Pharmaco-invasive Approach to Acute Coronary Syndrome with Acute Thrombotic Occlusion: A Tough Enemy to Conquer
Rutvik Trivedi1
1 Consultant Cardiologist, Department of Cardiology, Zydus Hospital and Research Centre, Anand-Lambhavel Road, Anand, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rutvik Trivedi, Consultant Cardiologist, Department of Cardiology, Zydus Hospital and Research Centre, Anand-Lambhavel Road, Anand-388001, Gujarat, India.
E-mail: rutviktrivedi78@gmail.com
Acute occlusion of a Saphenous Vein Graft (SVG) is commonly associated with extensive atherosclerotic and thrombotic burden, which increases the risk of distal embolisation and no reflow and thus myocardial infarction and death. To decrease the risk of distal embolisation, embolic protection devices are used. This case report is about two elderly patients admitted with Acute Coronary Syndrome (ACS) due to acute thrombotic SVG occlusion that was recanalized through the complementary nature of two strategies.
Chronic total occlusion, Coronary artery bypass graft, Percutaneous coronary intervention, Saphenous vein graft, Thrombus
Case Report
Case 1
A 69-year-old female presented with complaints of recent onset of chest pain, headache and back pain of seven hours duration. The patient was hypertensive and diabetic. She had a history of ACS due to which she had undergone Coronary Artery Bypass Grafting (CABG) with one venous graft to the Left Anterior Descending (LAD) artery and one to the Right Coronary Artery (RCA) 12 years ago elsewhere. She also had a history of hysterectomy.
On physical examination, heart rate was 80 bpm, respiratory rate was 20 bpm, and blood pressure was 129/87 mmHg. Her Electrocardiography (ECG) performed at that time was suggestive of QS in leads V1 to V4 with 1 mm ST elevation. Laboratory investigations revealed troponin levels of 40 pg/mL. A 2D colour Doppler ECG revealed mild left ventricular systolic dysfunction, Grade 1 left ventricular diastolic dysfunction, concentric left ventricular hypertrophy and a sclerosed aortic valve. Right ventricular systolic pressure was 38 mmHg. In view of symptoms and ECG changes, Coronary Angiography (CAG) was performed. CAG revealed multi-vessel coronary artery disease. LAD had complete ostial occlusion with faint filling of mid-LAD through collaterals from the right conal branch. Mid Left Circumflex Artery (LCx) had 80% occlusion [Table/Fig-1a], whilst mid-RCA also had complete occlusion of a long segment lesion [Table/Fig-1b]. Furthermore, the shaft of the SVG connected to the LAD (SVG-LAD) had acute thrombotic occlusion [Table/Fig-1c] and the shaft of the SVG connected to the RCA (SVG-RCA) had chronic occlusion.
Coronary angiography showing: (a) Mid-LCx 80% occlusion and LAD total occlusion; (b) RCA total occlusion (c) Mid SVG-LAD occlusion with heavy thrombus burden; (d) SVG-LAD lesion crossed with fielder FC guide wire and thrombosuction device parked distally whilst 5 mg alteplase was slowly infused over 5 minutes; (e) First check angiogram after 30 minutes; (f) Second check angiogram after second dose of 2.5 mg alteplase after 30 minutes; (g) 4.0×32 mm stent deployed in mid SVG-LAD lesion; and (h) Final TIMI grade 3 flow and myocardial blush.
