May Thurner Syndrome: A Case Report and its Endovascular Management
P Sudhakar1, B Amirthaganesh2, T Lokeshkumar3, CS Prabhu4
1 Postgraduate, Department of Radiology, Mahatma Gandhi Medical College and Research Institute, SBV Deemed to be University, Pondicherry, India.
2 Professor, Department of Cardiology, Mahatma Gandhi Medical College and Research Institute, SBV Deemed to be University, Pondicherry, India.
3 Associate Professor, Department of Radiology, Mahatma Gandhi Medical College and Research Institute, SBV Deemed to be University, Pondicherry, India.
4 Associate Professor, Department of Radiology, Mahatma Gandhi Medical College and Research Institute, SBV Deemed to be University, Pondicherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. B Amirthaganesh, 110, 10th Cross Anugraha Satellite Township, Perikattupalayam, Cuddalore District, Cuddalore-605007, Tamil Nadu, India.
E-mail: amirtha2001@rediffmail.com
May Thurner syndrome (MTS) is an anatomical variant in which right common iliac artery compresses the left common iliac vein against the lumbar vertebrae resulting in Deep Venous Thrombosis (DVT) of left lower limb in patients with no obvious cause. It is most common in middle-aged women. This is a case report of 48-year-old female who came with complaint of progressively increasing swelling of her left lower limb since one week duration with occasional mild pain. Venous Doppler and CT venogram were done, which suggested MTS, for which she underwent percutaneous transluminal angioplasty and stenting to the left common iliac vein. Immediately after this procedure, the left lower limb venous blood flow returned to normal with some residual thrombus in popliteal vein. Doppler ultrasonography was done after four months which showed patent stent with smooth flow across it and with ~60-70% recanalisation in external iliac vein, common femoral and femoral vein; ~70-80% recanalisation in popliteal vein. The present case report emphasises that MTS should be considered as a cause of acute left lower limb DVT in middle-aged women without any predisposing factors and endovascular treatment (Percutaneous transluminal angioplasty with stenting) is the most practical and effective method of treatment.
Left common iliac vein, Left lower limb DVT, Percutaneous transluminal angioplasty and stenting
Case Report
A 48-year-old female presented to the Emergency Department with complaint of progressively increasing swelling of her left lower limb since one week duration with occasional mild pain. She had no history of similar complaints, trauma, previous surgery. No significant medical and family history was given. On admission, her blood pressure was 110/70 mmHg and pulse rate was 80 beats per minute. On clinical examination, her vitals were stable; and swelling was warm and tender. No evident dilated veins or ulcers were noted; No evident ischemic changes were noted. Arterial pulse in both lower limbs including popliteal and dorsalis pedis arteries had normal palpable pulse. Since patient didn’t have clinical symptoms and signs suggesting a peripheral arterial disease, ankle-brachial index was not done and it was planned to proceed with lower limb Doppler sonography.
