Asymptomatic Migration of Intrauterine Device into the Abdominal Cavity
Atef Mejri1, Khaoula Arfaoui2, Emna Trigui3, Badreddine Aloui4
1 Visceral Surgeon, Department of General Surgery, Faculty of Medicine of Tunis, Jendouba, Tunisia.
2 Visceral Surgeon, Department of General Surgery, Faculty of Medicine of Tunis, Jendouba, Tunisia.
3 Obstetric-Gynecologist Surgeon, Department of Obstetrics and Gynaecology, Faculty of Medicine of Tunis, Jendouba, Tunisia.
4 Visceral Surgeon, Department of General Surgery, Faculty of Medicine of Tunis, Jendouba, Tunisia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Atef Mejri, BP 294, Bousalem, Jendouba, Tunisia.
E-mail: atef.mejri@hotmail.com
The Intrauterine Device (IUD) is one of the most used and effective contraceptive means worldwide due to its anti-conceptual and anti-nesting action. Although IUD use offers the benefits of being affordable, long lasting, highly effective, and reversible. However, like any foreign body, it can expose to certain complications, sometimes, with very serious consequences. Migration is the rarest but most feared complication. The frequency of uterine perforation ranges from 0.05 to 13 per 1000 insertions. It can be announced by pelvic pain, and in the majority of cases reported; this accident does not lead to major complications and remains clinically silent. The clinical presentation varies depending on the final ectopic site of the device. We report the case of an IUD migration into the peritoneal cavity 10 years after its insertion in a 41-year-old patient whose only complaint was epigastric pain. The clinical examination did not reveal lower abdominal tenderness. Apart from a lipase rate, which was around ten times the normal level, other ordinary blood tests did not show any abnormalities. The diagnosis was made fortuitously based on the subsequent CT scan findings that were part of the routine staging of the acute lithiasic pancreatitis, the underlying cause of the described pain. Acute pancreatitis was staged B and the patient had a successful surgical retrieval of the IUD with a good outcome.
