma, Piggyback reconstruction
Case Report
A 62-year-old male patient with 8 months history of hepatitis B (HBV) related chronic liver disease presented to the hospital in August 2018. He was on regular antivirals, and his HBV viral load was low. On work up, his Na-MELD (sodium related model for end stage liver disease) score was 27 with Child Pugh score of 9. He had decompensations in the form of diuretics controlled ascites, two episodes of hepato-renal syndrome and two episodes of hepatic encephalopathy, in last 8 months. On imaging, he was found to have two liver lesions, one each in segment VI and VII, measuring 1 cm × 1 cm and 1.5 cm × 1 cm respectively, with features of HCC (arterial enhancement with early portal and venous washout). His serum AFP level was normal and PET scan was negative for extrahepatic spread. He also had chronic partial Portal Vein Thrombus (PVT) (Yerdel’s Grade I), which was not tumour thrombus [1].
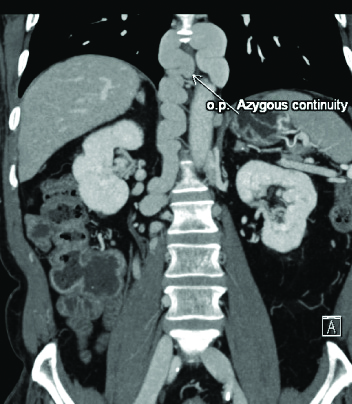
He was listed for liver transplant. As there was no suitable living donor in family, he was put on cadaveric organ waiting list. He was on regular follow-up meanwhile. Four months after listing, he was allotted a match, and he was planned for DDLT, in November 2018. As a routine protocol his laboratory, tumour markers and imaging were repeated before surgery. His tumour markers were normal (AFP <5 ng/mL, CA 19- 9-10.57 U/mL, Carcino Embryonic Antigen- 3.43 ng/mL). Although, his imaging was suggestive of thrombosed intrahepatic IVC, with thrombus extending inferiorly up to renal veins. Superiorly, thrombus extended just below orifices of hepatic vein, with hepatic venous outflow well maintained. His HCC and PVT showed no change in size. Interestingly, he had multiple collaterals with a very tortuous azygous, virtually providing entire infra-diaphragmatic venous drainage [Table/Fig-1]. His Chest CT was unremarkable.
Preoperative CT (abdomen) showing cirrhotic liver with new onset IVC thrombus with calcifications and tortuous azygous vein.

The piggyback modification was planned, but after explants hepatectomy, the native cava was seen extremely calcified and thrombosed. The wall of suprarenal IVC were seen extremely friable with minimal flow in it. Hence, decision was taken to ligate suprarenal IVC and allow azygous vein to be sole venous drainage. Supra hepatic, Portal, hepatic arterial and ductal anastomoses were done in classical manner. Intraoperative portal thrombectomy was performed prior to portal anastomosis which established good flow.
Post-operative course was uneventful. His successive liver dopplers showed good inflow and outflow. His renal functions were normal throughout. Histopathology report of explanted liver specimen confirmed the diagnosis of HBV related cirrhosis with HCC. His ascites was relieved and drains were removed on day 5. His prothrombotic work up (factor V mutation, lupus anticoagulant, protein C, protein S, JAK2 mutation, anticardiolipin antibody, beta 2 glycoprotein antibody) was negative. He was discharged on day 8. He was kept on Low molecular weight heparin for 3 months and then on oral antiplatelets for lifelong, in the form of oral aspirin 150 mg daily. His imaging was repeated at 3 and 6 months post-operative, which showed azygous draining infra diaphragmatic venous return, with hepatic veins providing good venous outflow to liver and no tumour recurrence [Table/Fig-2].
Postoperative CT (Abdomen) showing transplanted liver graft with azygous continuity, where azygous vein is seen providing, systemic venous drainage to infrahepatic portion.
Discussion
Liver transplantation is the only definitive treatment for patients with decompensated chronic liver disease. Organ shortage is biggest hurdle for transplantations worldwide, increasing the waiting list mortality. In India, number of patient requiring liver transplantation annually is approximately 20,000, whereas the actual number of liver transplants taking place is around 1000 per year [2]. HBV related liver cirrhosis is 3rd most common aetiology after hepatitis C and alcoholic cirrhosis in India while HCC as aetiology makes up to only 10% cases [3,4]. In cases of HCC related chronic liver disease, it is important to perform transplant earlier, before the extra hepatic spread of the disease making it inoperable. Living donor liver transplant is better option for these patients. In index case, unfortunately, there was no suitable related donor available, leaving the cadaveric donor only option for him.
Technically, liver transplantation is a challenging surgical procedure as it involves performance of multiple anastomoses, namely: a) Vena cava; b) portal venous; c) hepatic arterial; and d) bile duct anastomosis. According to type of Vena cava anastomosis performed, there are 3 main types of liver transplant: 1) Classical/standard method; 2) Piggyback method; 3) Belghiti modification of piggyback method. The classical method involves removal of intrahepatic cava with liver. Reconstruction is achieved by anastomosing graft cava to suprahepatic and infra hepatic IVC stumps, as described originally by Starlz T et al., [5]. It involves complete caval clamping. To reduce the effects of complete caval clamping, piggyback technique is used where a partial caval clamp is applied after removing liver while keeping recipient IVC in situ [6]. Graft cava is anatomosed to hepatic vein stumps of native cava. The Belghiti modification is similar to piggyback technique except that it uses side to side caval anastomosed [7].