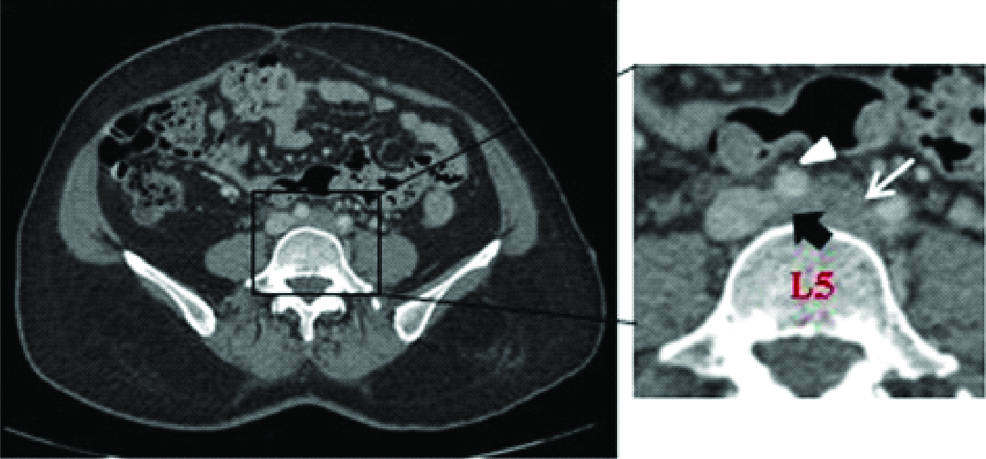
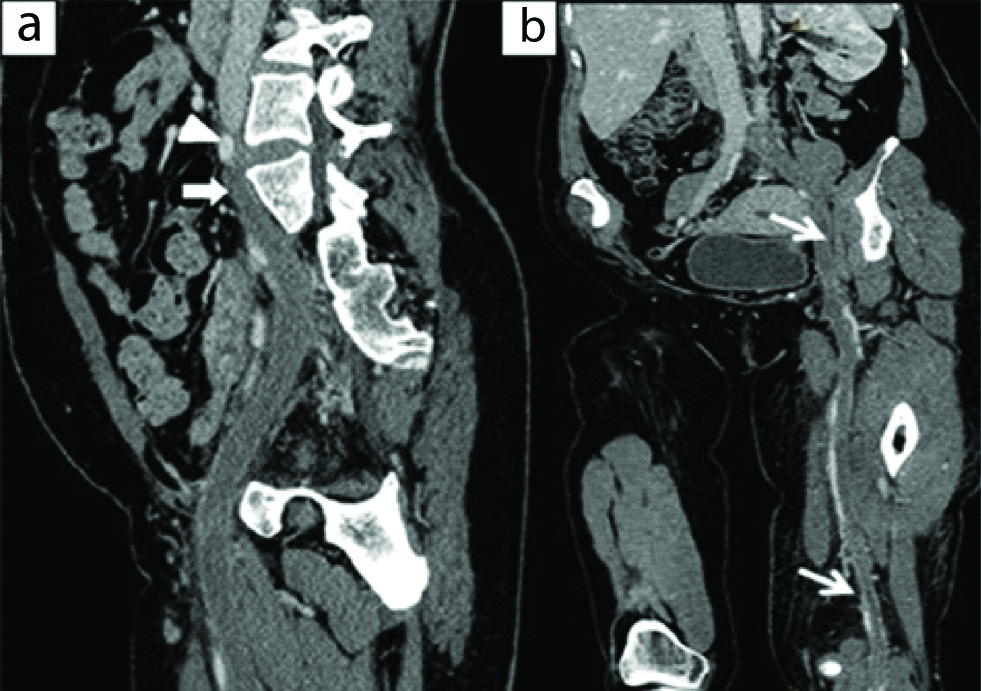
Basic workups including routine blood investigation, chest radiograph, ECG, ECHO were normal. Following which the patient was referred to the Radiology Department for a lower limb venous Doppler, which revealed an extensive left lower limb DVT involving left common iliac vein up to the popliteal vein; however, IVC appeared normal. CT venogram revealed- Left common iliac vein with more transverse course at its origin and is seen compressed between the right common iliac artery and the lumbar (L5) vertebrae with evident thrombus [Table/Fig-1] and involving the left common iliac vein extending up to the popliteal vein [Table/Fig-2a,b], suggestive of MTS.
Axial CT image showing left common iliac vein with more transverse course at its origin and is seen compressed (black arrow) between the right common iliac artery (White arrow head) and the lumbar (L5) vertebrae with evident thrombus involving the left common iliac vein (White arrow).
Sagittal and coronal curved reformatted CT venogram shows: a) Right common iliac artery (white arrow head) seen compressing over the left iliac vein (white arrow); b) Evident thrombus involving the left common iliac vein (white arrow) from its origin extending up to the popliteal vein.
