The most common impacted teeth in the oral cavity are the mandibular third molars [1]. The high chances of this impaction are due to a variety of factors like inadequate retromolar space, the unfavourable path of eruption, malposition of the tooth germ, and heredity; which can cause serious conditions such as cyst formation or development of neoplastic lesions [1]. It is one of the most routinely performed surgical procedures in Oral and Maxillofacial Surgery [2]. Surgical removal of impacted third molar can cause trauma to the adjacent bone and soft tissues and is often associated with post-operative inflammatory complications like pain, swelling, trismus, and discomfort to the patient [3].
Most of the treatment modalities have some disadvantages, associated with potential side effects and need specialised equipment [7,10,11,13,15-17]. This study chooses the use of a non-invasive, elastic KT for the effective management of post-operative complications after surgical extraction of the lower third molar. The application of KT was done from supraclavicular region to the point of maximum swelling which helps in enhancing lymphatic flow by lifting the skin, increasing the interstitial space, and improving the circulation of blood and lymph [2,18-20].
The tape is water-resistant and can remain on the skin for 3 to 5 days. In Oral and Maxillofacial Surgery, only a few studies have been done to assess the effectiveness of post-operative kinesio taping [2,8,19,20]. Among them, only one study by Ristow O et al., investigated the utility of KT application in the management of post-operative complications after third molar extraction [2]. The authors found that KT application significantly reduced pain, swelling, and trismus following third molar removal [2]. Thus, the aim of the study was to evaluate the effectiveness of KT in reducing post-operative complications like pain, swelling, trismus, and its influence on the quality of life after surgical extraction of impacted mandibular third molars.
Materials and Methods
This interventional study was done between January 2018 and July 2019 in the Department of Oral and Maxillofacial Surgery of GITAM Dental College and Hospital, Visakhapatnam. The study involves 80 patients who reported with slightly or moderately difficult impacted lower third molar according to Pederson difficulty index [23]. After selecting the patients who fulfilled inclusion criteria, they underwent surgical removal of their impacted mandibular 3rd molars. The nature and design of the clinical study were explained to all the patients and informed consent was taken from them for the study. Ethical clearance for the present study was obtained by the institutional review board and the ethics committee of Gitam Dental College and Hospital.