Complication, Laparoscopy, Uterine perforation
Case Report
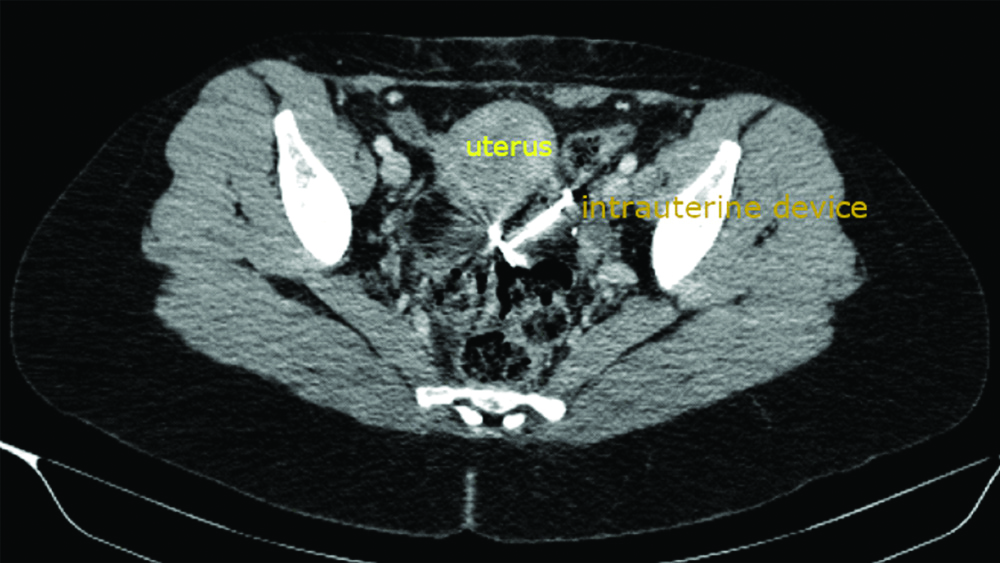
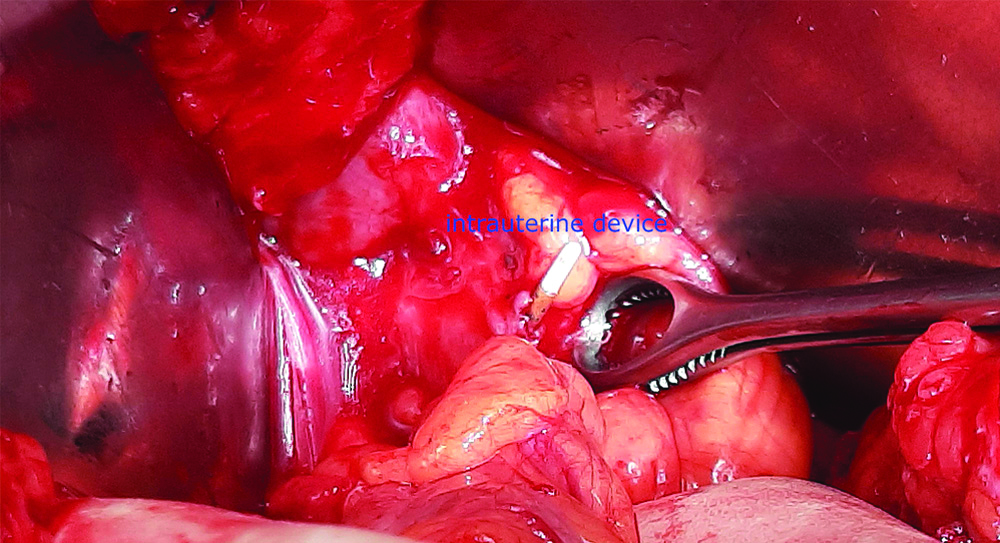
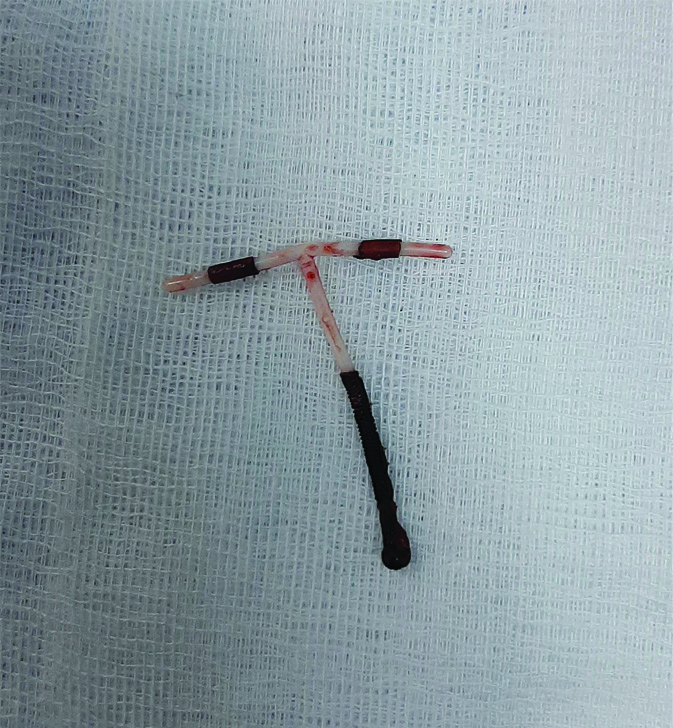
A 41-year-old patient presented to the surgery outpatient clinic for a severe transfixiant stabbing epigastric pain evolving for 48 hours that did not respond to usual pain relievers. She was Gravidia 5, Para 3 and had three Caesarean sections by Pfannenstiel incision, the last one dates back to 12 years. She carried an IUD for 10 years, and she claimed it had expelled spontaneously 3 years after its installation. She had a spontaneous miscarriage five years ago for which she did not consult a gynaecologist. She had no other notable medical or surgical past history and had no history of lower abdominal pain. On clinical examination, she was apyrexial and haemodynamically stable, the abdomen was soft with a slight epigastric tenderness. Blood tests did not showed any abnormalities besides a lipasemia at 10xN confirming the diagnosis of acute pancreatitis and pregnancy test was negative. An abdomino-pelvic CT scan was performed 48 hours later for a pancreatitis staging which showed an enlargement of the pancreas with no inflammatory changes in the peripanceatic fat or any collections thus making the diagnosis of grade B acute Pancreatitis. It also showed an ectopic IUD in the posterior cul-de-sac with no signs of further complications [Table/Fig-1]. Patient underwent a laparoscopic surgery. The exploration found an adherential pelvis with a perforation of the uterus, posterior wall thus exposing part of the IUD intra abdominally [Table/Fig-2]. Attempts at careful laparoscopic extraction failed due to the presence of an adherent magma. The resumption of the old pfannenstiel type scar made it possible to remove the IUD [Table/Fig-3] and the postoperative period was uneventful. The patient was discharged from the hospital in a stable condition five days after the removal of the IUD and at the follow-up visits, she was fully recovered.