Written informed consent was obtained for mechanical thrombectomy. Patient was kept in prone position; under local anaesthesia left popliteal vein was punctured with micro-puncture needle under USG guidance. An 8F sheath was introduced. Thrombus in popliteal vein, femoral vein, external iliac vein and common iliac vein was crossed using exchange length straight tip catheter (0.035’ Terumo wire). AngioJet catheter introduced via the straight tip catheter (Terumo wire) and Streptokinase infusion was given locally on the entire length of thrombus for a dwelling time of one hour. Then, mechanical thrombectomy was done using AngioJet catheter system for 480 seconds. Final venogram showed good flow and well resolved thrombus with tight stenosis at the origin of left common iliac vein obstruction which confirmed the diagnosis of MTS.
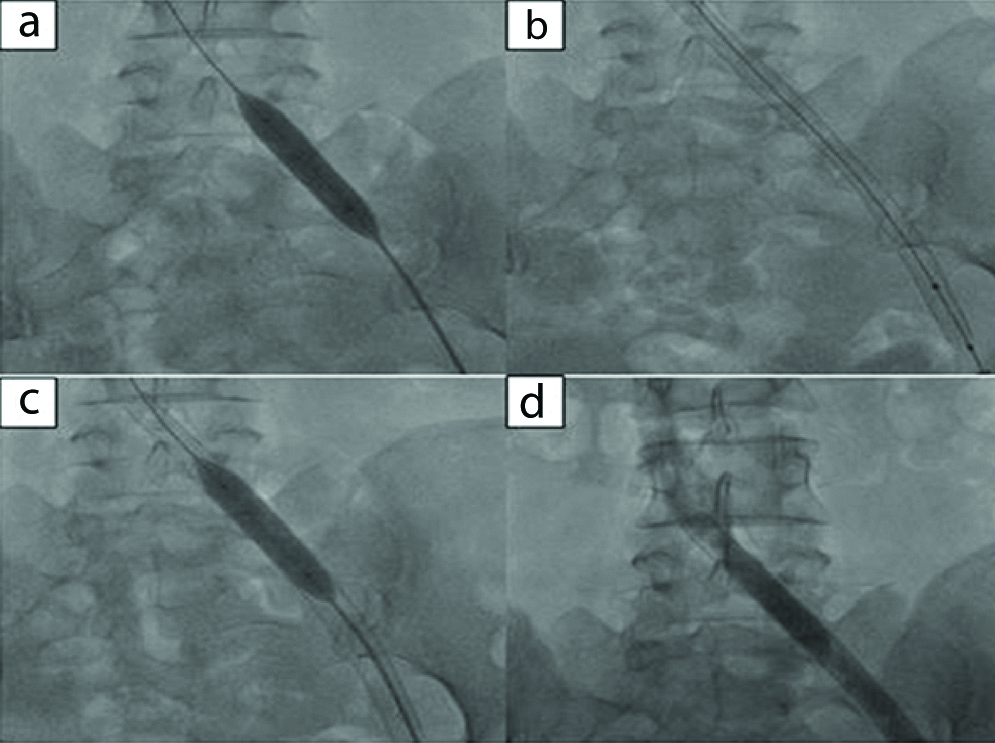
After a week, Venoplasty with stenting was planned and written informed consent was obtained for the same. Patient was positioned in prone; Left popliteal vein was punctured with micro-puncture needle under USG guidance. A 10F sheath was placed. Recurrence of thrombus noted in the popliteal, femoral and iliac veins. Hence, decided for a repeat AngioJet thrombectomy before Venoplasty. AngioJet thrombectomy was done from left common iliac vein to popliteal vein for 480 seconds using Heparin (5000U) saline as an anticoagulant. Sequential Venoplasty of left common iliac vein, external iliac vein, common femoral vein and femoral vein was done using a 9 mm × 40 mm balloon catheter (Mustang Balloon dilatation catheter) [Table/Fig-3a]. Stenting was done for narrow constricted part in left common iliac vein using a 16 mm × 90 mm self-expandable stent (Self-expandable wall stent, Boston Scientific) [Table/Fig-3b] and post-dilated with 14 mm × 40 mm balloon catheter (Mustang Balloon dilatation catheter), especially at the common iliac vein to expand the in-stent stenosis segment [Table/Fig-3c]. Final venogram showed the condition of the wall expanded stent was adequate with good flow across it [Table/Fig-3d] and with some residual thrombus within in left popliteal vein.