Inclusion Criteria:
Healthy individuals (Patients between 18 and 40 years of age with no systemic disease, history of allergy, or bleeding problems) indicated for lower third molar surgical extraction.
Patients who were willing to participate in the study.
Moderately and slightly difficult impactions according to Pederson difficulty index [23].
Exclusion Criteria:
Medically compromised patients. (Patients with existing heart disease; hepatic or renal disease; blood dyscrasias; known hypersensitivities; autoimmune disease).
Patients with bone pathologies.
Patients who were not willing to participate in the study.
Teeth with periapical pathology.
Patients allergic to tape. (Patients who developed any itching sensation or redness in the immediate 24 hours of tape application were considered to be allergic).
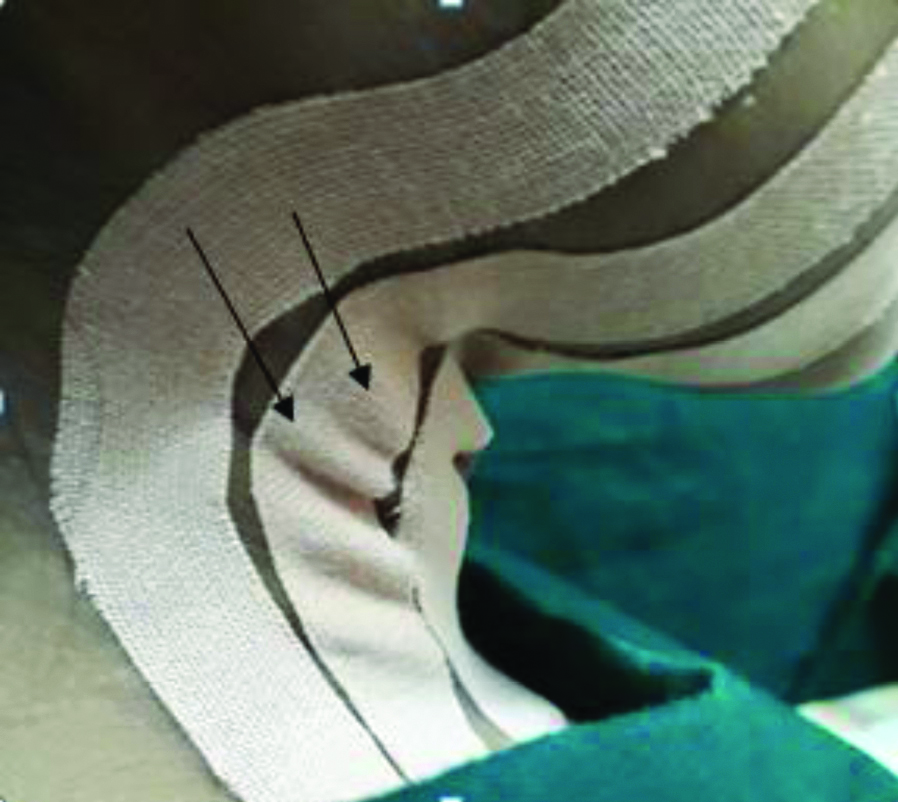
Patients who visited the Department of Oral and Maxillofacial Surgery for surgical extraction of impacted mandibular third molar were randomly divided into Groups A and B. Randomisation was carried out by allocating patients who fulfilled the inclusion criteria into Group A and Group B, alternatively. Group A received analgesics and antibiotics alone, whereas Group B received KT along with analgesics and antibiotics. This study chooses the use of a noninvasive, elastic KT [Table/Fig-1] for the effective management of post-operative complications after surgical extraction of the lower third molar. The application of KT is done from supraclavicular region to the point of maximum swelling [Table/Fig-2].
Kinesiologic tape application.

Skin lifting below the taped area (black arrow).
The pain intensity was evaluated subjectively using a 10 point Visual Analogue Scale (VAS), with the patient keeping a mark on the numerical rating scale to indicate pain intensity range from no pain ‘0’ to severe or unbearable pain ‘10’ [2].
The trismus was evaluated by measuring the inter incisal distance between the upper and lower central incisors for maximum mouth opening with the help of a divider [Table/Fig-3]. The post-operative swelling was measured by means of a five-line measurement [2] using a flexible plastic tape measure [Table/Fig-4,5]. The pre-operative sum of all the five-line measurements were considered as the baseline and the difference between each post-operative and the baseline measurements would give the changes in the facial swelling.
Measuring the inter incisal distance using a divider.

Image showing Five-line measurement of swelling.
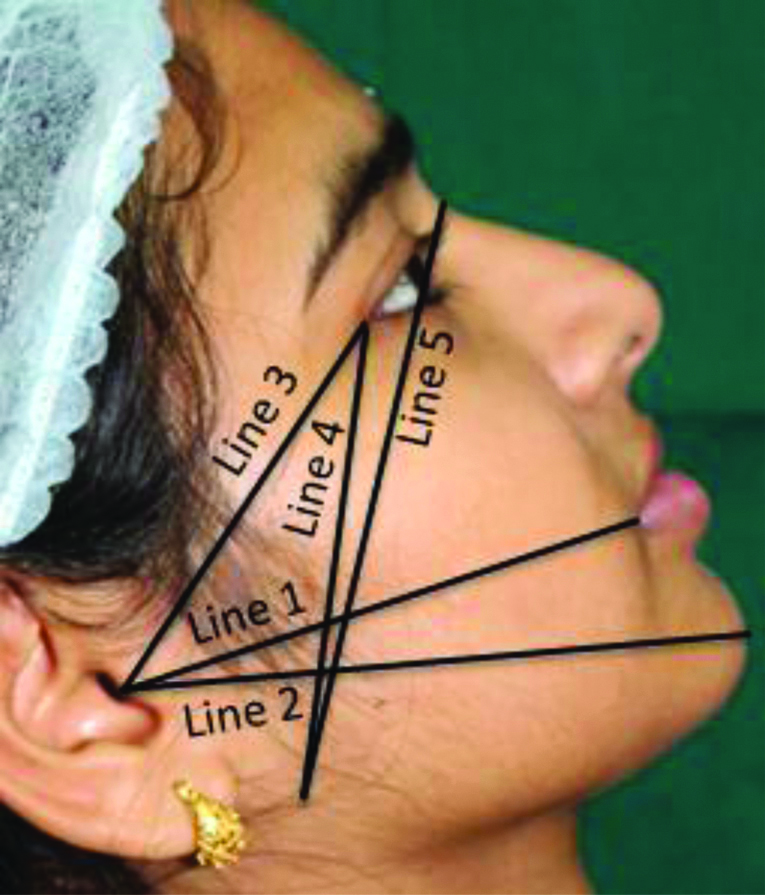
Five-line measurement of swelling.
