Actinomyces turicensis causing Urinary Tract Infection in Nephrotic Syndrome Patient- A Case Report
D Sarumathi1, Pallam Gopichand2, Kapil Sejpal3, PS Priyamvada4, Jharna Mandal5
1 Junior Resident, Department of Microbiology, Jawaharlal Institute of Postgraduate Medical Education & Research, Puducherry, India.
2 Senior Resident, Department of Microbiology, Jawaharlal Institute of Postgraduate Medical Education & Research, Puducherry, India.
3 Senior Resident, Department of Nephrology, Jawaharlal Institute of Postgraduate Medical Education & Research, Puducherry, India.
4 Associate Professor, Department of Nephrology, Jawaharlal Institute of Postgraduate Medical Education & Research, Puducherry, India.
5 Additional Professor and Head, Department of Microbiology, Jawaharlal Institute of Postgraduate Medical Education & Research, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jharna Mandal, Additional Professor and Head, Department of Microbiology, Jawaharlal Institute of Postgraduate Medical Education & Research, Puducherry, India.
E-mail: drjharna@gmail.com
Urinary Tract Infections (UTI) are one of the most common bacterial infections which accounts for significant cost to health care and it is one of the important cause of bacteremia. Escherichia coli remain the most common causative agent followed by Klebsiella pneumoniae, Proteus mirabilis and Enterococcus species. Actinomyces turicensis (A. turicensis) belongs to the family Actinomycetaceae. It is a rare pathogen and an infrequent cause of UTI. The author highlights one such case of a 42-year-old male with history of Nephrotic Syndrome (NS) presented with complaints of fever, dysuria and loose stools for three days. He was on treatment with corticosteroids for a long time. A. turicensis was isolated from urine of this patient as a single pathogen on culture and was found to be sensitive to Ampicillin, Ciprofloxacin, Cotrimoxazole and Nitrofurantoin. The patient responded well to Metronidazole and ampicillin and was discharged. The pathogenic importance of this organism cannot be undermined and should not be ignored in such cases who are on corticosteroids or any immunosuppressive drugs.
Actinomycetaceae, Bacteremia, Kidney disorder
Case Report
