Introduction
Acrylic resin is the most common material used for the prosthodontic and orthodontic removable appliances. Many brands have come up with High impact resins to overcome its inherent drawbacks of relatively poor resistance to impact and flexural forces, which might affect lifespan of the denture. Now-a-days, use of the high impact denture base materials is very common and hence, clinicians should be aware of the properties of high impact denture base materials available in market.
Aim
To evaluate and compare the impact strength and flexural strength of different brands of high impact denture base materials.
Materials and Methods
The present study was a comparative in-vitro study carried out in Krishna Institute of Medical Sciences Deemed to be University, Karad, Maharashtra, India from January 2017 to August 2017. Three high impact denture base materials used in the study were TRIPLEX (Ivoclar, Vivadent, Liechtenstin), LUCITONE 199 (Dentsply International Inc. Degu Dent GmbH Hanau, Germany) and DENTEK (SP Dental, India). Flexural and impact strengths of these three brands of high impact denture base materials were evaluated and analysed statistically using One-way analysis of variance (ANOVA) test with the help of SPSS version 21.0© software (IBM Corporation, Armonk, NY, USA).
Results
The mean impact strength values of three groups showed that Group III (DENTEK) (8.45 KJ/mm2) had the highest mean impact strength value followed by Group I (TRIPLEX), (8.19 KJ/mm2) and Group II (LUCITONE 199) (5.43 KJ/mm2). The difference between Groups III and I was insignificant but the difference was significant between Group III and Group II as well as between Group I and Group II. Group II showed highest mean flexural strength (103.45 Mpa) followed by Group I (95.95 Mpa) and Group III (86.22 Mpa). But difference was statistically insignificant among the three groups for flexural strength.
Conclusion
The study concluded that highest impact strength recorded was with DENTEK followed by TRIPLEX and LUCITONE. The highest flexural strength recorded was with LUCITONE followed by TRIPLEX and DENTEK.
Acrylic reinforcement, Denture fracture, Polymethylmethacrylate, Torsional forces
Introduction
Dentures are prosthetic devices used to replace the missing teeth which take support from surrounding hard and soft tissues of the oral cavity. In ancient times, dentures were made up of ivory, animal horns, bone or wood [1,2]. Vulcanised rubbers came in use as a denture base material in 18th century [3]. Acrylic resin was developed in 1937 by Dr. Walter Wright during the early years of the Second World War when the use of natural rubber for dental vulcanite was prohibited [4,5]. An ideal denture base material should possess several properties such as biocompatibility, ease of repair, high bond strength with teeth, good esthetics and adequate physical and mechanical properties [6,7]. No such material has been introduced till today, which possesses all the above mentioned properties and the research continued to prosper in the respective field.
Even after 80 years of its invention, acrylic resins are the most common material used for the prosthodontic and orthodontic removable appliances [2]. Acrylic resin is basically derived from acrylic acid, methacrylic acid or compounds related to them. Most commonly used acrylic resin is Poly Methyl Methacrylate (PMMA) [6,7]. Adequate strength, excellent esthetic properties, low water sorption, biocompatibility, facility of repair, and simple processing technique are some of the advantages of PMMA material [8,9]. At the same time the material has some inherent drawbacks as relatively poor resistance to impact and flexural forces which might affect lifespan of the denture [10-13]. Denture fractures are very common and pose a problem for patient, dentists as well as the laboratory technicians. Denture fractures usually result from two types of forces as flexural fatigue and impact force. Flexural fatigue is responsible for the midline fracture while denture fracture because of the sudden fall of the denture is a result of impact failure [11]. Denture fracture also may be due to a multiplicity of factors rather than just denture base material properties itself as thin denture base, prominent frenum-usually labial, prominent midpalatine raphe, single complete denture opposing natural dentition without any reinforcement etc., [14-19]. Midline fracture is the most common site of denture fracture which usually coincides with the notch for the relief of labial frenum of either the maxillary and mandibular complete denture (59%) [15-17,20]. Denture fracture thus shows that adequate flexural strength and impact strength are a common requisite to overcome these fractures.
