Orbital Cellulitis in Paediatric Patient with Sinusitis
Gurnoor Singh1, Anand Kumar Bhardwaj2, Gauri Chauhan3, Bharat Bhushan Singh4
1 Junior Resident, Department of Paediatrics, Maharishi Markandeshwar Institute of Medical Sciences and Research, Mullana, Haryana, India.
2 Professor and Head, Department of Paediatrics, Maharishi Markandeshwar Institute of Medical Sciences and Research, Mullana, Haryana, India.
3 Assistant Professor, Department of Paediatrics, Maharishi Markandeshwar Institute of Medical Sciences and Research, Mullana, Haryana, India.
4 Junior Resident, Department of Paediatrics, Maharishi Markandeshwar Institute of Medical Sciences and Research, Mullana, Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Gauri Chauhan, Maharishi Markandeshwar Institute of Medical Sciences and Research, Mullana-133203, Haryana, India.
E-mail: pgfinalgauri@gmail.com
Orbital cellulitis is a serious complication of sinusitis. It is a common life-threatening infection of the post-septal tissues of the orbit and one of the most common causes of orbital inflammation. A five-year-old boy presented to Emergency room with pain and swelling of right eye with history of cough, coryza and fever. He was immediately hospitalised and broad-spectrum antibiotics were started on an empirical basis. MRI showed sign of ethmoidal sinusitis with orbital cellulitis. Functional endoscopic sinus surgery was done and pus was drained from ethmoidal and maxillary sinuses. As child recovered, he was discharged after 14 days course of antibiotics (Ceftriaxone, Metronidazole and Vancomycin). Treatment of such cases usually requires multidisciplinary collaborated management by Paediatric, Radiology, Otorhinolaryngology and Surgical team.
Ethmoidal sinusitis, Functional endoscopic sinus surgery, Multidisciplinary management
Case Report
A five-year-old boy had fever with chills and rigor, cough, coryza from last five days following that he developed blurring of vision, watering, pain and swelling of right eye since three days [Table/Fig-1].
Pre-treatment picture showing displacement of the right eye.

Child was conscious, irritable and had tachycardia with high grade fever. Blood pressure was within normal limits. On physical examination, there was swelling and erythema over the right eye which was warm and tender. Further, Ophthalmic examination showed right eyelid oedema, with proptosis of the right eye. Bulbar conjunctiva was found to be congested and papillary reaction was difficult to assess due to restricted eye-opening. On visualising the fundus, it showed a distinct disc margin with C:D ratio 0.3 and the active and passive eye movements were also restricted. The left eye had mild upper lid oedema and the rest was clear.
Ear, Nose and Throat (ENT) examination revealed no external deformity. Mucopurulent discharge was present in the right vestibule and the left vestibule was normal. Septum was oedematous.
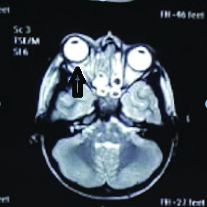
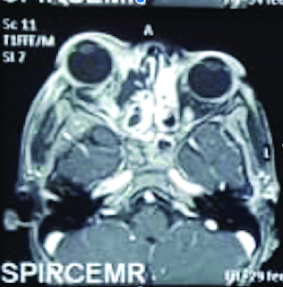
The routine blood investigations were done which showed raised White Blood Cells (WBCs). Magnetic Resonance Imaging (MRI) brain with orbits revealed ill-defined fluid collection in the right orbit extending along floor appearing hyperintense on T2, hypointense on T1 and showing peripheral enhancement on post-contrast scan and destruction of lamina papyracea and marked stranding in retrobulbar fat was also seen [Table/Fig-2,3]. Collection was measuring 6.8 mm in maximum diameter. There was associated inflammation of medial rectus as well as inferior rectus which were thickened and oedematous.
Axial T2 weighted image showing a large area of hypertense fluid signal in right orbit (black arrow) in extraconal space in subperiosteal location extending medially along the floor.
Axial T1 weighted fat suppressed contrast image showing peripheral enhancement of fluid collection in medial orbital wall subperiosteal region partially extending into the preseptal space.
The patient was started on i/v fluids and i/v antibiotics (ceftriaxone 100 mg/kg/day, metronidazole 30 mg/kg/day, and vancomycin 60 mg/kg/day).
Blood culture was suggestive of Methicillin Resistant Staphylococcus aureus (MRSA) sensitive to vancomycin. Even after four days course of antibiotics, there was no response. Functional endoscopic sinus surgery was done and pus was drained from ethmoidal and maxillary sinuses. Within 2-3 days, fever and swelling subsided and the general condition of the child was improved. Intravenous Vancomycin (60 mg/kg/day) was continued for 14 days and the child was discharged. Patient was followed up after 15 days with improvement in signs and symptoms.