| Five-line measurement of swelling |
|---|
| Line 1 | The most posterior point of tragus to the most lateral point of the lip commissure |
| Line 2 | The most posterior point of tragus to the pogonium |
| Line 3 | The most posterior point of tragus to the lateral canthus of the eye |
| Line 4 | The lateral canthus of eye to the most inferior point angle of the mandible |
| Line 5 | The most inferior point angle of mandible to the midpoint of the nasal bone |
Quality of life was evaluated using the Likert type scale with an oral health-related questionnaire and its 7 domains [24] [Table/Fig-6]. The scoring was given according to Likert-Type Scale: Score 0: Never, Score 1: Hardly ever, Score 2: Occasionally, Score 3: Fairly often, Score 4: Very often [24].
OHIP-14 questionnaire and its domains.
| OHIP-14 Questionnaire and its domains |
|---|
| Domain | Item |
|---|
| Domain 1: Functional limitation | 1. Had trouble pronouncing any words |
| 2. Felt sense of taste has worsened |
| Domain 2: Physical pain | 3. Had painful aching |
| 4. Found it uncomfortable to eat any foods |
| Domain 3: Psychological discomfort | 5. Been self-conscious |
| 6. Felt tense |
| Domain 4: Physical disability | 7. Felt diet has been unsatisfactory |
| 8. Had to interrupt meals |
| Domain 5: Psychological disability | 9. Found it difficult to relax |
| 10. Been a bit embarrassed |
| Domain 6: Social disability | 11. Been a bit irritable |
| 12. Had difficulty doing usual jobs |
| Domain 7: Handicap | 13. Felt life less satisfying |
| 14. Been totally unable to function |
Statistical Analysis
The data were collected on sheets and entered in MS-Excel and analysed in SPSS (version 22). Descriptive statistics were represented with percentages and Mean±standard deviation. Independent t-test was applied to find the statistical significance by comparing measurements of pain, trismus, swelling, and quality of life between the two groups (Inter group comparisons) for different observations during the various follow-up days (Pre-operative, 3rd, 5th and 7th days). Repeated ANOVA was applied to find the statistical significance and to compare the measurements of pain, trismus, swelling, for difference within each group (intra groups comparisons) for different observations during the various follow-up days (Pre-operative, 3rd, 5th, 7th days). In all the tests p-value less than 0.05 was accepted as statistically significant.
Results
A total of 80 patients were taken into the study, who were randomly divided into two equal groups. Two patients from Group A were excluded, due to incomplete follow-up, and two patients from Group B were excluded, as they developed an itching sensation within 24 hours of tape application. Thus, the effective sample size was 76 (n=38 for each group). The percentage of females and males for Group A and Group B is presented in [Table/Fig-7]. The mean age of total patients in Group A and Group B is presented in [Table/Fig-8].
Gender wise distribution of cases in Group A and B.
| Gender | Group A | Group B |
|---|
| Frequency | Percentage | Frequency | Percentage |
|---|
| Female | 16 | 42.1 | 30 | 78.9 |
| Male | 22 | 57.9 | 8 | 21.1 |
| Total | 38 | 100 | 38 | 100 |
The mean age of individuals in Group A and Group B.
| Groups | Age (Years) |
|---|
| Minimum | Maximum | Mean | SD |
|---|
| Group A | 18 | 38 | 25.89 | 5.99 |
| Group B | 18 | 40 | 27.08 | 6.30 |
The pre-operative mean pain score for Group A was 2.89, which was taken as baseline. On the 3rd, 5th and 7th post-operative days, the mean pain scores for Group A were 4.71, 3.87 and 2.95, respectively. It can be inferred that there was a significant (p=0.0001) difference in pain at baseline and on 3rd, 5th and 7th post-operative days in Group A. The pre-operative mean pain score for Group B was 2.76, which was taken as baseline. The mean pain scores for Group B at 3rd, 5th and 7th post-operative days were 2.66, 1.45, and 0.37, respectively [Table/Fig-9]. It can be inferred that there was a significant (p=0.0001) difference in pain at baseline and on 3rd, 5th and 7th post-operative days in Group B. There was no significant difference between the groups (A and B) in the pre-operative pain score with a p-value 0.37. There was a significance difference between the groups (A and B) in pain scores on various post-operative days (3rd, 5th and 7th) p-value <0.0001. It can thus be inferred that there was a significant decrease in pain on each of the post-operative days (3rd, 5th and 7th) in Group B when compared to Group A.