Flexural strength is the stress in a material just before it yields in a flexure test [6,21]. High flexural strength of the material resists the torsional forces in function for the longer clinical service of the prosthesis, while Impact strength is the measure of the energy absorbed by a material when it is subjected to sudden load [22]. Thus, flexural strength indicates material performance under the conditions of static load while impact strength is a measure of energy absorbed by the material before fracture [23,24].
Literature suggests two approaches to strengthen PMMA material [12,25,26]. One is to increase the impact strength by incorporating a rubber phase in bead polymer [12,25]. Rodford RA described the development of these high impact denture base materials using Butadiene-styrene rubber [27]. The Butadiene-styrene rubber particles help to achieve better bond with PMMA. These high impact denture base materials are so-called because of greater impact strength and fatigue properties. The second approach is a reinforcement of PMMA resin denture base with high modulus fibres, for example, carbon fibers, glass fibers, ultra-high modulus polyethylene, titanium derived fillers, silver nanoparticles, zirconium oxide nanoparticles etc., [25-31].
Many brands of acrylic resins are available as “High impact resins”. There have been many studies comparing regular heat cure resins but very few studies are available comparing high impact resins. At present, use of high impact denture base materials is very common and hence clinicians should be aware of the properties of high impact denture base materials for selection of better material from the different available brands. So, the purpose of this study was to evaluate and compare the flexural and impact strength of three different brands of high impact denture base resins.
Materials and Methods
This was a comparative in-vitro original research study. The study was carried out in the Department of Prosthodontics, School of Dental Sciences, Krishna Institute of Medical Sciences Deemed to be University (KIMSDU), Karad, Maharashtra, India during January 2017 -August 2017. The approval from the KIMSDU ethical committee (Protocol no. 2016-17/228 and letter no. KIMSDU/IEC/04/2016) was obtained. The materials selected for the study based upon fact that these were the commonly used materials in the western Maharashtra region and sufficient scientific literature was not available regarding their comparative mechanical properties.
Three high impact denture base materials used in the study were:
Group I: High Impact heat cure PMMA-TRIPLEX (Ivoclar, Vivadent, Liechtenstin)
Group II: High Impact heat cure PMMA-LUCITONE 199 (Dentsply International Inc. Degu Dent GmbH Hanau, Germany)
Group III: High Impact heat cure PMMA-DENTEK (SP Dental, India).
Three Stainless steel dies of dimensions 64 × 10 × 3 mm each as per the ISO standardisation (ISO: 1567:1999) required for testing flexural strength of denture base acrylic resin (10 in each group) were fabricated. Similarly, another three Stainless steel dies of dimensions 60×8×3 mm each as per the ISO standardisation (ISO: 1567:1999) required for testing impact strength of denture base acrylic resin (10 in each group) were fabricated.
Preparation of the Mould
A. For impact strength: Three Metal dies of dimension 60×8×3 mm each (ISO: 1567:1999) were flasked (Jabbar Varsity Flask. India) using standard flasking protocols with Type III Dental stone (Kalstone, Kalabhai, India). After the stone was set, the metal dies were removed thus creating space for the resin [Table/Fig-1].

B. For flexural strength: In a similar way, moulds were prepared for the impact strength samples with the use of metal dies of dimension 64×10×3 mm each (ISO: 1567:1999).
Preparation of the Acrylic Specimens
The monomer-polymer ratio was maintained as per the manufactures’ instructions for all three resin brands. The monomer-polymer ratio for Triplex resin was 1:2.3 while it was 1:2.1 for Lucitone 199 and 1:2.5 for Dentek. After packing, the flasks were allowed to bench cure for 1 hour under hydraulic press (Sirio P400, SIRIO DENTAL S.R.L. Meldola, Italy) at pressure and then transferred on manual press [7]. The acrylic specimens were cured with long curing cycle in a digitally controlled acryliser (Wasserman 170980, Hamburg, Germany). The acrylic specimens were retrieved after deflasking followed by their finishing and polishing [Table/Fig-2]. The polished specimens were measured using a digital vernier calliper (Aerospace 0-150 digital calliper pr17, India). This procedure was repeated until there were 10 specimens of the 3 brands each thus making 30 specimens available for flexural strength testing and 30 specimens for impact strength testing. The specimens then stored in 3 different water baths (20 specimens in each bath) according to the brand to avoid the mix up [Table/Fig-3]. The specimens were stored in a water bath for 24 hour so that the residual monomer from acrylic specimens could leach out.
