Introduction
Antibiotic nails are taking over the traditional method of fixation of open fractures of tibia now and are becoming a treatment of choice for Gustilo Type I, II and IIIA fractures. They not only hasten the bone union as a single step procedure, but also decrease the systemic side effects of parenteral antibiotics postoperatively. These nails elute the antibiotic exactly in right doses where it is needed to combat the infection and prevent a possible delayed union or hostile environment in Gustilo type I, II and IIIA compound tibial fractures.
Aim
To study the clinical and radiological outcome of antibiotic impregnated Intramedullary (IM) nailing in compound tibial fractures.
Materials and Methods
Twenty five adults having compound tibial shaft fractures of Gustilo Type I and Type II and IIIA were treated with antibiotic impregnated IM nails to evaluate the outcome. Data collection, compilation, and analysis performed using microsoft excel 2007.
Results
Results were excellent to good in 92% (Lysholm’s scale). Partial weight bearing commenced at 5.44 weeks and full weight bearing after 10.48 weeks of operation on an average. Radiological union achieved in 12 to 18 weeks (average 15.55 weeks) in all AO (Arbeitsgemeinschaft für Osteosynthesefragen, German for “Association for the Study of Internal Fixation”) group A, group B fractures with Gustilo type I injury. Complex (AO group C), while Gustilo type II took 12 to 22 weeks (average 16.69 weeks). One Gustilo type IIIA fracture showed delayed union (beyond 22 weeks). There was minimal incidence of infection [overall 24% (20% in type II- superficial in 12% and deep in 8% cases; 4% in type IIIA-deep)]. One Gustilo type IIIA fracture showed infection along the deeper tissue planes.
Conclusion
Antibiotic impregnated nails can be a trustworthy alternative single stage treatment modality, obviating the need of multiple procedures to achieve the bony union in open fractures of tibia.
Delayed union, Gustilo, Infection, Lysholm’s scale
Introduction
Polytrauma patients having open long bone fractures with associated severe soft tissue damage and wound contamination are common now-a-days which put the skills of orthopaedic surgeons to test [1].
The combination of mechanical instability and infection of these creates a synergistically hostile environment for fracture healing. IM nails were advocated for selected open fractures especially as modern surgical technique and antibiotics have successfully managed the infection even in open fractures [2-4].
Application of a compression plate damages one of the better sources of blood supply to bone i.e., periosteal, which is not the case with tibial nailing [5-8]. IM supply is most important in normal bone, however a bony injury disrupts the IM vascular pattern and after injury, periosteal blood supply becomes prominent source of blood supply to bone.
Thus, after injury there is reversal of blood flow from centrifugal to centripetal pattern and significant recruitment of vessels occurs to provide best conditions for early bone healing. Therefore, during internal fixation, it is important to maintain sufficient stability and vascular support of bone and soft tissue. This can be achieved with minimum exposure, careful handling of fracture and particularly the least possible damage to periosteum which is the major blood supply to bone after the fracture. Interlocking nailing preserves the periosteal blood supply and hence, recommended for closed fractures of tibial shaft in adults. Delayed interlocked nailing is done in grade 1 and grade 2 open fractures after healing of wound [9,10].
Patient with an open tibial fracture have a significantly increased risk of infection after injury [11]. Therefore, compound tibial shaft fractures (Gustilo type I or type II and IIIA) fixed with traditional Stainless Steel Intramedullary (SSIM) nails, require a heavy dose of postoperative intravenous antibiotics, causing systemic side effects and increased morbidity in compromised patients. To add further, they still get infection in some cases and implant used for internal fixation itself becomes a potential media for infection, which causes non-union with necrosis of fracture ends because of bacterial adhesion and biofilm formation. They further require infection control first, followed by treatment of the non-union fracture (autologus bone graft at fracture site).