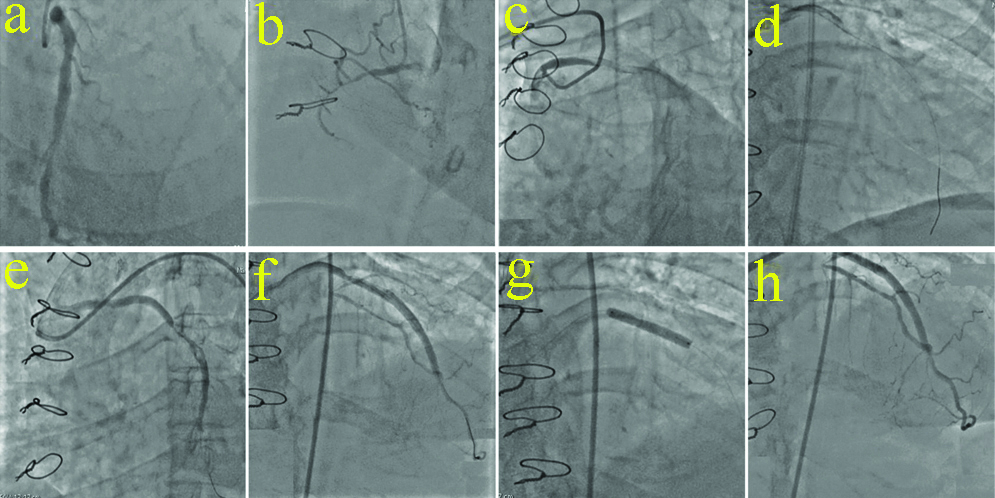
In view of these findings, it was elected to treat the patient through a pharmaco-invasive approach. As there was no space to park a filter, a 6F guiding catheter was used to access the right femoral artery. The SVG-LAD graft lesion was crossed with a Fielder FC (Asahi Corporation, Japan) guidewire and over the wire, a 6F Thrombuster II (Kaneka Corporation) was placed distally and 5 mg alteplase was slowly infused over a period of five minutes [Table/Fig-1d]. The patient’s condition, especially rhythm was monitored for 30 minutes and check angiography was performed [Table/Fig-1e]. Next, a second dose of 2.5 mg alteplase was administered over a period of five minutes. Check angiography was again performed [Table/Fig-1f]. Good TIMI flow was achieved in the graft with 90% stenosis in mid part of the vessel. The graft lesion was then pre-dilated at 10 atm and a 4.0 mm × 32 mm Abluminus Sirolimus-Eluting Stent (SES) (Envision Scientific, India) was subsequently implanted [Table/Fig-1g]. The procedure was successful and TIMI flow 3 was achieved [Table/Fig-1h]. Post-dilatation was avoided as per planned strategy.
Case 2
A 58-year-old male presented with chest pain of four hours duration. He had a history of CABG with four grafts, left internal mammary to LAD, left radial to first Obtuse Marginal (OM) branch, and venous grafts to Ramus Intermedius (RI) ramus artery and Posterior Left ventricular Branch (PLB) 15-years ago.
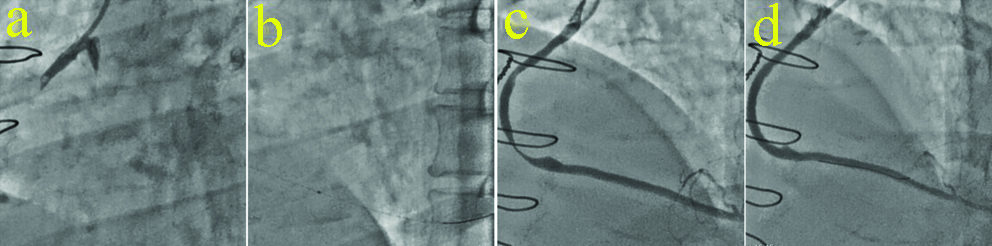
His ECG was suggestive of 1 mm ST-elevation in lead III and aVF with T wave inversion in lead V2-V6, I, aVL with early R wave transition from V1 to V2, suggestive of infero-posterior wall myocardial infarction. His CAG revealed total occlusion of native LAD from mid-LAD with proximal calcification. LCx had 80% distal occlusion, whilst proximal OM2 had 99% occlusion. Proximal native RCA had total occlusion. His LIMA to LAD (LIMA-LAD) graft was normal. The graft connecting Left Radial Artery to OM (LRA-OM) had 80% proximal occlusion with 40% occlusion in the mid segment and 80% distal occlusion before the anastomosis. The graft connection SVG to Posterior Descending Artery (SVG-PDA) had complete thrombotic occlusion [Table/Fig-2a]. A 6F guiding catheter was used to access the right femoral artery and the SVG-PDA graft lesion was crossed with a Fielder FC (Asahi Corporation, Japan) guidewire. A dose of 10 mg alteplase was administered via a Thrombuster II (Kaneka Corporation) and check angiography was performed after 20 minutes [Table/Fig-2b,c]. Good TIMI III flow post thrombolysis was achieved. The residual lesion was stented with 3.5 mm × 44 mm Biomime SES (Meril Life Sciences, India). Post-dilatation was avoided as per planned strategy. The procedure was successful and TIMI flow 3 was achieved [Table/Fig-2d].
