OSA is characterised by repeated episodes of cessation of breathing due to abnormal collapse of upper airway leading to apnea or hypopnea and is by far the most common form of sleep-disordered breathing. T2DM and OSA are the two common and chronic conditions that are associated with each other in a bidirectional [1] relationship i.e., T2DM is a risk factor for OSA and OSA is a risk factor for T2DM.
A two-fold increased rate of OSA in people with prediabetes and morbid obesity, compared to normoglycaemic and morbid obese patients is reported [2]. It is important to be cognizant of the increased likelihood of OSA in obese patients with T2DM, especially in people with higher Body Mass Index (BMI) [3].
This study, also tried to find a co-relation between AHI and HbA1c as poor glycaemic control has been observed due to undiagnosed OSA in obese patients with T2DM which further increases the risk of serious complications. The primary aim was to study the prevalence of OSA in Obese patients with T2DM.
Materials and Methods
This was a cross-sectional study carried out in patients attending the Out-Patient Departments (OPDs) of TB and Respiratory Diseases and Endocrinology, from 1st September 2017 to 31st March 2019 after getting an approval from the Ethical Committee (Dean/2017/EC/198). The consent was taken from participants.
Inclusion criteria: Participants included in the study were obese adults with T2DM.
Exclusion criteria: Pregnant females, participants taking treatment for OSA, having any chronic pulmonary condition, respiratory failure, or on domiciliary oxygen therapy, having any pre-existing cardiovascular disease, hepatic disease or neuromuscular/neurological disorders, having history of drug abuse or alcoholism (consumption of alcohol (ethanol) for more than 4 nights per week as per CAGE criteria) [4].
Data on demographic characteristics, medical history, medications, habits and sleep using Epworth Sleepiness Scale [5] were obtained before the initiation of overnight unattended polysomnography.
Each patient’s height, weight, neck circumference, waist circumference, abdominal girth and BMI were measured. Routine blood investigations like Complete Blood Count (CBC), Liver Function Test (LFT), Renal Function Test (RFT), blood sugar level i.e., fasting blood sugar and postprandial blood sugar and HbA1c were done. T2DM was diagnosed by using the following criteria [6] i.e., symptoms of diabetes plus random blood glucose concentration ≥200 mg/dL and/or Fasting plasma glucose ≥126 mg/dL, and/or Haemoglobin A1c (HbA1c) ≥6.5%, and/or 2-h plasma glucose ≥200 mg/dL. Obesity (BMI >30 Kg/m2) was classified [7] using BMI into Class 1 (30-34.99 Kg/m2), Class 2 (35-39.99 Kg/m2) and Class 3 (≥40.0 Kg/m2). Based on AHI, OSA was classified [8] into Mild (AHI 5 to <15), Moderate (AHI 15 to 30) and Severe (AHI >30) groups.
Statistical Analysis
The statistical analysis was done using statistical software SPSS for windows (version 16). Chi-square test was used for non-parametric variables. Student’s t-test was used for comparing two groups. The p-value <0.05 was stated as statistically significant.
Results
The baseline characteristics of the population are given in [Table/Fig-1].
Baseline data of participants.
| No. of participants | Obese diabetics (N=50) | Obese diabetics with OSA (N=44) |
|---|
| Mean age | 52.68±10.67 | 52.13±10.07 |
| Gender ratio (M:F) | 2.57:1 | 2.66:1 |
| Mean BMI | 34.35±4.36 | 34.82±4.45 |
| Mean HbA1c | 8.85±1.77 | 8.87±1.88 |
Prevalence of OSA in Patients with Obesity and T2DM as per AHI [Table/Fig-2]:
Prevalence of OSA in patients with obesity and type 2 diabetes mellitus as per AHI.
| AHI | Number | Percent |
|---|
| <5 | 6 | 12.0% |
| 5-14 | 16 | 32.0% |
| 15-30 | 13 | 26.0% |
| >30 | 15 | 30.0% |
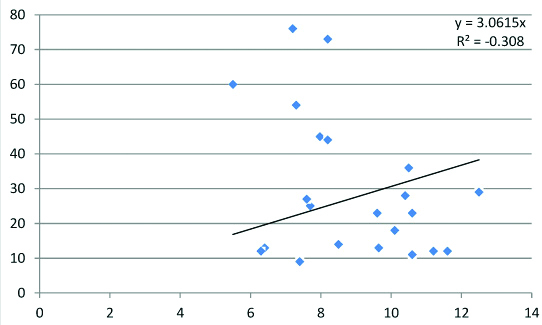
There were total 88% (N=44) of participants {64% male (N=32) and 24% female (N=12)} with obesity and T2DM who had OSA with an AHI ≥5 events/h. The mean AHI was 33.57±24.88 events/h in males and 24.33±18.75 events/h in females. A total of 32% (N=16) of the participants had mild OSA (AHI 5-14), 26% (N=13) had moderate OSA (AHI 15-30), and 30% had severe OSA (AHI≥30) (N=15). A correlational graph between AHI and HbA1c with negative R- square value was obtained [Table/Fig-3].