The use of antibiotic impregnated IM nailing for compound fractures of tibia fractures is documented in the literature [12]. Antibiotic impregnated nailing is a single stage treatment modality to overcome troublesome infection and achieve stability. It provides stability across the fracture site, unlike cement beads [12,13]. Secondly, antibiotic impregnation of nail allows higher concentration of antibiotic at the local site (including avascular bony fragments) and is associated with fewer side effects. Antibiotic impregnated nail continues eluting antibiotic at the site of fracture for up to three years and thus, having a positive decisive role in refractory infection [13,14]. Thirdly, antibiotic impregnation will also stimulate the proliferation of osteoblasts in infection free zone around the fracture site thus, enhancing the rate of new healthy bone tissue formation and strong fixation of the bone.
Therefore, a solid fixation from day one, local release of the antibiotics at the fracture site eliminates the chances of postoperative infection, fracture end necrosis, non-union largely and thus, hasten the bony union and decreases the morbidity.
Therefore, keeping in mind the above stated factors as a must for union of compound tibial fractures, the present study was conducted with the aim to study the clinical and radiological outcome of antibiotic impregnated Intramedullary (IM) nailing in compound tibial fractures.
Materials and Methods
In the present prospective study, 25 adults having compound tibial shaft fractures of Gustilo Type I, Type II and IIIA were managed with antibiotic impregnated IM nails, at a tertiary institute of Punjab, India from June 2018 to May 2019. They were evaluated for the outcome. This research was approved by the Ethical Committee (GMC/1048/2k18) of the institution and was done after having patient’s consent for their involvement in the study.
Inclusion Criteria
Skeletally mature patients,
Gustilo type I and II and IIIA fractures,
Fractures distal to tibial tuberosity,
Fractures 4 cm proximal the ankle joint.
Exclusion Criteria
Intra articular tibial fracture around knee,
Malignancy (primary or metastatic),
Intra articular fractures of distal 1/3rd of tibia near ankle joint,
Closed tibial fractures,
Gustilo type IIIB, IIIC fractures,
Patients having co-morbidities like diabetes mellitus, uncontrolled hypertension, patients on steroid therapy, thyroid abnormality and hyperactive parathyroids.
Patients who were chronic alcoholic, drug addicts, chronic smokers and mentally challenged patients, patients with deranged Liver Function Tests (LFT) and/or deranged renal function tests.
Patients medically unfit for surgery.
History regarding mode and mechanism of injury was documented followed by standard emergency evaluation and investigations. Wound irrigation of open fractures with three litres of normal saline, debridement and primary suturing was performed where possible. Plaster of Paris (POP) back splintage and sending cultures was done as initial measures in those cases that didn’t report to institution within the recommended golden period of six hours and more when the edges of their wounds were soiled due to road side accidents. If the cultures were sterile, the patient was posted for surgery; if not, patient was put on parenteral antibiotics, depending upon growth and sensitivity of organism, in recommended dosage as per literature till his cultures showed no growth and Erythrocyte Sedimentation Rate (ESR) and Connective Tissue Reactive (CRP) levels returned to normal. Thereafter, the patients were planned for surgery. Although it increased the hospital stay for a few more days, but it was worth it. X-rays were done in two views. All the patients were operated under spinal anaesthesia with standard nailing technique. Commercially available cytocompatible Gentamicin eluting tibial nail was used. It is a nail with double coating (to provide better adhesion as compared to dip coating) of the antibiotic, with a coat thickness of 50 micron measured by Scanning Electron Microscopy (SEM). The manufacturer provided the uniform coating of antibiotic over the nail by high velocity spray coating technique. The concentration of the drug in it was 1 mg. per square cm. Total drug on an average size nail was 100 mg. The drug postoperatively released with an initial burst of 30-40% in first 3-4 days with an initial highest concentration locally up to 200 microgram/ml which prevented and destroyed the colonsation of invading bacteria. This was followed by the sustained release of the antibiotic for another 4-8 weeks maintaining local drug levels high enough for the bactericidal activity in a period, most susceptible to infections postoperatively.
X-rays were done postoperatively to confirm the adequacy of reduction. Parenteral broad spectrum antibiotics {cefuroxime (1.5 gm BD+ amikacin (25 mg/kg) BD} were given for initial seven days and then, switched over to oral antibiotics for another seven days. Static exercises commenced on the second day and touchdown weight bearing with walker allowed on third postoperative. day. Sutures were removed on 10th postoperative day. All the cases were followed-up in the Out Patient Department (OPD) at six weeks, 12 weeks and six months and thereafter at regular intervals until clinical and radiological union occurred.