A 42-year-old non-diabetic male who was otherwise a known case of NS presented with complaints of fever, dysuria and loose stools for three days. He was on treatment with corticosteroids for one and half years to manage his underlying NS and similar history in family was not present. On examination, he was febrile, but no pain abdomen or renal angle tenderness could be elicited. His physical examination revealed no abnormalities. On investigation, his blood culture was sterile and stool sample did not reveal any pathogen on culture. Other laboratory investigations showed that the patient was anaemic [Table/Fig-1]. The consent form was obtained from the patient for his clinical information to be published.
Laboratory investigations.
| Investigation | Value | Normal range |
|---|
| Urine analysis |
| Glucose | Present (2+) | Absent |
| Protein | Present (2+) | Absent |
| Cast | Granular cast (3+) | Absent |
| WBC | 5-10/HPF | 0-1/HPF |
| Crystal | Absent | Absent |
| Interpretation: Presence of glycosuria, Protenuria and Pyuria suggests the presence of renal abnormalities |
| Haemogram |
| Haemoglobin | 10.1 gm% | 13.2-17.3 gm% |
| RBC count | 3.81×106/μL | 4.3-5.7×106/μL |
| Haematocrit | 31.7% | 38-50% |
| Platelets | 173×103/μL | 150-450×103/μL |
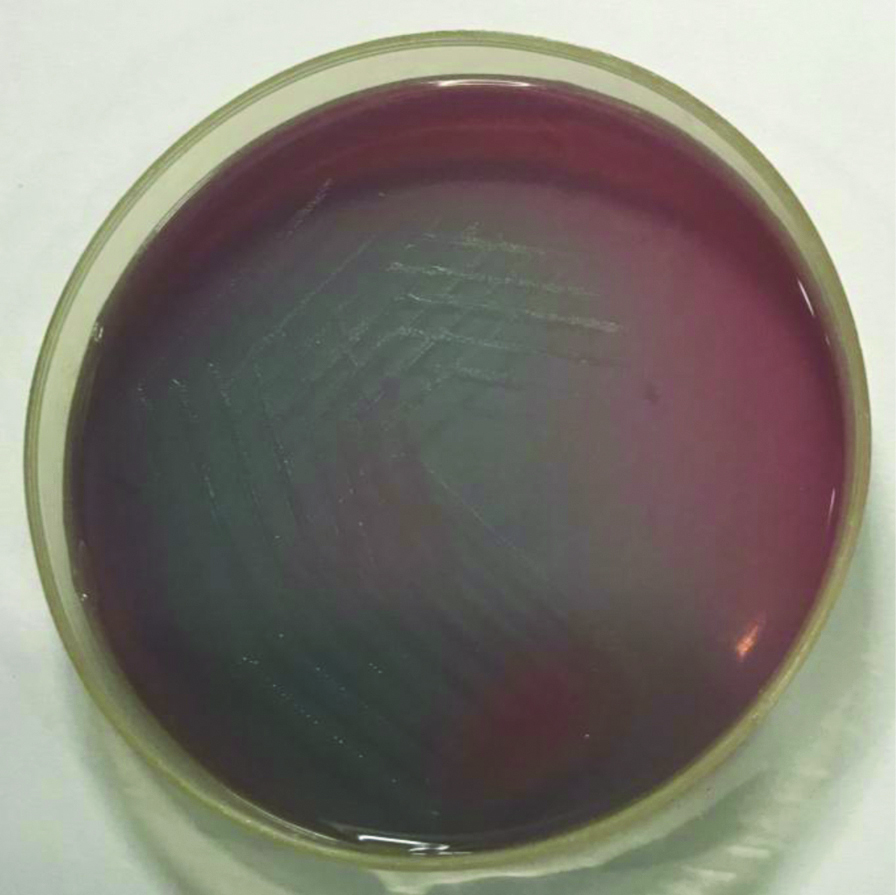
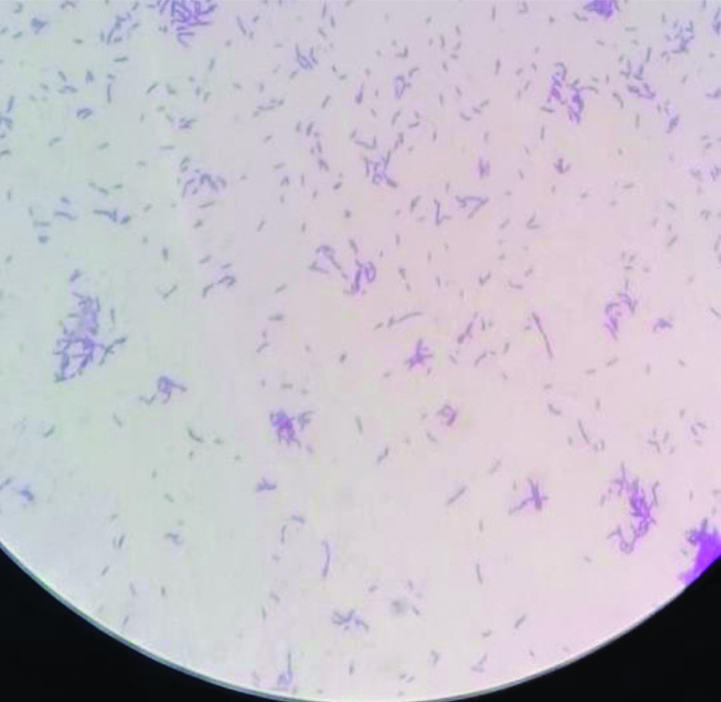
Mid-stream clean catch urine sample was sent to Microbiology laboratory for culture. Grossly, the urine was turbid. Microscopic examination revealed the presence of pus cells without any RBC and epithelial cells. Using the standard semi-quantitative method [1], the sample was inoculated onto Cysteine-Lactose-Electrolyte Deficient (CLED) agar and 5% sheep blood agar. After 18-24 hours of incubation at 37°C aerobically, very minute pale colonies were seen on the CLED agar [Table/Fig-2], while on the blood agar, small grey, convex circular non-haemolytic colonies were observed with a colony count of >104 CFU/mL [Table/Fig-3]. Both catalase and oxidase tests were negative. Gram stain showed short thin branching curved Gram positive rods [Table/Fig-4] which were non-acid fast, non-motile, did not hydrolyse aesculin, did not hydrolyse urea and was negative in the CAMP test (Christie-Atkins-Munch-Peterson). The colonies were subjected to MALDI-TOF-MS (version 3.2, Biomerieux, France) and it was identified as Actinomyces turicensis. As per the Clinical Laboratory Standards Institute (CLSI) recommended method [2], antimicrobial susceptibility testing was performed and the strain was found to be sensitive to Ampicillin, Ciprofloxacin, Cotrimoxazole and Nitrofurantoin.