Samples: a) Impact strength Samples; b) Flexural strength Samples.
Final division of the specimens.
Evaluation of Impact Strength
Impact strength of the samples was determined using the Izod/Charpy Impact testing machine (Computerised, Software based), Company: International Equipments, India, Serial No. 430. Impact strength is the measure of the energy absorbed by a material when it is subjected to sudden load [14-17]. Impact strength is calculated by using the formula:
Impact Strength=(Impact Energy)/(Area of the Sample)
Evaluation of Flexural Strength
Universal testing machine {(Computerised, software based) Company: Star Testing System, India. Model No. STS 248} was used to determine the flexural strength of the samples. Accuracy of the machine: ±1%, C/h speed: 5mm/minutes, Distance between supports: 50mm. The maximum load before fracture was recorded for all the specimens with the help of Universal testing machine. To calculate the flexural strength, following formula was used:
FS=3FL/2bd2 [32] where,
FS=Flexural strength
F=the force at fracture point (N) L=the length
b=width, d=thickness.
Statistical Analysis
Mean value along with the standard deviation for the three groups was calculated for both impact and flexural strength records. One-way analysis of variance (ANOVA) was used to statistically compare the study groups using SPSS version 21.0© software (IBM Corporation, Armonk, NY, USA).
Results
Impact and flexural strengths were measured for three different commercially available high impact heat cure PMMA. The results were as follows.
Impact Strength
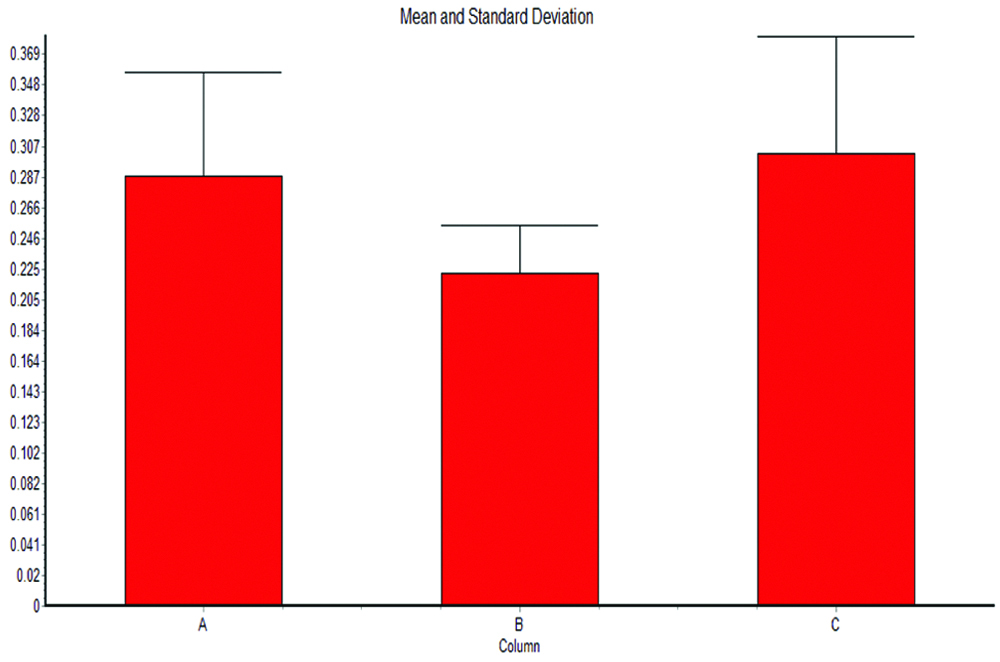
Energy absorbed to break the specimens of Group I ranged from 0.18 J to 0.40 J with a mean of 0.287 J. For Group II it was from 0.16 J to 0.28 J with a mean of 0.222 J and for Group III from 0.20 J to 0.46 J with a mean of 0.30 J.