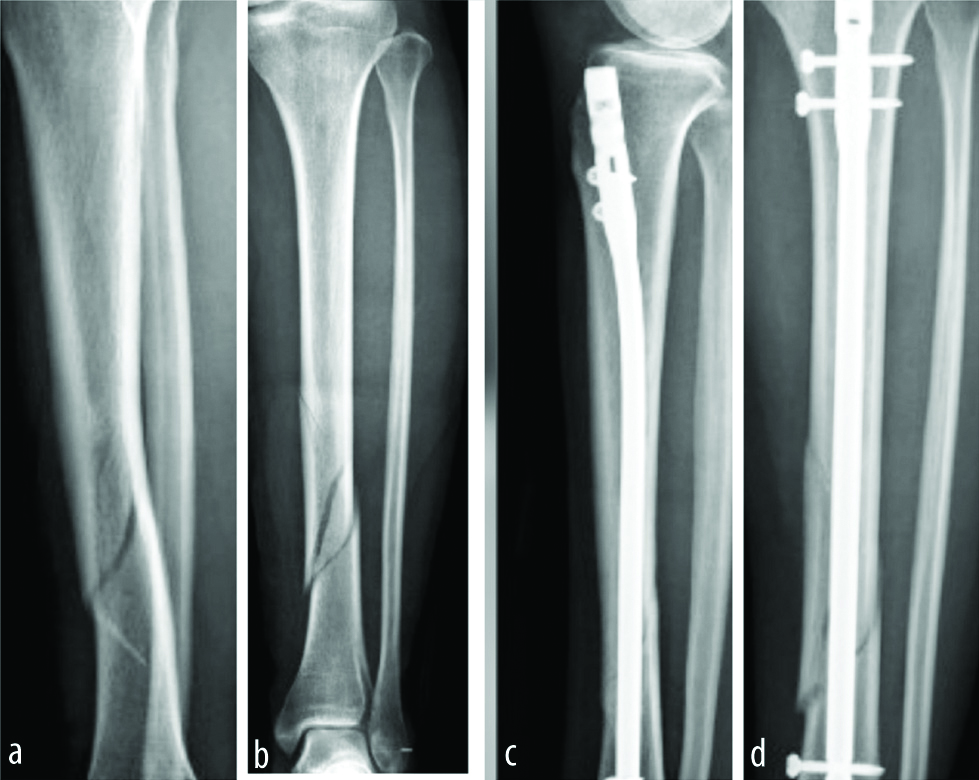
Time of union: Clinical signs of union were taken as no pain, warmth or redness at the fracture site and unrestricted weight bearing. Radiological signs of union included appearance of callus in three out of four cortices, obliteration of fracture line, homogenous bone structure, trabecular and cortical continuity. Following arbitrary standards of rate of union were adopted: Normal union 12-20 weeks; Accelerated union <12 weeks; Delayed union >20 weeks. Radiological union was achieved in 12 to 18 weeks (average 15.55 weeks) in all AO group A, group B fractures with Gustilo type I injury [Table/Fig-1]. Complex AO group C with Gustilo type II took 12 to 22 weeks (average 16.69 weeks) [Table/Fig-2] for radiological union.
Catalogue of implant used. a,b) Preoperative X-rays (ap and lateral) showing AO group A fracture (gustilo type I); c,d) Postoperative X-rays (ap and lateral) showing uniting fracture in AO group.
a) Preoperative wound (gustilo Type II); b) Healed wound; c) X-ray of complex AO group C (gustilo type II) showing united fracture.