CLED agar showing colonies of Actinomyces turicensis.
A 5% sheep blood agar plate showing colonies of Actinomyces turicensis.

Gram stain done from culture.
The patient was started on Metronidazole 400 mg/PO thrice daily and Ampicillin 500 mg/PO every 8 hourly and responded well. He was discharged on the same antimicrobials after two days of stay in the hospital. After seven days of therapy, the urine sample was submitted for culture which was found to be sterile.
Discussion
Actinomycosis is an indolent chronic bacterial infection caused by gram positive filamentous bacteria which belongs to the family, Actinomycetaceae. It contains species which can withstand anaerobic to microaerophilic conditions of growth. Actinomyces israeli has long been considered as causative organism for actinomycosis. The availability of advanced automated bacterial identification system and molecular methods, many species of Actinomyces has been identified with ease from various clinical specimens [3-5]. In this regard, A. turicensis is emerging as an important cause of infection at many body sites. This report discusses the presentation and diagnosis of one such case with a rare association of UTI caused by A. turicensis. Actinomyces genus consists of organism which is obligate anaerobe as well as aerotolerant. They are Gram positive branching rods which on serial subcultures tend to appear coccobacilli which are arranged singly or in pairs, are non-acid fast bacilli and non-motile [6]. There are many species which have been identified till now some of which are pathogenic to man. The most common species is A. israelii [3,7].
Actinomyces turicensis was first reported in 1995 by Wust J et al., [6]. Since then it has been found to be associated with infections in various sites such as genital, UTI and skin infection [8]. In a study by Hall V et al., A. turicensis was isolated in 18.5% (80/432 strains) of the clinical cases of actinomycosis studied [4]. The most common clinical presentation was penile lesion followed by rectal abscess. According to another study by Clarridge JE and Zhang Q detected A.turicensis in urine and urethral exudate samples from 9 patients out of 23 cases [9]. In another study done by Sabbe LJ et al., A.turicensis was isolated from six patients with urethritis and cystitis and reported as the sole organism in three male patients [10]. The study also showed that in both males and females, A.turicensis was detected in connection with urethritis and cystitis. In a case report by Kansara T et al., this organism was found to be associated with renal stones and life threatening sepsis [11]. According to Vandamme P et al., most strains of A.turicensis which were isolated from various specimens were susceptible to antibiotics such as Penicillin, Oxacillin, Erythromycin, Cefazolin, and Cotrimoxazole [12]. In the present case, A. turicensis isolated from urine was found to be sensitive to Ciprofloxacin, Ampicillin and Nitrofurantoin, Cotrimaxazole. The patient was started on Metronidazole and Ampicillin after two days of sending urine culture. Urine sample after seven days was found to be sterile on culture.
Conclusion(s)
This case report highlights the importance of lesser-known agents of UTI and the importance of A. turicensis which cannot be overemphasised, considering the underlying condition of the present case. The identification of this pathogen by rapid diagnostics is need of the hour, which aids in early treatment of the rare organism.