Comparison of pain between group A and group B at pre-operative, 3rd, 5th and 7th post-operative days.
| Duration after surgery | Pain | t-value | p-value |
|---|
| Group A | Group B |
|---|
| Mean | SD | Mean | SD |
|---|
| Pre-operative | 2.89 | 0.65 | 2.76 | 0.63 | 0.89 | 0.37 |
| 3rd day | 4.71 | 0.65 | 2.66 | 0.75 | 12.76 | <0.0001* |
| 5th day | 3.87 | 0.62 | 1.45 | 1.13 | 11.55 | <0.0001* |
| 7th day | 2.95 | 0.70 | 0.37 | 0.75 | 15.54 | <0.0001* |
| p-value | 0.0001* | 0.0001* | | |
The results of inter group comparison was done by using Independent t-test and intra group (Pre-op, 3rd day, 5th day and 7th day) comparison was done by using Repeated ANOVA test.
*Significant; SD: Standard deviation
The pre-operative mean mouth opening (trismus score) for Group A was 42.66 mm, which was taken as baseline. On the 3rd, 5th and 7th post-operative days, the mean mouth opening for Group A were 30.82 mm, 33.42 mm and 36.92 mm, respectively. It can be inferred that there was a significant difference in mouth opening (p=0.0001) at baseline and on 3rd, 5th and 7th post-operative days in Group A. The pre-operative mean mouth opening for Group B was 40.97 mm, which was taken as baseline. The mean mouth opening (trismus score) for Group B at 3rd, 5th and 7th post-operative days were 35.11 mm, 38.42 mm, and 40.68 mm, respectively [Table/Fig-10]. It can be inferred that there was significant (p=0.0001) difference in mouth opening at baseline and on 3rd, 5th and 7th post-operative days in Group B. There was no significant difference between the groups (A and B) in the pre-operative mouth opening with a p-value 0.13. There was a significant difference between the groups (A and B) in mouth opening on various follow-up days (3rd, 5th and 7th) with p-values 0.0026, 0.0001, and 0.0013 respectively. It can be inferred that there was significant improvement in trismus on each of the post-operative days (3rd, 5th and 7th) in Group B when compared to Group A.
Comparison of trismus by mouth opening between group A and group B at pre-operative, 3rd, 5th and 7th post-operative days.
| Days after surgery | Mouth opening (mm) | t-value | p-value |
|---|
| Group A | Group B |
|---|
| Mean | SD | Mean | SD |
|---|
| Pre-operative | 42.66 | 4.74 | 40.97 | 5.00 | 1.51 | 0.13 |
| 3rd day | 30.82 | 5.85 | 35.11 | 6.14 | 3.12 | 0.0026* |
| 5th day | 33.42 | 5.73 | 38.42 | 5.09 | 4.02 | 0.0001* |
| 7th day | 36.92 | 5.27 | 40.68 | 4.53 | 3.34 | 0.0013* |
| p-value | 0.0001* | 0.0001* | | |
The results of inter group comparison was done by using Independent t-test and intra group (Pre-op, 3rd day, 5th day and 7th day) comparison was done by using Repeated ANOVA test
*Significant; SD: Standard deviation
The pre-operative mean swelling for Group A was 11.83 cm, which was taken as baseline. On the 3rd, 5th and 7th post-operative days, the mean swellings for Group A were 12.67 cm, 12.49 cm, and 12.17 cm, respectively. It can be inferred that there was a significant difference in swelling (p=0.0001) at baseline and on 3rd, 5th and 7th post-operative days in Group A. The pre-operative mean swelling for Group B was 11.68 cm, which are taken as baseline. The mean swellings for Group B on 3rd, 5th and 7th post-operative days were 12.09 cm, 11.72 cm, and 11.48 cm, respectively [Table/Fig-11]. It can be inferred that there was a significant difference in swelling (p=0.0001) at baseline, 3rd, 5th and 7th post-operative days in Group B. It was observed that there was no significance difference between the groups (A and B) in the pre-operative swelling score with a p-value 0.4415. It was observed that there was a significant difference in swelling between the groups (A and B) on post-operative days (3rd, 5th and 7th) swelling with p-values of 0.0061, 0.0003 and 0.0010, respectively. It can thus be inferred that there was a significant decrease in swelling on each of the post-operative days (3rd, 5th and 7th) in Group B when compared to Group A.