Impact strength ranges from 5.14 KJ/m2 to 11.42 KJ/mm2 with a mean of 8.195 KJ/mm2 for Group I. For Group II and Group III the mean Impact strength was 5.439 KJ/mm2 and 8.45 KJ/mm2, respectively [Table/Fig-4,5].
Comparative statistics of Impact strength.
| Group A: Triplex | Group B: Lucitone | Group C: Dentek |
|---|
| Sample No. | Impact energy (J) | Izod impact strength (KJ/m2) | Sample No. | Impact energy (J) | Izod impact strength (KJ/m2) | Sample No. | Impact energy (J) | Izod impact strength (KJ/m2) |
|---|
| No. 1 | 0.26 | 7.42 | No. 1 | 0.28 | 6.86 | No. 1 | 0.28 | 7.84 |
| No. 2 | 0.30 | 8.57 | No. 2 | 0.22 | 5.39 | No. 2 | 0.36 | 10.08 |
| No. 3 | 0.24 | 6.85 | No. 3 | 0.20 | 4.90 | No. 3 | 0.46 | 12.88 |
| No. 4 | 0.32 | 9.14 | No. 4 | 0.24 | 5.88 | No. 4 | 0.20 | 5.60 |
| No. 5 | 0.24 | 6.85 | No. 5 | 0.20 | 4.90 | No. 5 | 0.28 | 7.84 |
| No. 6 | 0.32 | 9.14 | No. 6 | 0.22 | 5.39 | No. 6 | 0.22 | 6.16 |
| No. 7 | 0.40 | 11.42 | No. 7 | 0.22 | 5.39 | No. 7 | 0.34 | 9.52 |
| No. 8 | 0.38 | 10.85 | No. 8 | 0.24 | 5.88 | No. 8 | 0.28 | 7.84 |
| No. 9 | 0.18 | 5.14 | No. 9 | 0.16 | 3.92 | No. 9 | 0.36 | 10.08 |
| No. 10 | 0.23 | 6.57 | No. 10 | 0.24 | 5.88 | No. 10 | 0.24 | 6.72 |
| Average | 0.287 | 8.195 | | 0.222 | 5.439 | | 0.30 | 8.45 |
Mean Impact strength of three study groups.
| Group | No. of points | Mean | Standard deviation | Standard error of mean | Median |
|---|
| 1 | 10 | 8.195 | 1.988 | 0.6287 | 7.995 |
| 2 | 10 | 5.439 | 0.7816 | 0.2472 | 5.390 |
| 3 | 10 | 8.456 | 2.200 | 0.6957 | 7.840 |
The comparative statistics of Impact strength showed in [Table/Fig-4]. The mean impact strength values of three groups [Table/Fig-5] showed that Group III had the highest mean impact strength value followed by Group I and Group II. Also the comparison showed that the difference between Group II and Group III (p=0.002) and that of between Group I and Group II (p=0.005) was statistically significant. However, the difference between Groups I and III was insignificant [Table/Fig-6]. So Group III can be considered the most superior among the three groups in terms of impact strength.
One-way ANOVA- impact strength.