Coronary angiography showing: (a) SVG-RCA total thrombotic occlusion; (b) Intragraft infusion of 10 mg alteplase; (c) Post thrombolysis flow in graft; and (d) Post stenting check angiogram.
Discussion
Coronary Artery Bypass Grafting (CABG) is a well-established and frequently practised reperfusion strategy. However, despite routine employment of SVG in such procedures, these grafted venous conduits have been identified as the culprit lesions in 70-80% cases of ACS occurring post CABG [1]. Furthermore, current literature evidence 10-15% venous graft occlusion within the first year and 50% graft failure after 10 years [2]. Thus, SVG failure due to rapid development of atherodegenerative disease elicits a problematic situation and poses a major challenge for interventional cardiologists.
SVG used during CABG are prone to degeneration and occlusion. High attrition rates of these conduits diminish long-term patency and moreover consequence fatal sequelae such as peri-procedural myocardial infarction and death [3]. Patients presenting with ACS triggered by acute thrombotic SVG occlusion constitute a high-risk patient population. This case report describes two such patients treated through the complementary nature of two strategies. It further highlights the complexities associated with intervention of this high-risk patient population.
There is a paucity of robust evidence-based data addressing intervention in this specific patient subset. Retrospective data evidence poor clinical outcomes following intervention of SVG [4]. Hence, native coronary arteries prevail as the target in 65% interventions, whilst SVG is preferred in only 37.5% interventions [5]. Despite strong recommendation for native coronary artery treatment, several other factors should be taken into account when selecting the optimum reperfusion strategy. These include patient symptoms and anatomical features such as graft age, extent of native/graft vessel disease, distal vessel anatomy, chronic total occlusions, and calcification [3,5]. The lesion profiles of both the patients were characterised by severe multi-vessel disease, proximal calcification, chronic total occlusion, extensive thrombosis, and distal vessel disease proximal to anastomosis. Thus, the decision to treat the native coronary arteries (SVG grafts) using a combined-strategy approach was multifactorial.
Atherosclerotic plaque which manifests within SVG differs morphologically to that of native coronary arteries. Plaque typically found within older venous grafts rapidly accumulates and is distinguishably larger, softer and highly friable with consistency comparable to that of cottage cheese. Furthermore, thinner, more fibrous caps prompt distal embolisation cause the graft to backfill extensively with thrombus [4]. Therefore, glycoprotein 2b/3a inhibitors alone are ineffectual in the prevention of distal embolisation. Embolic Protective Devices (EPD) remain the default therapy to avert such peri-procedural complications, although these devices are not able to trap all debris. Stenting has been shown to provide favourable outcomes in SVG intervention with abundant literature supporting superiority drug-eluting stents over bare-metal stents [6,7]. Lesion pre-dilation versus direct stenting remains a debatable topic and warrants further investigations [3].
It was decided to treat both the patients through a novel pharmaco-invasive approach considering the presentation of three dilemma. The first dilemma encountered during intervention was lack of a distal landing zone impeding distal filter placement. Although the American College of Cardiology/American Heart Association guidelines support adjunctive EPD use [8], several studies have found no outcome benefits of these advanced modern-day devices [9,10]. Therefore, attention should be drawn towards trending deployment of these devices in high-risk patients. Such patients are elderly with several co-morbidities and higher thrombotic burden. Therefore, this trend may have acted as a confounding factor in several earlier studies possibly masking the benefits of EPD use.
The second dilemma encountered was the risk of no-flow phenomenon. The precise cause of the no-flow phenomenon is yet to be established. However, mechanical thrombectomy or aspiration with liberal use of vasodilators is advisable for the prevention as well as treatment of no-reflow [3].
Mortality rates of 14.3% and Major Adverse Cardiac Events (MACE) rates of 36.8% reported in acute myocardial infarction patients are evidence of the risk associated with this patient subset [11]. Significant thrombus burden in the culprit vessel and long lesion length have shown robust correlations with MACE rates [6]. Both the patients presented with long and thrombosed lesions, thus the third dilemma faced was the possibility of MACE.