Results were graded as excellent, good, fair and poor as per Lysholm criteria [15] [Table/Fig-3] to assess postoperative functionality of the knee joint [Table/Fig-4,5]. Results were graded as-
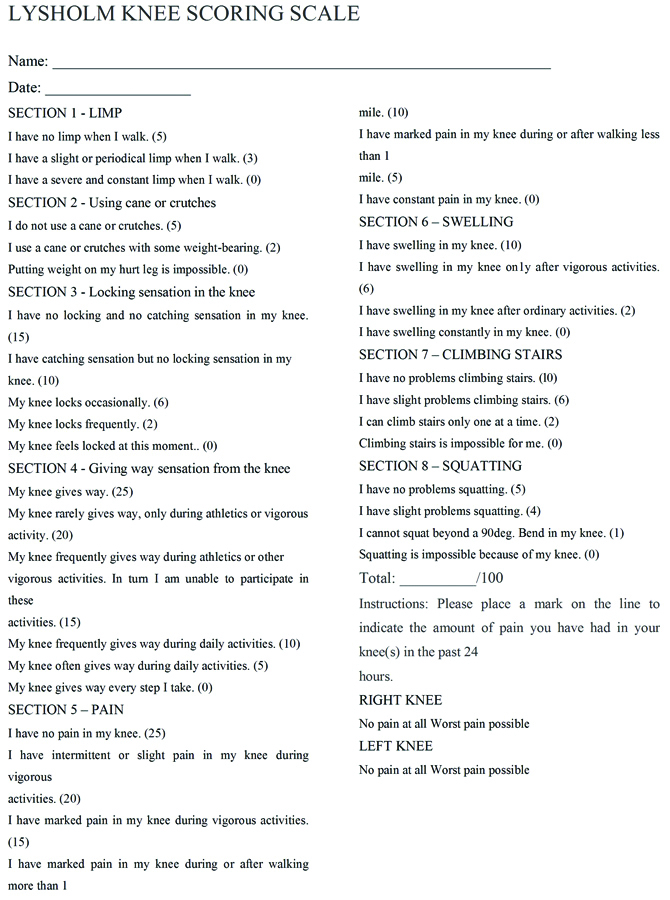
Results as per lysholm scale.
| Sl. No. | | Parameters | Score |
|---|
| 01. | Limping | NeverMildStrong | 19 (76%)6 (24%)0 |
| 02. | Support | No SupportWalking StickImpossible | 22 (88%)3 (12%)0 |
| 03. | Restraining | No RestrainingHas The Feel of RestrainingOccasional RestrainingFrequent Restraining | 15 (60%)7 (28%)2 (8%)1 (4%) |
| 04. | Instability | Never Miss a StepSeldom Miss a StepFrequent Miss a Step | 20 (80%)3 (12%)2 (8%) |
| 05. | Pain | No PainMild During ExerciseModerate During ExercisePain With Walking> 2 KmPain With Walkin<2 km | 21(84%)2 (8%)1 (4%)1 (4%)0 |
| 06. | Swelling | No SwellingSwelling on Strong EffortSwelling on Mild EffortContinuous Swelling | 16 (64%)5 (20%)3 (12%)1 (4%) |
| 07. | Climbing Stairs | No Problem 21Slightly DamagedOne Step at a TimeImpossible | (84%)3 (12%)1 (4%)0 |
| 08. | Squatting | No ProblemSlightly DamagedNot More Than 90 DegreeImpossible | 22 (88%)3 (12%)00 |
| 09. | Complications | No InfectionSuperficial InfectionDeep Infection | 19 (76%)5 (20%)1 (4%) |
Postoperative functionality at knee joint.

Excellent when the score was 90-100,
Good with a score of 84-89,
Fair when the score was 83-64.
Statistical Analysis
The results of observations of individual patients were pooled. Data collection, compilation and analysis performed using microsoft excel 2007 (any type of statistical analysis was not needed, so simple percentage values were calculated using Microsoft excel 2007).