| | Mean difference | p-value | F-value |
|---|
| Triplex | Lucitone | 2.75 | 0.005* | 8.915 |
| Dentek | -0.26 | 0.942 |
| Lucitone | Dentek | -3.017 | 0.002* |
Flexural Strength
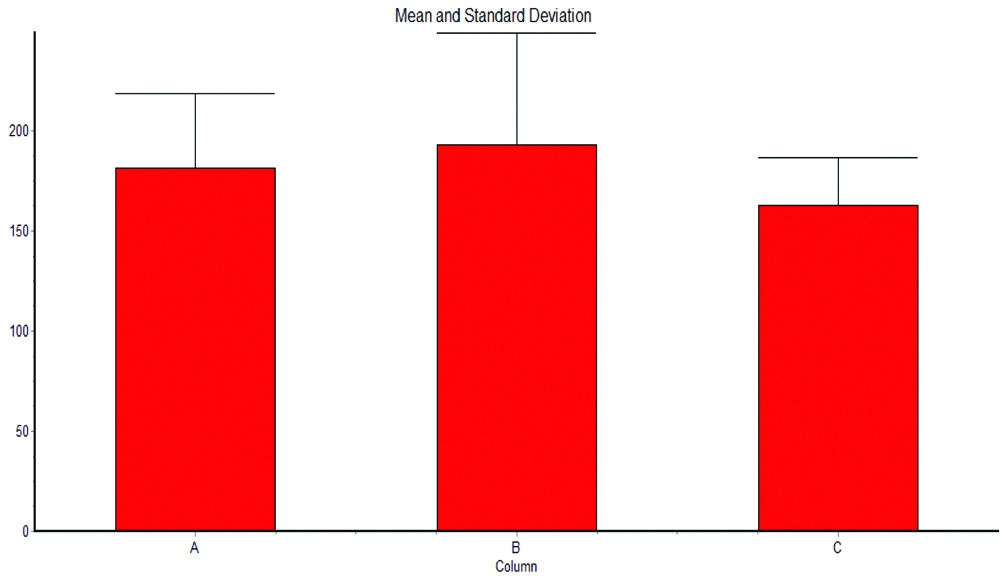
For Group I, the force required to fracture the specimen was in the range of 140.53 to 260.28 N. while it was in the range of 117.89 to 265.38 N and in the range of 117.31 to 204.82 N. for Group II and Group III, respectively [Table/Fig-7]. The mean flexural strength was 95.95 Mpa, 103.45 Mpa and 86.22 Mpa for Group I, Group II and Group III, respectively [Table/Fig-8]. The mean Flexural strength values of the three groups showed that Group II had the highest mean Flexural strength value followed by Group I, Group III. However, the differences between these Groups were statistically insignificant [Table/Fig-9].
Comparative statistics of Flexural strength.
| Group A: Triplex | Group B: Lucitone | Group C: Dentek |
|---|
| Sample No. | Flexural load (N) | Flexural strength (MPa) | Sample No. | Flexural load (N) | Flexural strength (MPa) | Sample No. | Flexural load (N) | Flexural strength (MPa) |
|---|
| No. 1 | 157.58 | 83.48 | No. 1 | 230.59 | 122.16 | No. 1 | 144.35 | 76.47 |
| No. 2 | 203.25 | 107.67 | No. 2 | 170.61 | 90.38 | No. 2 | 186.39 | 98.74 |
| No. 3 | 140.53 | 74.45 | No. 3 | 121.52 | 64.37 | No. 3 | 163.26 | 86.49 |
| No. 4 | 162.48 | 86.07 | No. 4 | 117.89 | 62.45 | No. 4 | 204.82 | 108.50 |
| No. 5 | 158.95 | 84.21 | No. 5 | 207.76 | 110.06 | No. 5 | 157.38 | 83.37 |
| No. 6 | 176.40 | 93.45 | No. 6 | 253.23 | 134.15 | No. 6 | 176.79 | 93.65 |
| No. 7 | 144.45 | 76.52 | No. 7 | 265.38 | 140.59 | No. 7 | 152.19 | 80.62 |
| No. 8 | 187.96 | 99.57 | No. 8 | 230.60 | 122.46 | No. 8 | 117.31 | 62.14 |
| No. 9 | 219.32 | 116.19 | No. 9 | 207.80 | 110.24 | No. 9 | 161.89 | 85.76 |
| No. 10 | 260.28 | 137.89 | No. 10 | 125.85 | 77.64 | No. 10 | 163.26 | 86.49 |
| Average | | 95.95 | | | 103.45 | | | 86.22 |
Mean Flexural strength of three study groups.
| Group | No. of points | Mean | Standard deviation | Standard error of mean | Median |
|---|
| 1 | 10 | 95.950 | 19.878 | 6.286 | 89.760 |
| 2 | 10 | 103.45 | 28.222 | 8.925 | 110.15 |
| 3 | 10 | 86.223 | 12.575 | 3.976 | 86.125 |
One-way ANOVA- flexural strength.
| | Mean difference | p-value | F-Value |
|---|
| Triplex | Lucitone | -7.5 | 0.712 | 1.658 |
| Dentek | 9.72 | 0.568 |
| Lucitone | Dentek | 17.227 | 0.183 |
Comparative evaluation of Impact and Flexural strength of all 3 study groups along with the standard deviation showed in [Table/Fig-10,11], respectively.