Correlation graph between AHI and HbA1c in subjects with OSA.
Prevalence of OSA in Patients with Obesity and T2DM as per BMI [Table/Fig-4]:
Prevalence of OSA in patients with obesity and type 2 diabetes mellitus as per BMI.
| BMI (kg/m2) | Female (N=12) | Male (n=32) | Total (n=44) |
|---|
| 30-34.99 | 4 | 24 | 28 |
| 33.3% | 75.0% | 63.6% |
| 35-39.99 | 4 | 8 | 12 |
| 33.3% | 25.0% | 27.3% |
| ≥40.0 | 4 | 0 | 4 |
| 33.3% | 0% | 9.1% |
| Total | 12 | 32 | 44 |
| 100.0% | 100.0% | 100.0% |
χ2=13.270, p=0.001
Twenty eight out of 34 class I obese (BMI- 30-34.99 kg/m2) with T2DM, 12 out of 12 class II obese (BMI- 35-39.99 kg/m2) with T2DM and 4 out of 4 class III obese (BMI ≥40 kg/m2) and T2DM patients had OSA (p-value=0.001).
Prevalence of OSA in Patients with Obesity and T2DM as Per Age:
Mean age in men and women with OSA was 52.06±10.90 and 52.33±7.83, respectively with an insignificant p-value of 0.939. 40.9% OSA subjects were in 41-50 years age group and the maximum subjects with severe OSA (46.7%) were in 51-60 years age group.
Discussion
An obstructive hypopnea/apnea is characterised by a transient reduction in, or complete cessation of breathing due to upper airway collapse and are usually associated with sleep fragmentation, arousals and reduction in oxygen saturation which may eventually lead to development of other significant co-morbidities also. Likely mechanisms are sleep fragmentation and chronic intermittent hypoxia exposure which trigger a systemic inflammatory response [9]. This study mainly focused to diagnose OSA in obese T2DM patients and to evaluate its clinical correlations. In the study, 32% had mild OSA, 26% had moderate OSA, and 30% had severe OSA. A 12% of participants did not have OSA. Mean HbA1c and BMI in participants with OSA was 8.87±1.88 and 34.82±4.45, respectively. An exceedingly high prevalence of undiagnosed OSA i.e., 88% was obtained.
A study done by Foster GD et al., has also reported similar results (86% of participants had OSA including 30.5% with moderate OSA, and 22.6% with severe OSA) in obese patients with T2DM [3].
Studies have demonstrated an approximately 40% prevalence of sleep apnea in moderately overweight men [10,11]. In severe obesity (BMI ≥40 kg/m2), the prevalence of sleep apnea has been estimated to vary between 40 and 90% [12]. Similarly, in this study, there was a high prevalence of OSA (p-value= 0.001) in obese population with T2DM and the prevalence increased with increase in BMI.
These conditions share common risk factors such as obesity and age, which are also risk factors for cardiovascular disease. Obesity, in particular, is a prominent common risk factor for cardiovascular diseases. A 10% increase in weight has been shown to cause a six-fold increase in the risk of developing OSA [13].
OSA occurs approximately in 1 to 2% of middle aged women and 4-9% in middle aged men which increases with age and plateaus at around 65 years [14]. In this study, a majority of the participants with OSA (N= 18, 40.9%) were in 41-50 years age group. So, it appears that OSA affects middle age population with Obesity and T2DM.
OSA is known to be more prevalent among males than females. Epidemiologic studies demonstrate that the prevalence of OSA is two to three times higher in men than women [15,16]. Similarly, this study also observed, in a population 50 subjects comprised of 14 females and 36 males, 12 female subjects (85.71%) and 32 male subjects (88.88%) had OSA i.e., OSA, in patients with Obesity and T2DM, is more prevalent among males than females. Men are more likely to develop sleep apnea than women as men have larger pharyngeal airway cross-sectional area, longer airway length and airway volumes, thus more collapsible [17].
Limitation(s)
A high prevalence, observed in this study, could be due to the small sample size. These results need further evaluation in a larger sample sized population.
Conclusion(s)
The study on obese patients with T2DM concludes a high prevalence of undiagnosed OSA and increased risk of developing OSA in patients with higher BMI. Therefore, early diagnosis by screening methods and investigations should sincerely be considered in patients with obesity and T2DM to help develop early prevention strategies, treatment and to reduce the incidence of various serious OSA, obesity and T2DM disease related complications.
χ2=13.270, p=0.001