Results
A union rate of 100% was achieved in present study with 92% excellent to good results, as per lysholm scale [Table/Fig-6]. Partial weight bearing commenced at 5.44 weeks on an average and full weight bearing on an average after 10.48 weeks of surgery. Only six out of 25 cases needed eradication of infection (superficial in five and deep in one case) with systemic antibiotics for more than stipulated period and eventually increasing the union time.
| Parameter | N (Percentage) |
|---|
| Age (Years) | 21-30 | 12 (48%) |
| 31-40 | 07 (28%) |
| 41-50 | 04 (16%) |
| 51-60 | 01 (04%) |
| 61-70 | 01 (04%) |
| Sex | Male | 21 (84%) |
| Female | 04 (16%) |
| Side | Right | 15 (60%) |
| Left | 10 (40%) |
| Mode of Injury | Road side accidents | 20 (80%) |
| Direct trauma | 02 (08%) |
| Fall | 03 (12%) |
| Distribution of cases (Gustilo anderson classification) | Gustilo Type I | 13 (52%) |
| Gustilo Type Ii | 11 (36%) |
| Gustilo Type Iiia | 01 (04%) |
| Associated Injuries | Fracture fibula | 21 (84%) |
| Fracture femur | 01 (04%) |
| Head injury | 01 (04%) |
| Bimalleolar fracture | 01 (04%) |
| Chest injury | 01(04%) |
| Distribution of cases (Ao classification) | Type I | 20 (80%) |
| Type II | 04 (16%) |
| Type III | 01 (04%) |
| Location of tibial shaft fractures | Upper 1/3 | 03 (12%) |
| Middle 1/3 | 13 (52%) |
| Lower 1/3 | 09 (36%) |
| Time of union | 12-24 weeks | 24 (96%) |
| More than 24 weeks | 01 (04%) |
| Functional results (Lysholm scale) | Excellent | 18 (72%) |
| Good | 05 (20%) |
| Fair | 02 (08%) |
| Complications | Residual deformity | 01 (04%) |
| Anterior knee pain | 07 (28%) |
| Cpn palsy | 01 (04%) |
| Hypertrophy of scar | 01 (04%) |
| Infection | 06 (24%) |
| No complications | 09 (36%) |
The patients advised follow-up visits at 6, 12, 24 weeks and thereafter, at six months to assess the progress of union radiologically, wound condition and for implant failure if any. The shortest time to union was 12 weeks in group A fractures with Gustilo type I injury and longest was 22 weeks in group B with Gustilo type II fracture. There was one case with Gustilo type IIIA fracture which showed delayed union (beyond 22 weeks) due to infection along the deeper tissue planes in that case.
With regular physiotherapy and active movements of knee, full range of flexion returned in all cases. After about five weeks of active movements of ankle, all patients had near normal or normal range of ankle movement. There was no clawing of toes postoperatively. There was no case of fat embolism/ amputation of limb/ postoperative death.
Discussion
In the present study, 25 cases of compound factures of the tibia were treated with antibiotic impregnated tibial nail. In present series, 80% of the fractures were due to high velocity road traffic accidents, 12% were due to fall and 8% were as a result of direct trauma. This was comparable to earlier studies [16-18].
Various researchers have documented the importance of local elution of antibiotic as a game changer for achieving union in compound fractures of tibia. Raschke MJ et al., quoted that an IM tibia nail with antibiotic coating proved to be a useful tool in the treatment of tibia fractures in patients with a higher risk of developing implant-related infections. Gentamicin impregnated tibia nail reduced deep infections and prevented long-term external fixation [19].
Thonse R and Convey J treated infected non-union and segmental bone defects of tibia with antibiotic cement-coated interlocking nail. They managed 20 patients by this and found that 17 (85%) patients, got bony union. Three patients (15%), had control of infection with stable non-union (one patient) and stable non-union with cement spacer (two patients). Nineteen (95%) patients achieved control of infection except for one patient, who had a bony union with intermittent wound discharge finally landing in above knee amputation. Three patients (15%) needed exchange nailing to another antibiotic cement-coated nail in order to achieve infection free union [20].
Metsemakers WJ et al., treated 16 consecutive patients with 16 tibia fractures from a gentamycin-coated IM nail. Among them, 11 (68.8%) with acute fractures were treated with a gentamicin-coated IM nail; rest five were complex revision cases (31.2%). No deep infections noted after the treatment with a gentamicin-coated tibia nail [21].
Bharti A et al., postulated that local antibiotic delivery system through antibiotic impregnated Poly Methyl Methacrylate (PMMA) rods holds a promising modality of treatment for handling difficult to control, chronic infections and promotes bony union. They achieved union in five patients (71%) at mean follow-up of 7.28 months. No infection was there in six cases (85.7%), out of which four cases (57%) had good union and two had (29%) had a non-union. One case was of infected union (14.5%) [22].