Impact strength of three study groups.
Flexural strength of three study groups.
Discussion
Acrylic resin is universally accepted and used widely today as a denture base material. The resistance to fracture of acrylic dentures depends on two important properties- flexural and impact strength of that material. Denture fractures usually occur because of insufficient flexural strength and impact strength [16]. Over the years, various modifications were attempted to improve overall properties of the Poly Methyl Methacrylate (PMMA). The modifications include chemical modification or mechanical reinforcement. The autoclave processing technique is another method to improve properties of acrylic resins in comparison to conventional water-bath processing technique [33]. Focus of this study was to evaluate the impact and flexural strength of three different commercially available chemically modified high impact heat cure denture base resins. Results of the present study showed that the flexural and impact strength of different brands of high impact denture base materials were different. So, the null hypothesis was rejected in this study.
In a study done by Gupta A and Tewari RK the authors compared the impact strength and transverse strength of the high-impact materials- Trevalon Hi, DPI Tuff and Metrocryl Hi [12]. Trevalon was used as a control, which is a conventional heat polymerised resin; the study observed that incorporation of butadiene styrene rubber resulted in increase in impact strength as compared to the control group. Shibat Al Hamd YA and Dhuru VB compared the physical and mechanical properties of pressure-molded (Lucitone 199 and ProBase Hot) and injection-molded (SR-Ivocap) denture base materials [34]. It was seen that ProBase Hot had less bending deflection but higher flexural strength values than other two materials (p<0.05). At the same time Lucitone (PMMA-grafted resin) showed least flexural strength and higher bending deflection when compared to all other materials tested. In another study Ajaj-Alkordy NM and Alsaadi MH compared the flexural strength of Lucitone 199, a high-impact resin and Rodex, a conventional resin resulted into higher flexural strength (p=0.001) of Lucitone 199 [35]. Jagger DC et al., compared impact strength of five “high strength” acrylic materials with a conventional heat cured resin [36]. The results of the study demonstrated that the impact strength was highest for Metrocryl Hi and lowest for Trevalon. Three out of the five materials namely; Metrocryl Hi, Lucitone 199, and N.D.S Hi had higher impact strength than the control group (Trevalon) which was statistically significant. There was no significant difference between Enigma Hi-base (7.73 kJ m-2) and Sledgehammer (7.40 kJ m-2) as compared with the control (4.94 kJ m-2).
Limitation(s)
In the present study, conventional denture base resin could have been used as a control group.
Conclusion(s)
The study concluded that DENTEK had the highest impact strength followed by TRIPLEX and LUCITONE while LUCITONE had the highest flexural strength followed by TRIPLEX and DENTEK but the difference between the three study materials in terms of flexural strength was statistically insignificant.
Similar studies can be undertaken in different clinical set-up to underline the results of this in-vitro study. So then clinician can choose the denture base material accordingly which will be an evidence based practice.