A CT scan axial view showing an IUD in the peritoneal cavity.
Intraoperative view showing an adherential pelvis with a perforation of the uterus, posterior wall exposing IUD intra abdominally.
Discussion
The IUD is an old contraceptive method, used for first time in 1909 by Richard Richter in Germany and remains very widespread in the world because of its good tolerance and its long duration of action [1]. Although it protects against systemic side effects of hormonal methods but it is not completely harmless and migration remains a rare complication not exceeding 3 per 1000 but potentially serious [2]. This obstacle seems to be linked with the type of device (higher rates occur with copper-containing IUDs), timing of insertion (higher rates occur in lactating women), ability of the operator to perform the procedure, location of the uterus (higher rates occur in retroverted uteri), and level of follow-up [2,3]. Multiparity and previous scars in the uterus these two conditions retained in present case patient. Migration can be suspected sometimes by the occurrence of intense pelvic pain but in present case it likely went completely unnoticed. This closely corresponds and correlates to the findings in the literature stating that 85% of reported IUD migration cases did not involve significant signs of complications at the time of the diagnosis [2]. In this case, we bring to light a serious error often made by some health care workers in the IUD management. Failure to locate the IUD strings always suggest the possibility of migration and justifies the need for further investigations in order to rule out this presumption before assuming its expulsion. In this reported case, the absence of visualisation of the reference wires during the clinical examinations was hastily and wrongly attributed to the simple spontaneous expulsion of the device. Indeed, the radiography eliminates the erroneous conclusions of a spontaneous expulsion and confirms the migration of the IUD especially if the latter has completely crossed the uterine wall by showing a metallic opacity in the shape of a T in an ectopic abdominal position without judging its topography exactly [4].
However, CT imaging is of great value as it indicates precise IUD positioning, gives further evaluation of adjacent anatomy, and it plays a key role in detecting and evaluating associated intra abdominal complications such as abscess, bowel obstruction or even perforation [5]. Therefore, a precise localisation of this foreign body, its relation with organs and its possible vascular contacts by an abdominal CT is judicious before considering any gesture of surgical extraction [6]. Once in an ectopic position, the IUD can be embedded anywhere in the peritoneal cavity, though it seems to have a predilection for the Douglas pouch, the broad ligament and the omentum but other rare and surprising locations have been reported in the literature [7]. Haouas N et al., presented two cases of intra vesical migration of IUDs with lithiasis formation treated by cystoscopy [8], Delotte J et al., published the case of an intra rectal migration of IUDs which was the subject of anoscopic extraction [9] as well as appendicular perforation by an IUD has been reported by Cuillier F et al., [7]. Other complications such as acute bowel obstruction on the bridle or following intestinal strangulation by the IUD thread or peritonitis by perforation of a hollow organ are rare but more serious and should be kept in mind [10]. In previous times ectopic IUDs were not removed in case of asymptomatic patients; but today, most of the experts recommend removal of any ectopic IUD [11]. It is currently recognised that the immediate removal of any diagnosed migrating IUD is necessary to avoid these complications [12]. Early surgical intervention is also highly recommended in order to decrease the adhesion formation. Laparoscopy is the best surgical option, since it allows good exploration of the entire peritoneal cavity only through small trocar incisions, and it succeeds in finding and removing the IUD in 44-100% of cases [13].
However, the adhesions generated by the inflammatory reaction induced by copper IUDs sometimes makes dissection difficult and the extraction hazardous [7]. In this case, we did not hesitate to convert in order to avoid lesions of digestive perforations that are sometimes overlooked during the operation. Given the aesthetic damage involved in such an approach the patient was warned before the intervention of the risk of laparo-conversion and prior consent was granted.