Digital Subtraction left Venogram showing: a) Balloon dilatation after crossing the lesion with 0.035’ terumo wire; b) Deployed stent in the left common iliac vein; c) In-stent balloon dilatation-in view of residual stenosis; and d) Showing evident good flow through the stent in the left iliac vein with no residual stenosis.
After the procedure, the patient received subcutaneous injection of low molecular weight heparin (60 mL) twice daily for 3 days and continued with per oral administration of Dabigatran 110 mg twice daily. After a week, she improved symptomatically and on clinical examination, there was no significant swelling in the left lower limb; Doppler ultrasonography at the time of discharge showed patent stent with smooth flow across it, with partial recanalisation (60-70% recanalisation in external iliac vein, common femoral vein, femoral vein and popliteal vein) involving the left lower limb deep venous system. She was advised to continue with the tablet Rivaroxaban and Clopilet along with a DVT stocking and suggested for review. On follow-up four months after the procedure she had no complaints of pain and swelling in the left lower limb; Doppler ultrasonography showed patent stent with smooth flow across it, and chronic thrombus with partial recanalisation (60 to 70% recanalisation in external iliac vein, common femoral vein, femoral vein and 80 to 90% recanalisation in popliteal vein) involving the left lower limb deep venous system.
Discussion
In 1851, Virchow R, stated that thrombosis of the pelvic veins occurs 5 times more frequently on the left side when compared to the right, especially in the left common iliac vein [1,2]. Later in 1957, May R and Thurner J, discovered an anatomical variant of left common iliac vein which had a vascular thickening at the point where it was crossed and compressed against the fifth lumbar vertebrae by overlying right common iliac artery which results in DVT of left lower limb [3]. This anatomical variant is known as MTS’. Most of the MTS cases are under-diagnosed and literatures have reported an association of 25% DVT of left lower limb with MTS [2,4]. Hence, awareness about this condition is important especially in cases of left leg DVT in middle-aged (20-40 years) women with no evident predisposing factors [4].
Though, the exact incidence and prevalence of MTS are still not known [5], the clinical prevalence of MTS related lower limb DVTs account for 2%-3% [4]. This is because majority of the patients are asymptomatic and rest presents with acute DVT of left lower limb without any obvious cause; other clinical manifestations include lower limb swelling, pain, venous claudication, ulcerations, and varicose veins [6]. Apart from DVT, two other major complications are iliac vein rupture and post thrombotic syndrome [7].
USG Doppler of lower limb is the initial modality of choice in patients presenting with leg pain or swelling, has a limited role in diagnosing MTS especially in patients with Type I and II MTS to assess the compressibility of iliac vein which can be challenging. In such cases, MTS is easily missed. CT venography because of its high sensitivity and specificity can effectively detect MTS and its types and it is also useful to exclude the other compressive causes of lower limb swelling/pain [8].
Conventional venography with Intravenous Ultrasonogram (IVUS) is imaging modality of choice in a suspected case of MTS. This can help in evaluating the nature of vessel wall and lumen, its diameter and nature of the thrombus. This further helps in selection of stent with appropriate size and length. In addition to this, it helps in accurate deployment of the stent [6].
Endovascular treatment which includes catheter guided thrombolysis/balloon angioplasty and stenting is the practical and effective method for treating MTS. Zhang X et al., showed similar outcome and concluded that endovascular treatment was a feasible and safest treatment of MTS [9] which is similar to present case.
In a retrospective study conducted by Shi WY et al., among 233 patients, the endovascular management (PTA and stent placement) for MTS was successful in 225 patients (96.6%) [10]. They have demonstrated that with percutaneous transluminal angioplasty with stenting showed a primary patency rate of 93.2% in 1 year, 84.3% in 3 years and 74.5% in 5 years over a median follow-up time of 34 months. Finally, they have concluded that endovascular treatment for MTS is safe and effective. Along with this post-procedural anticoagulation therapy is advised for a minimum period of six months, unless there is a contraindication [11].