Conclusion(s)
Venous graft interventions are always challenging. In many cases, filters are preferred to prevent distal embolisation. However, in the setting of ACS accompanied by large thrombotic burden, the use of an EPD is challenging as well as controversial. Here, it is demonstrated that use of thrombolytic agents in judicious dose (intra-lesional) with stenting is feasible even without filter.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 11, 2020
Manual Googling: Apr 03, 2020
iThenticate Software: May 04, 2020 (14%)
[1]. Mathew V, Berger PB, Lennon RJ, Gersh BJ, Holmes DR Jr, Comparison of percutaneous interventions for unstable angina pectoris in patients with and without previous coronary artery bypass graftingAm J Cardiol 2000 86(9):931-37.10.1016/S0002-9149(00)01125-5 [Google Scholar] [CrossRef]
[2]. Harskamp RE, Lopes RD, Baisden CE, de Winter RJ, Alexander JH, Saphenous vein graft failure after coronary artery bypass surgery: Pathophysiology, management, and future directionsAnn Surg 2013 257(5):824-33.10.1097/SLA.0b013e318288c38d23574989 [Google Scholar] [CrossRef] [PubMed]
[3]. Lee M, Kong J, Current state of the art in approaches to saphenous vein graft interventionsInterv Cardiol 2017 12(2):85-91.10.15420/icr.2017:4:2 [Google Scholar] [CrossRef]
[4]. Poon K, Roati A, Walters DL, Saphenous vein graft intervention: Discussion on acute vein graft occlusion interventionJACC Cardiovasc Interv 2011 4(11):1250-51.10.1016/j.jcin.2011.09.00422115669 [Google Scholar] [CrossRef] [PubMed]
[5]. Ota H, Mahmoudi M, Lhermusier T, Magalhaes MA, Torguson R, Satler LF, Comparison of clinical outcomes in patients presenting with an acute coronary syndrome due to stent thrombosis or saphenous vein graft occlusion and undergoing percutaneous coronary interventionCardiovasc Revasc Med 2015 16(8):441-46.10.1016/j.carrev.2015.10.00226704310 [Google Scholar] [CrossRef] [PubMed]
[6]. Mehilli J, Pache J, Abdel-Wahab M, Schulz S, Byrne RA, Tiroch K, Drug-eluting versus bare-metal stents in saphenous vein graft lesions (ISAR-CABG): A randomised controlled superiority trialLancet 2011 378(9796):1071-78.10.1016/S0140-6736(11)61255-5 [Google Scholar] [CrossRef]
[7]. Brilakis ES, Lichtenwalter C, de Lemos JA, Roesle M, Obel O, Haagen D, A randomized controlled trial of a paclitaxel-eluting stent versus a similar bare-metal stent in saphenous vein graft lesions: The SOS (Stenting of Saphenous Vein Grafts) trialJ Am Coll Cardiol 2009 53(11):919-28.10.1016/j.jacc.2008.11.02919281920 [Google Scholar] [CrossRef] [PubMed]
[8]. Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: Executive summary: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and InterventionsJ Am Coll Cardiol 2011 58(24):2550-83.10.1016/j.jacc.2011.08.006 [Google Scholar] [CrossRef]
[9]. Brennan JM, Al-Hejily W, Dai D, Shaw RE, Trilesskaya M, Rao SV, Three-year outcomes associated with embolic protection in saphenous vein graft intervention: Results in 49 325 senior patients in the Medicare-linked National Cardiovascular Data Registry CathPCI RegistryCirc Cardiovasc Interv 2015 8(3):e00140310.1161/CIRCINTERVENTIONS.114.00140325714391 [Google Scholar] [CrossRef] [PubMed]
[10]. Paul TK, Bhatheja S, Panchal HB, Zheng S, Banerjee S, Rao SV, Outcomes of saphenous vein graft intervention with and without embolic protection device: A comprehensive review and meta-analysisCirc Cardiovasc Interv 2017 10(12):e00553810.1161/CIRCINTERVENTIONS.117.00553829246912 [Google Scholar] [CrossRef] [PubMed]
[11]. Gaglia Jr MA, Torguson R, Xue Z, Gonzalez MA, Ben-Dor I, Suddath WO, Outcomes of patients with acute myocardial infarction from a saphenous vein graft culprit undergoing percutaneous coronary interventionCatheter Cardiovasc Interv 2011 78(1):23-29.10.1002/ccd.2287321061247 [Google Scholar] [CrossRef] [PubMed]