Bhatia C et al., concluded that antibiotic cement impregnated nailing is simple, economical and an effective single stage procedure for the management of compound tibial fractures with non-union. They controlled Infection in 95% of the patients and achieved bony union in 60% patients with antibiotic cement nailing [23].
Desouuza C et al., also documented the role of cement coated antibiotic nail in compound fractures of tibia with bony non-unions and advocated its use. There was no infection in 95% of the patients and bony union was achieved in 60% patients with antibiotic cement nailing with average time of union of 32 weeks [24].
In the present study, results were better when compared with above quoted studies as 100% union achieved with overall infection rate of 24% only. Infection did not hinder the union and resolved with local antibiotic release through nail and concurrent administration of systemic antibiotics.
Limitation(s)
The small size of the sample and affordability of the implant were the limitations of the present study. More studies on a larger data base are needed to corroborate findings of the present study.
Conclusion(s)
Antibiotic impregnated nailing is a very effective single stage procedure for the management of gustilo type I, II, IIIA compound fractures of tibia. It achieves the goal of early bony union with less morbidity and decreases the complications such as infection and chronic osteomyelitis due to constant elution of antibiotic at the fracture site, obviating the need of intravenous/oral administration of the same, thus decreasing the overall systemic side effects. It also decreases the non-union percentage as the fixation is sound in the absence of infection and enhances the bone formation rate and eventual early fracture union. Also, early range of motion exercises of joints and early weight bearing is permitted because breakage of implant is very uncommon due to load sharing.
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 03, 2020
Manual Googling: Apr 15, 2020
iThenticate Software: May 11, 2020 (9%)
[1]. Gustilo RB, Anderson JT, Prevention of infection in the treatment of one thousand and twenty five open fractures of long bones. Retrospective and prospective analysisJBJS 1976 58-A:453-58.10.2106/00004623-197658040-00004 [Google Scholar] [CrossRef]
[2]. Fader M, Jagardo H, Fracture and dislocation compendium orthopaedic trauma association committee for coding and classificationJ Orthop Trauma 1996 10(supp. 1):01-154. [Google Scholar]
[3]. Kim PH, Leopold SS, Gustilo-Anderson classificationClin Orthop Relat Res. Res 2012 470(11):3270-74.10.1007/s11999-012-2376-622569719 [Google Scholar] [CrossRef] [PubMed]
[4]. Anderson LD, Hutchins WC, Fracture of the tibia and fibula treated with casts and transfixing pinsClin Orthop 1976 150:179 [Google Scholar]
[5]. Bone LB, Johnson KD, Treatment of tibial fractures by reaming and intramedullary nailingJBJS 1986 68-A:87710.2106/00004623-198668060-00009 [Google Scholar] [CrossRef]
[6]. The Blood Supply of Bone. By Murray Brookes, M.A., D.M., D.L.O., Reader and Appointed Teacher of Human Anatomy and Morphology, University of London; Director of Basic Research, Guy’s Hospital, London. 82/5 × 52/5 in. Pp. 338 + ix. Illustrated. 1971. London: Butterworth & Co. (Publishers) Ltd. £6.5; First published: September 1971. https://doi.org/10.1002/bjs.180058093510.1002/bjs.1800580935 [Google Scholar] [CrossRef]
[7]. Strachan RK, McCarthy I, Fleming R, Hughes SP, The role of the tibial nutrient artery. Microsphere estimation of blood flow in the osteotomised canine tibiaJBJS 1990 72(3):391-94.10.1302/0301-620X.72B3.2341434 [Google Scholar] [CrossRef]