Authors and contributors: SD, GP performed the experiments/tests and drafted the manuscript. SKN, PPS were involved in the clinical management of the patient. PPS added to the clinical data in the manuscript. JM supervised and interpreted the test results and finally edited the manuscript.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. No
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 03, 2020
Manual Googling: Apr 23, 2020
iThenticate Software: May 04, 2020 (13%)
[1]. Mackie TJ, Mackie & McCartney Practical Medical Microbiology 2006 14th editionNew YorkChurchill Livingstone [Google Scholar]
[2]. CLSI. Methods for Antimicrobial Dilution and Disk Susceptibility Testing of Infrequently Isolated or Fastidious Bacteria. 3rd ed. CLSI guideline M45. Wayne, PA: Clinical and Laboratory Standards Institute; 2015 [Google Scholar]
[3]. Schaal KP, Lee HJ, Actinomycete infections in humans- A reviewGene 1992 115(1-2):201-11.10.1016/0378-1119(92)90560-C [Google Scholar] [CrossRef]
[4]. Hall V, Talbot PR, Stubbs SL, Duerden BI, Identification of clinical isolates of Actinomyces species by amplified 16S ribosomal DNA restriction analysisJournal of Clinical Microbiology 2001 39(10):3555-62.10.1128/JCM.39.10.3555-3562.200111574572 [Google Scholar] [CrossRef] [PubMed]
[5]. Le Bihan A, Ahmed F, O’Driscoll J, An uncommon cause for a breast abscess: Actinomyces turicensis with Peptoniphilus hareiBMJ Case Reports CP 2019 12(12):pii: e23119410.1136/bcr-2019-23119431796455 [Google Scholar] [CrossRef] [PubMed]
[6]. Wust J, Stubbs S, Weiss N, Funke G, Collins M, Assignment of Actinomyces pyogenes-like (CDC coryneform group E) bacteria to the genus Actinomyces as Actinomyces radingae sp. nov. and Actinomyces turicensis sp. NovLett Appl Microbiol 1995 20:76-81.10.1111/j.1472-765X.1995.tb01290.x7534464 [Google Scholar] [CrossRef] [PubMed]
[7]. Könönen E, Wade WG, Actinomyces and related organisms in human infectionsClin Microbiol Rev 2015 28(2):419-42.10.1128/CMR.00100-1425788515 [Google Scholar] [CrossRef] [PubMed]
[8]. Chudáčková E, Geigerová L, Hrabák J, Bergerová T, Liška V, Scharfen J, Seven isolates of Actinomyces turicensis from patients with surgical infections of the anogenital area in a Czech hospitalJournal of Clinical Microbiology 2010 48(7):2660-61.10.1128/JCM.00548-1020504980 [Google Scholar] [CrossRef] [PubMed]
[9]. Clarridge JE, Zhang Q, Genotypic diversity of clinical Actinomyces species: Phenotype, source, and disease correlation among genospeciesJ Clin Microbiol 2002 40:3442-48.10.1128/JCM.40.9.3442-3448.200212202591 [Google Scholar] [CrossRef] [PubMed]
[10]. Sabbe LJ, Van De Merwe D, Schouls L, Bergmans A, Vaneechoutte M, Vandamme P, Clinical spectrum of infections due to the newly described Actinomyces species A. turicensis, A. radingae, and A. europaeusJ Clin Microbiol 1999 37:08-13.10.1128/JCM.37.1.8-13.1999 [Google Scholar] [CrossRef]
[11]. Kansara T, Majmundar M, Doshi R, Ghosh K, Saeed M, A case of life-threatening Actinomyces turicensis bacteremiaCureus 2020 12(1):e676110.7759/cureus.676132140329 [Google Scholar] [CrossRef] [PubMed]
[12]. Vandamme P, Falsen E, Vancanneyt M, Van Esbroeck M, Van de Merwe D, Bergmans A, Characterization of Actinomyces turicensis and Actinomyces radingae strains from human clinical samplesInt J Syst Bact 1998 48:503-10.10.1099/00207713-48-2-5039731291 [Google Scholar] [CrossRef] [PubMed]