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Feb 12, 2020
Manual Googling: Apr 15, 2020
iThenticate Software: May 04, 2020 (19%)
[1]. Pande NA, Shori K, Comparative evaluation of impact and flexural strength of four commercially available flexible denture base materials: An in vitro studyJ Indian Prosthodont Soc 2013 13(4):499-508.10.1007/s13191-012-0203-024431782 [Google Scholar] [CrossRef] [PubMed]
[2]. Alla RK, Swamy R, Vyas R, Konakanchi A, Conventional and Contemporary polymers for the fabrication of denture prosthesis: Part I- Overview, composition and propertiesInt J Appl Dent Sci 2015 1(4):82-89. [Google Scholar]
[3]. Frederick A, Rueggeberg From vulcanite to vinyl, a history of resins in restorative dentistryJ Prosthet Dent 2002 87:364-79.10.1067/mpr.2002.12340012011846 [Google Scholar] [CrossRef] [PubMed]
[4]. Eden SE, Kerr WJS, Brown J, A clinical trial of light cure acrylic resin for orthodontic useJ Orthod 2002 29(1):51-55.10.1093/ortho/29.1.5111907310 [Google Scholar] [CrossRef] [PubMed]
[5]. Narendra R, Reddy NS, Reddy SD, Purna S, Shekar MC, Balasubramanyam S, A comparative evaluation of impact strength of conventionally heat cured and high impact heat cured polymethyl methacrylate denture base resins: An in vitro studyJ Contemp Dent Pract 2013 14(6):1115-21.10.5005/jp-journals-10024-146124858761 [Google Scholar] [CrossRef] [PubMed]
[6]. Aunsavice KJ, Philip’s science of dental materials c2003 11th edSt. LouisW.B. Saunders:143-70. [Google Scholar]
[7]. Craig RG, Powers JM, Restorative Dental Materials c2002 11th edMissouri: St. Mosby, Louis:636-89. [Google Scholar]
[8]. Sushma R, Vande AV, Malvika SR, Kore AR, Sanyal PK, A comparative study of the mechanical properties of clear and pink colored denture base acrylic resinsAnn Afr Med 2018 17:178-82.10.4103/aam.aam_65_1730588930 [Google Scholar] [CrossRef] [PubMed]
[9]. Tench RW, The use of synthetic resins in denture prosthesisJ Dist Dent Soc 1940 26:01-09. [Google Scholar]
[10]. Beyli MS, von Fraunhofer JA, An analysis of causes of fracture of acrylic resin denturesJ Prosthet Dent 1981 46:238-41.10.1016/0022-3913(81)90206-7 [Google Scholar] [CrossRef]
[11]. Jagger DC, Harrison A, Jandt KD, Review The reinforcement of denturesJ Oral Rehabil 1999 26:185-94.10.1046/j.1365-2842.1999.00375.x10194725 [Google Scholar] [CrossRef] [PubMed]
[12]. Gupta A, Tewari RK, Evaluation and comparison of transverse and impact strength of different high strength denture base resinsIndian J Dent Res 2016 27:61-65.10.4103/0970-9290.17983327054863 [Google Scholar] [CrossRef] [PubMed]
[13]. O’Brien WJ, Dental Materials and their selection c1997 2nd edChicago (IL)Quintescence Pub:85-86. [Google Scholar]
[14]. Peyton FA, History of resins in dentistryDent Clin North Am 1975 19(2):211-22. [Google Scholar]
[15]. Naik AV, Complete denture fractures: A clinical studyJ Indian Prosthodont Soc 2009 9(3):148-50.10.4103/0972-4052.57084 [Google Scholar] [CrossRef]
[16]. Khalid H, Causes and types of complete denture fractureZanco J Med Sci 2018 15(3):36-40. [Google Scholar]
[17]. El-Sheikh AM, Al-Zahrani SB, Causes of denture fracture: A surveySaudi Dental Journal 2006 18:149-54. [Google Scholar]
[18]. Dabbar U, Huggett R, Harrison A, Denture fracture- surveyBr Dent J 1994 176:342-45.10.1038/sj.bdj.48084498024869 [Google Scholar] [CrossRef] [PubMed]
[19]. Jadhav SS, Sanyal PK, Tewary S, Guru R, Joshi S, Kore AR, Comparison of mechanical strength of palatal denture base using four mesh designs on shallow palatal vault configuration: An in vitro studyInt J Prev Clin Dent Res 2017 4(3):01-09.10.5005/jp-journals-10052-0109 [Google Scholar] [CrossRef]