Comparison of swelling between group A and group B at pre-operative, 3rd, 5th and 7th post-operative days.
| Days after surgery | Swelling (cm) | t-value | p-value |
|---|
| Group A | Group B |
|---|
| Mean | SD | Mean | SD |
|---|
| Pre-operative | 11.83 | 0.85 | 11.68 | 0.84 | 0.26 | 0.4415 |
| 3rd day | 12.67 | 0.92 | 12.09 | 0.87 | 2.82 | 0.0061* |
| 5th day | 12.49 | 0.93 | 11.72 | 0.83 | 3.81 | 0.0003* |
| 7th day | 12.17 | 0.95 | 11.48 | 0.80 | 3.47 | 0.0010* |
| p-value | 0.0001* | 0.0001* | | |
The results of inter group comparison was done by using Independent t-test and intra group (Pre-op, 3rd day, 5th day and 7th day) comparison was done by using Repeated ANOVA test
*Significant; SD: Standard deviation
On the 3rd, 5th and 7th post-operative days, the mean Quality of Life (QOL) scores for Group A were 12.29, 9.24, and 6.66, respectively. It can be inferred that there was a significant difference in QOL (p=0.0001) on 3rd, 5th and 7th post-operative days in Group A. The mean quality of life scores for Group B on 3rd, 5th and 7th post-operative days were 7.29, 4.61, and 1.63, respectively [Table/Fig-12]. It can be inferred that there was a significant (p=0.0001) difference in QOL on 3rd, 5th and 7th post-operative days in Group B. It was observed that there was a significant difference in quality of life between the groups (A and B) on post-operative days (3rd, 5th and 7th) with p-value=0.0001. It can thus be inferred that there was a significant improvement in quality of life on each of the post-operative days (3rd, 5th and 7th) in Group B when compared to Group A.
Comparison of quality of life between group A and group B at 3rd, 5th and 7th post-operative days.
| Days after surgery | Quality of life | t-value | p-value |
|---|
| Group A | Group B |
|---|
| Mean | SD | Mean | SD |
|---|
| 3rd day | 12.29 | 2.08 | 7.29 | 2.15 | 10.30 | 0.0001* |
| 5th day | 9.24 | 1.85 | 4.61 | 1.76 | 11.17 | 0.0001* |
| 7th day | 6.66 | 1.94 | 1.63 | 1.62 | 12.26 | 0.0001* |
| p-value | 0.0001* | 0.0001* | | |
The overall results showed Group B with KT helps in reducing post-operative pain, trismus, swelling, and improving the quality of life more effectively when compared with Group A.
Discussion
Surgical extraction of impacted mandibular third molars is one of the most frequent surgical procedures performed by Oral and Maxillofacial surgeons [25]. The surgical removal of tooth leads to inflammation, which in turn causes post-operative pain, swelling, and trismus, which quite adversely, affects the quality of life of the patients post-operatively [2].
The present study was designed to use therapeutic KT to minimise the post-operative complications in patients undergoing third molar surgery. The advantages of KT are that it is easy to handle (simple to use), non-invasive, less traumatic, cost-effective, light weight and has ventilation characters (free movement of air through the skin as KT is made of 100% cotton) [2]. The disadvantages of KT are that it causes friction due to elasticity of tape; can irritate the skin and sometimes adhesives may produce allergic reaction [2]. KT is generally used for rehabilitation of sports injuries [26].
After surgical extraction of the mandibular molar, pain generally peaks after 3-5 hours and continues for 2-3 days, gradually diminishing by day 7 [5]. According to the existing literature, the elastic nature of KT causes stretching and lifting of the skin during movement, which arouses low-threshold cutaneous mechanoreceptors and reduction in pain [2,8,22]. Kase K et al., found out that KT decreases pain by alleviating pressure on nociceptors and thereby helps in pain reduction [22].