In index case, initially, the plan was for a classical technique, to remove the diseased and thrombosed cava. However, intraoperatively it was found that infra hepatic cava was calcified and thrombosed just up to the renal veins. Anastomosing this cava to graft cava had few theoretical risks, namely: a) vascular anastomosis with friable and calcified vessel may lead to poor anastomosis. Such anastomosis carries high risk of dehiscence and may lead to catastrophic bleeding; b) As the aetiology of rapid development of thrombus was unknown, there was risk of thrombus propagation across the anastomosis. Inferior propagation of thrombus might have put renal venous outflow in risk. So, it was decided to go for piggyback technique. However, the flow across suprarenal IVC was very minimal, so to avoid risking kidneys the native infra hepatic cava were ligated. It was concluded that tortuous azygous was large enough to drain the infra diaphragmatic venous return, as it was the best intraoperative option available.
Azygous continuity (also known as azygous continuation of inferior vena cava) is a condition where, there is termination of IVC below hepatic veins and systemic flow beyond this point is accommodated by dilated azygous and hemiazygos vein, which empty into SVC. This is seen more commonly as a developmental anomaly than an acquired condition like in index case, with incidence of 0.2-3% [8]. It is more commonly seen in association with congenital heart diseases, dextrocardia, asplenia, polysplenia, biliary atresia [8]. In rare cases with left sided IVC, similar continuation is seen through hemiazygous vein. It is important to identify this pre-operatively, as dilated azygous may be perceived as right-sided paratracheal mass or retrocrural adenopathy. In index case, though patient did not have congenital anomaly, due to his IVC thrombus, he had functional azygous continuation.
There are very few reports available of azygous continuity in Liver transplantation. First successful orthotopic DDLT in an asymptomatic adult with an interrupted IVC and azygous continuation was reported in 2012 by Zinser M and Hanto D [9]. In the same year, Hatipoglu S et al., reported living donor liver transplantation in a patient with absent IVC [10]. Eldeen FZ and Alsebayel M, reported a case of 71-year-old male undergoing living donor liver transplant with interrupted left sided IVC with azygous continuity [11]. As per the present clinicians review, no such case report has been published in India. In index case, a recent onset rapidly progressed IVC thrombus completely narrowed the intrahepatic IVC, leading to compensatory azygous dilatation. Due to technically challenging and risky vascular reconstruction, the present authors relied on azygous vein for abdominal and lower limb venous return and ligated the infra hepatic native IVC. There was no postoperative complication seen due to this and patient recovered well and doing fine till his last follow-up.
Conclusion(s)
Inferior Vana Cava (IVC) anomalies, thrombus, strictures are very rare, identifying these preoperatively on imaging is very crucial in planning of liver transplant. Azygous continuity is not a contraindication for liver transplant surgery, rather it can aid in venous return post transplant. An experienced and skilled surgical and anaesthetic team is required to deal with such intraoperative challenges.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 28, 2020
Manual Googling: Apr 22, 2020
iThenticate Software: May 11, 2020 (8%)
[1]. Yerdel M, Gunson B, Mirza D, Karayalcin K, Olliff S, Buckels J, Portal vein thrombosis in adults undergoing liver transplantation: Risk factors, screening, management, and outcomeTransplantation 2000 69:1873-81.10.1097/00007890-200005150-0002310830225 [Google Scholar] [CrossRef] [PubMed]
[2]. Soin A, Kakodkar R, Living donor liver transplantation in IndiaTrop Gastroenterol 2007 28:96-98. [Google Scholar]
[3]. Shukla A, Vadeyar H, Rela M, Shah S, Liver transplantation east versus westJ Clin Exp Hepatol 2013 3:243-53.10.1016/j.jceh.2013.08.00425755506 [Google Scholar] [CrossRef] [PubMed]
[4]. Kakodkar R, Soin A, Liver transplantation for HCC: A reviewIndian J Surg 2012 74:100-17.10.1007/s12262-011-0387-223372314 [Google Scholar] [CrossRef] [PubMed]
[5]. Starzl T, Groth C, Brettschneider L, Orthotopic homotransplantation of the human liverAnn Surg 1968 168(3):392-415.10.1097/00000658-196809000-000094877589 [Google Scholar] [CrossRef] [PubMed]
[6]. Tzakis A, Todo S, Starzl T, Orthotopic liver transplantation with preservation of the inferior vena cavaAnn Surg 1989 210(5):649-52.10.1097/00000658-198911000-000132818033 [Google Scholar] [CrossRef] [PubMed]
[7]. Belghiti J, Panis Y, Sauvanet A, Gayet B, Fekete F, A new technique of side to side caval anastomosis during orthotopic hepatic transplantation without inferior vena caval occlusionSurg Gynecol Obstet 1992 175(3):270-72. [Google Scholar]
[8]. Chaudhary S, Kamyab A, Jacobs M, Congenitally absent inferior vena cavaAm Surg 2013 79:E202-03.10.1177/000313481307900510 [Google Scholar] [CrossRef]
[9]. Zinser M, Hanto D, Liver transplantation in a patient with developmental interruption of the inferior vena cava with azygos substitutionTransplant Proc 2012 44:1460-63.10.1016/j.transproceed.2012.01.12122664037 [Google Scholar] [CrossRef] [PubMed]
[10]. Hatipoglu S, Olmez A, Ozgor D, Living donor liver transplantation in the absence of inferior vena cava: a case reportTransplant Proc 2012 44:1761-63.10.1016/j.transproceed.2012.05.05322841266 [Google Scholar] [CrossRef] [PubMed]
[11]. Eldeen FZ, Alsebayel M, Living Donor Liver Transplantation in so-called “Absent Inferior Vena Cava”: Case ReportAnnals of Saudi Medicine 2013 33(2):60-61. [Google Scholar]