Conclusion(s)
It is very important to consider MTS as a cause of DVT, especially in middle-aged women with left lower limb pain or swelling with no other obvious cause, because of its significant morbidity and mortality. The key to successful diagnosis lies in the multimodal approach which includes initial ultrasonogram Doppler, CT venogram and conventional venogram with IVUS. Current case report shows that endovascular treatment (PTA with stenting) is the most practical and effective method of treatment in the case of MTS.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 05, 2020
Manual Googling: Apr 20, 2020
iThenticate Software: Apr 27, 2020 (14%)
[1]. Virchow R, Ueber die Erweiterung kleinerer GefäfseArchiv F pathol Anat 1851 3(3):427-62.10.1007/BF01960918 [Google Scholar] [CrossRef]
[2]. Kibbe MR, Ujiki M, Goodwin AL, Eskandari M, Yao J, Matsumura J, Iliac vein compression in an asymptomatic patient populationJournal of Vascular Surgery 2004 39(5):937-43.10.1016/j.jvs.2003.12.03215111841 [Google Scholar] [CrossRef] [PubMed]
[3]. May R, Thurner J, The cause of the Predominantly Sinistral Occurrence of Thrombosis of the Pelvic VeinsAngiology 1957 8(5):419-27.10.1177/00033197570080050513478912 [Google Scholar] [CrossRef] [PubMed]
[4]. O’Sullivan GJ, Semba CP, Bittner CA, Kee ST, Razavi MK, Sze DY, Endovascular management of iliac vein compression (May-Thurner) syndromeJ Vasc Interv Radiol 2000 11(7):823-36.10.1016/S1051-0443(07)61796-5 [Google Scholar] [CrossRef]
[5]. Dogan OF, Boke E, Three cases with May-Thurner syndrome: A possibly under-reported disorderVASA 2005 34(2):147-51.10.1024/0301-1526.34.2.14715968901 [Google Scholar] [CrossRef] [PubMed]
[6]. Knuttinen M-G, Naidu S, Oklu R, Kriegshauser S, Eversman W, Rotellini L, May-Thurner: Diagnosis and endovascular managementCardiovasc Diagn Ther 2017 7(Suppl 3):S159-64.10.21037/cdt.2017.10.1429399519 [Google Scholar] [CrossRef] [PubMed]
[7]. Kim YH, Ko SM, Kim HT, Spontaneous rupture of the left common iliac vein associated with May-Thurner syndrome: Successful management with surgery and placement of an endovascular stentBJR 2007 80(956):e176-79.10.1259/bjr/6937193317762051 [Google Scholar] [CrossRef] [PubMed]
[8]. Liu Z, Gao N, Shen L, Yang J, Zhu Y, Li Z, Endovascular treatment for symptomatic iliac vein compression syndrome: A prospective consecutive series of 48 patientsAnn Vasc Surg 2014 28(3):695-704.10.1016/j.avsg.2013.05.01924559785 [Google Scholar] [CrossRef] [PubMed]
[9]. Zhang X, Shi X, Gao P, Wang J, Li S, Yao S, Endovascular management of May-Thurner syndrome: A case reportMedicine 2016 95(4):e254110.1097/MD.000000000000254126825895 [Google Scholar] [CrossRef] [PubMed]
[10]. Shi WY, Gu JP, Liu CJ, He X, Lou WS, Endovascular treatment for iliac vein compression syndrome with or without lower extremity deep vein thrombosis: A retrospective study on mid-term in-stent patency from a single centerEur J Radiol 2016 85(1):07-14.10.1016/j.ejrad.2015.10.02126724643 [Google Scholar] [CrossRef] [PubMed]
[11]. Moudgill N, Hager E, Gonsalves C, Larson R, Lombardi J, DiMuzio P, May-Thurner syndrome: Case report and review of the literature involving modern endovascular therapyVascular 2009 17(6):330-35.10.2310/6670.2009.0002719909680 [Google Scholar] [CrossRef] [PubMed]