[8]. Treuta J, Blood supply and the rate of healing of tibial fracturesClin Orthop 1974 (105):11-26.10.1097/00003086-197411000-00003 [Google Scholar] [CrossRef]
[9]. Ekeland A, Thoreson BO, Alho A, Stromsol K, Folleras G, Haukebo A, Interlocking intramedullary nailing in the treatment of tibial fractures; A report of 45 casesClin Orthop 1988 231:205-15.10.1097/00003086-198806000-00027 [Google Scholar] [CrossRef]
[10]. Mohammad JZ, Keivan A, Mir Mostafa S, Enders nail: Is the old implant effective today?Clin Orthop 2004 3:217-21. [Google Scholar]
[11]. Schemitsch EH, Turchin DC, Kowalski MJ, Swiontkowski MF, Quantitative assessment of bone injury and repair after reamed and unreamed locked intramedullary nailingJ Trauma 1998 45:250-55.10.1097/00005373-199808000-000089715180 [Google Scholar] [CrossRef] [PubMed]
[12]. Riel RU, Gladden PB, A simple method for fashioning an antibiotic cement-coated interlocking intramedullary nailAm J Orthop 2010 39:18-21. [Google Scholar]
[13]. Nelson CK, Hickmon SG, Harrison BH, Elution characteristics of gentamicin-PMMA beads after implantation in humansOrthopedics 1994 17:415-16. [Google Scholar]
[14]. Nizegorodcew T, Palmieri G, Marzetti E, Antibiotic-coated nails in orthopedic and trauma surgery: State of the artInt J Immunopathol Pharmacol 2011 24:125-28.10.1177/03946320110241S22321669150 [Google Scholar] [CrossRef] [PubMed]
[15]. Lysholm J, Gillquist J, Evaluation of knee ligament surgery results with special emphasis on use of a scoring scaleAm J Sports Med 1982 10:150-154.10.1177/0363546582010003066896798 [Google Scholar] [CrossRef] [PubMed]
[16]. Court brown CM, Mc Birnie J, The epidemiology of the tibia fracturesJ Bone Joint Surg 1995 77B:417-21.10.1302/0301-620X.77B3.7744927 [Google Scholar] [CrossRef]
[17]. Giannoudis PV, The role of plating in the operative treatment of severe open tibial fractures: A systematic reviewInt. Orthop 2009 33(1):19-26.10.1007/s00264-007-0443-517786444 [Google Scholar] [CrossRef] [PubMed]
[18]. Michail B, External fixation as a primary and definitive treatment for tibial diaphyseal fracturesSTLR 2009 4(2):81-87.10.1007/s11751-009-0062-319714440 [Google Scholar] [CrossRef] [PubMed]
[19]. Raschke M J, Rosslenbroich SB, Thomas F, Fuchs Antibiotic Coated Nails 2005 Intramedullary Nailing (springer):555-63.10.1007/978-1-4471-6612-2_32 [Google Scholar] [CrossRef]
[20]. Thonse R, Conway J, Antibiotic cement-coated interlocking nail for the treatment of infected nonunion and segmental bone defectsJ. Orthop. Trauma 2007 21(4):258-68.10.1097/BOT.0b013e31803ea9e617414554 [Google Scholar] [CrossRef] [PubMed]
[21]. Metsemakers WJ, Reul M, Nijs S, The use of gentamicin-coated nails in complex open tibia fracture and revision cases: A retrospective analysis of a single centre case series and review of the literatureInjury 2015 46(12):2433-37.10.1016/j.injury.2015.09.02826477343 [Google Scholar] [CrossRef] [PubMed]
[22]. Bharti A, Saroj UK, Vineet K, Sanjay K, Oma BJ, A simple method for fashioning an antibiotic impregnated cemented rod for intramedullary placement in infected non-union of long bonesJ Clin Orthop Trauma 2016 7(Suppl 2):171-76.10.1016/j.jcot.2016.08.00428053381 [Google Scholar] [CrossRef] [PubMed]
[23]. Bhatia C, Tiwari AK, Sharma SB, Thalanki S, Rai A, Role of antibiotic cement coated nailing in infected nonunion of tibiaM Ortho J 2017 1(11):06-11.10.5704/MOJ.1703.01928435567 [Google Scholar] [CrossRef] [PubMed]
[24]. Desouuza C, Nair V, Chaudhary A, Hurkat H, George S, Role of antibiotic cement-coated nailing in infected nonunion of tibiaTrauma International 2018 4(2):18-21. [Google Scholar]