In the present study, pain was assessed using VAS and it was observed that the patients in Group B had less pain (p=0.0001) when compared with the Group A on 3rd, 5th and 7th post-operative days after third molar surgery which is in coherence with the study done by Ristow O et al., [2]. Ristow O et al., studied the effectiveness of KT following wisdom teeth removal and showed a significant decrease in the post-operative pain [2]. KT is found to reduce the pain by decreasing the pressure on nociceptors [2]. Tozzi U et al., evaluated the effects of KT after orthognathic surgery, and found that KT serves as a useful technique for managing post-operative pain [19]. In two other studies, Ristow O et al., utilised KT after surgical treatment of patients with zygomatico-orbital and mandibular fractures and stated that KT helps in the reduction of post-operative pain and improves patient satisfaction [18,20].
Oedema is a clinical state primarily defined as the collection of excessive plasma proteins in tissue spaces, which occurs when the lymphatic fluid exceeds the capacity of the lymphatic system [27]. Szolnoky G et al., used manual lymphatic drainage on post-operative swelling after impacted third molar removal [17]. KT application creates a pulling force resulting in the characteristic skin elevations below the taped area, which is believed to increase the interstitial space between the skin and underlying connective tissue, thus favouring the blood, lymphatic flow and thus reduces swelling [28].
The maximum swelling is usually seen on 2nd and 3rd post-operative days and lasts for one week following surgery [18]. This study uses a five-line measurement [2] for the post-operative changes in facial volume. There was significant reduction in facial swelling after application of KT, which is in coherence with the studies done by Tozzi U et al., in orthognathic surgeries [19] and Ristow O et al., in managing the third molar surgery and mandibular fractures [2,18].
Trismus (inability to open mouth) reduces markedly after third molar surgery, which can be associated with pain and swelling in the early 72 hours [12]. There was a significant improvement in the mouth opening in Group B when compared to Group A (p<0.05) in the study, which is comparable to the study done by Ristow O et al., [2].
In the immediate post-operative days, the QoL is affected in most of the patients with common post-operative complaints such as pain, trismus and swelling [24]. QoL is defined as an individual’s assessment of how the functional, psychological, and social factors affect his or her well-being in relation to orofacial concerns [24]. Negreiros RM et al., reported the oral health-related quality of life of patients after lower third molar surgery and found that the patients having teeth with greater degree of surgical difficulty, had higher OHIP scores on all subscales [24]. McGrath C et al., reported the changes in oral health related quality of life in patients following third molar surgery. They emphasised that there is a significant deterioration in oral health related quality of life, as it is associated with trismus and swelling in the early post-operative period after which slowly recovers to a pre-operative level [29]. The surgical procedure causes inflammatory reactions that lead to post-operative pain, trismus, and swelling which is quite annoying and discomfort to the patients. The present study found that the application of KT helps in reducing the post-operative pain, trismus, swelling thereby presenting significant improvement of QoL and greater satisfaction by the patients post-operatively.
Limitation(s)
Further studies are advised with larger sample size, including impactions with slight to very difficult scores according to modified Pederson’s criteria in a split-mouth design (to reduce the inter subject variability, give precise treatment results) with bilateral symmetrical impacted teeth to determine the effect of KT after mandibular third molar removal.
Conclusion(s)
The KT can be used as a potential adjunct to other treatment modalities in managing post-surgical complications such as pain, trismus and swelling. It is a simple, non-invasive, and safe method to improve the quality of Life after impacted mandibular third molar surgery.
The results of inter group comparison was done by using Independent t-test and intra group (Pre-op, 3rd day, 5th day and 7th day) comparison was done by using Repeated ANOVA test.
*Significant; SD: Standard deviation
The results of inter group comparison was done by using Independent t-test and intra group (Pre-op, 3rd day, 5th day and 7th day) comparison was done by using Repeated ANOVA test
*Significant; SD: Standard deviation
The results of inter group comparison was done by using Independent t-test and intra group (Pre-op, 3rd day, 5th day and 7th day) comparison was done by using Repeated ANOVA test
*Significant; SD: Standard deviation