Conclusion(s)
Intraperitoneal migration of the IUD is a rare accidental event that can remain asymptomatic and therefore remains undiagnosed for a long time, but it is not risk free. This justifies a systematic surgical treatment ideally by laparoscopy and must above all encourage the adoption of a regular clinical and paraclinical monitoring of each patient carrying this contraceptive method in order to watch for this complication in time.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 05, 2020
Manual Googling: Apr 17, 2020
iThenticate Software: May 04, 2020 (11%)
[1]. Nowitzki KM, Hoimes ML, Chen B, Zheng LZ, Kim YH, Ultrasonography of intrauterine devicesUltrasonography 2015 34(3):183-94.10.14366/usg.1501025985959 [Google Scholar] [CrossRef] [PubMed]
[2]. Bouzouba W, Alaoui F, Jayi S, Bouguern H, Melhouf M, Intraperitoneal migration of intrauterine device diagnosed 20 years after insertion: Report of a caseThe Pan African Medical Journal 2014 17:710.11604/pamj.2014.17.7.379025184024 [Google Scholar] [CrossRef] [PubMed]
[3]. Zakin D, Stern WZ, Rosenblatt R, Complete and partial uterine perforation and embedding following insertion of intrauterine devices. II. Diagnostic methods, prevention, and managementObstet Gynaecol Surv 1981 36(8):401-17.10.1097/00006254-198108000-000016455610 [Google Scholar] [CrossRef] [PubMed]
[4]. Chai W, Zhang W, Jia G, Cui M, Cui L, Vesical transmigration of an intrauterine contraceptive device: A rare case report and literature reviewMedicine 2017 96(40):e823610.1097/MD.000000000000823628984781 [Google Scholar] [CrossRef] [PubMed]
[5]. Boortz HE, Margolis DJA, Ragavendra N, Patel MK, Kadell BM, Migration of intrauterine devices: Radiologic findings and implications for patient careRadioGraphics 2012 32(2):335-52.10.1148/rg.32211506822411936 [Google Scholar] [CrossRef] [PubMed]
[6]. Brar R, Doddi S, Ramasamy A, Sinha P, A forgotten migrated intrauterine contraceptive device is not always innocent: A case reportCase Rep Med 2010 2010:7406422010 [cité 13 avr 2020];2010. Disponible sur: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2938829/10.1155/2010/74064220862381 [Google Scholar] [CrossRef] [PubMed]
[7]. Cuillier F, Ghalem S, Haffaf Y, Intrauterine device appendicitis: An exceptional complicationJournal de Gynécologie, Obstétrique Et Biologie De La Reproduction 2003 32:55-57. [Google Scholar]
[8]. Haouas N, Sahraoui W, Youssef A, Intravesical migration of intrauterine device resulting in stone formationJ Gynecol Obstet Biol Reprod (Paris) 2006 35(3):288-92.10.1016/S0368-2315(06)78316-8 [Google Scholar] [CrossRef]
[9]. Delotte J, Trastour C, Bafghi A, Iannelli A, Bongain A, A surprising reason for consulting: wires projecting from the anus, a rare complication of intra uterine device insertionJ Gynaecol Obstet Biol Reprod (Paris) 2006 35(8 Pt 1):820-21.10.1016/S0368-2315(06)76485-7 [Google Scholar] [CrossRef]
[10]. Yang HW, Zhou ZG, Small bowel obstruction caused by migrated intrauterine contraceptive device: A case reportBiomedical Research [Internet] 2017 [cité 13 avr 2020] 28(22):10125-27.Disponible sur: https://www.alliedacademies.org/abstract/small-bowel-obstruction-caused-by-migrated-intrauterine-contraceptive-device-a-case-report-9472.html [Google Scholar]
[11]. Ozgun MT, Batukan C, Serin IS, Ozcelik B, Basbug M, Dolanbay M, Surgical management of intra-abdominal mislocated intrauterine devicesContraception 2007 75(2):96-100.10.1016/j.contraception.2006.09.01117241837 [Google Scholar] [CrossRef] [PubMed]
[12]. Shah B, Degloorkar S, Intrauterine contraceptive device in peritoneal cavity invading sigmoid colonJournal of Case Reports 2015 4(1):193-95.10.17659/01.2014.0048 [Google Scholar] [CrossRef]
[13]. Lachiri B, Hafidi MR, Zazi A, Fagouri H, Kouach J, Rahali DM, Migratory IUD: Report of two cases and review of the literaturePan Afr Med J 2014 19:361 [Google Scholar]