[20]. Chauhan MR, Wadkar AP, Rehabilitation of an edentulous patient with reinforced maxillary complete denture: A case reportInt J Dent Health Sci 2014 1(5):809-14. [Google Scholar]
[21]. Ashby M, Materials selection in mechanical design 2011 Butterworth-Heinemann:4010.1016/B978-1-85617-663-7.00005-9 [Google Scholar] [CrossRef]
[22]. Yee A, Impact resistance. In: Mark HF (ed)Encyclopedia of polymer science and technology c1987 Volume 82nd edNew YorkWiley:36-68. [Google Scholar]
[23]. Kelly E, Fatigue failures in denture base polymersJ Prosthet Dent 1969 21:257-66.10.1016/0022-3913(69)90289-3 [Google Scholar] [CrossRef]
[24]. Lambrecht JR, Kydd WL, A functional stress analysis of the maxillary complete denture baseJ Prosthet Dent 1962 12(5):865-72.10.1016/0022-3913(62)90039-2 [Google Scholar] [CrossRef]
[25]. Nandal S, Ghalaut P, Shekhawat H, Gulati M, New era in denture base resins: A reviewDent J Adv Stud 2013 1(3):136-43.10.1055/s-0038-1671969 [Google Scholar] [CrossRef]
[26]. Naji A, Kashi J, Behroozibakhsh M, Hajizamani H, Habibzadeh S, Recent advances and future perspectives for reinforcement of poly(methyl methacrylate) denture base materials: A literature reviewJ Dent Biomater 2018 5(1):490-502. [Google Scholar]
[27]. Rodford RA, The development and evaluation of high impact strength denture base materialJ Dent Res 1986 14:214-17.10.1016/0300-5712(86)90004-7 [Google Scholar] [CrossRef]
[28]. Rodford RA, Further development and evaluation of high impact strength denture base materialsJ Dent 1990 18:151-57.10.1016/0300-5712(90)90056-K [Google Scholar] [CrossRef]
[29]. Kanie T, Fujii K, Arikawa H, Inoue K, Flexural properties and impact strength of denture base polymer reinforced with woven glass fibersDental Materials 2000 16:150-58.10.1016/S0109-5641(99)00097-4 [Google Scholar] [CrossRef]
[30]. Vijay A, Prabhu N, Balakrishnan D, Narayan A, Comparative study of the flexural strength of high impact denture base resins reinforced by silver nanoparticles and e-glass fibres: An in-vitro studyJ Clin Diagn Res 2018 12(11):ZC22-26.10.7860/JCDR/2018/36931.12285 [Google Scholar] [CrossRef]
[31]. Gad MM, Al-Thobity AM, Rahoma A, Abualsaud R, Al-Harbi F, Akhtar S, Reinforcement of PMMA denture base material with a mixture of ZrO2 nano-particles and glass fibersInt J Dent 2019 2019:2489393. 1110.1155/2019/248939330809260 [Google Scholar] [CrossRef] [PubMed]
[32]. Jaikumar RA, Karthigeyan S, Ali SA, Naidu NM, Kumar RP, Vijayalakshmi K, Comparison of flexural strength in three types of denture base resins: An in vitro studyJ Pharm Bio Allied Sci 2015 7(Suppl 2):S461-S464.10.4103/0975-7406.16350526538898 [Google Scholar] [CrossRef] [PubMed]
[33]. Abdulwahhab SS, High-impact strength acrylic denture base material processed by autoclaveJ Prosthodont Res 2013 57:288-93.10.1016/j.jpor.2013.08.00424120309 [Google Scholar] [CrossRef] [PubMed]
[34]. Shibat Al Hamd YA, Dhuru VB, Physical and mechanical properties of pressure-molded and injection-molded denture base acrylics in different conditionsSaudi J Oral Sci 2014 1:65-70.10.4103/1658-6816.138463 [Google Scholar] [CrossRef]
[35]. Ajaj-Alkordy NM, Alsaadi MH, Elastic modulus and flexural strength comparisons of high-impact and traditional denture base acrylic resinsSaudi Dent J 2014 26:15-18.10.1016/j.sdentj.2013.12.00524532960 [Google Scholar] [CrossRef] [PubMed]
[36]. Jagger DC, Jagger RG, Allen SM, Harrison A, An investigation into the transverse and impact strength of “high strength” denture base acrylic resinsJ Oral Rehabil 2002 29:263-67.10.1046/j.1365-2842.2002.00830.x11896843 [Google Scholar] [CrossRef] [PubMed]