Discussion
Orbital cellulitis is a common complication of ethmoidal sinusitis in children. It is an acute suppurative inflammation of orbital tissue which has an acute onset and a rapid progression. The complications of this condition namely; cavernous sinus thrombosis, meningitis, frontal abscess, osteomyelitis, loss of vision and even death have been reported due to late or ineffective treatment [1,2]. Thus, orbital cellulitis is an emergency condition and it is important to make an early diagnosis with effective treatment. Hodges E and Tabbara KF studied the complications of orbital cellulitis and found blindness in 52% of patients on admission and a mortality of 4% because of cavernous venous thrombosis [3]. There results also highlighted that treatment was ineffective in individuals who presented late in the tertiary health care set-up. Sobol SE et al., and Miglioretti DL et al., reported 60-91% of orbital cellutis secondary to sinusitis [4,5]. There is decline of orbital complications of acute sinusits due to advent of the antibiotic era [6]. An incidence of 3% complications was found by Hicks CW et al., who focussed on paediatric population [7].
Preseptal cellulitis is caused by inflammation of anterior septum which accounts for 85-87% of cases while orbital cellulitis is caused by the inflammation of posterior septum [8]. It is difficult to differentiate preseptal cellulitis from deep orbital cellulitis solely on clinical basis because of the presence of soft tissue oedema, hence the use of imaging modality becomes mandatory to arrive at proper diagnosis Contrast-enhanced CT scanning or MRI is the imaging modality of choice for detailed visualisation [9-11].
Routine Blood investigations are done at preliminary level which include Complete Blood Count (CBC), C-Reactive Protein (CRP) and sedimentation rate [11]. White blood cells are usually raised in orbital Cellulitis and rarely in case of Preseptal Cellulitis [12].
The main organism in children affected with orbital cellulitis is Streptococcus (two-thirds of cases) and Haemophilus (almost half of cases) and the treatment depends on the culture report [13]. The treatment of preseptal and orbital cellulitis requires a combined approach of a paediatrician, ophthalmologist and otorhinolaryngologist, and further advice taken from the neurosurgical and neurology teams. Frequent evaluation of the child is mandatory to assess the response to the treatment. Physician should consider other conditions like neuroblastoma, rhabdomyosarcoma, fungal infections, orbital myositis, lymphangioma, Graves’s disease, dermoid cyst rupture or inflammation, trauma, systemic conditions like sickle cell disease as it resembles orbital infections [12]. Patients with orbital cellulitis require hospitalization and treatment with a combination of intravenous antibiotics which covers for both aerobic and anaerobic infections for two weeks followed by oral antibiotics for one week. If there is visible abscess formation on CT or MRI, loss of vision, diminish ocular motility, or a clinical advancement after 24 hour therapy then surgical intervention is required. Ceftriaxone or Cefotaxime covers both gram-positive and gram-negative organisms, however, the ancillary use of flucloxacillin to cover Staphylococcus aureus is beneficial. Metronidazole is also used for anaerobic bacteria. Clindamycin use is suggested in the presence of infections with osteomyelitis or in those persons who are allergic to cephalosporins and penicillins [14].
Conclusion(s)
Delays in diagnosis of the cause and adequate treatment (medical/surgical) in case of an acute orbit may cause the progression of disease to an irreversible stage resulting in blindness. Therefore, we recommend that all the patients presenting with either fever or headache combined with symptoms or signs of orbital inflammation, should undergo orbital and sinus CT scanning without delay.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Dec 13, 2019
Manual Googling: Apr 08, 2020
iThenticate Software: Apr 27, 2020 (17%)
[1]. Hawkins DB, Clark RW, Orbital involvement in acute sinusitis: Lessons from 24 childhood patientsClin Pediatr 1977 16(5):464-71.10.1177/000992287701600510849665 [Google Scholar] [CrossRef] [PubMed]
[2]. Dossari SA, Abou-Elhamd K-EA, A case report of orbital abscess complicating ethmoidal sinusitis in 15 months girlClin Surg 2017 2(1):1289 [Google Scholar]
[3]. Hodges E, Tabbara KF, Orbital cellulitis: Review of 23 cases from Saudi ArabiaBr J Ophthalmol 1989 73(3):205-08.10.1136/bjo.73.3.2052706211 [Google Scholar] [CrossRef] [PubMed]
[4]. Sobol SE, Marchand J, Tewfik TL, Manoukian JJ, Schloss MD, Orbital complications of sinusitis in childrenJ Otolaryngol 2002 31(3):131-36.10.2310/7070.2002.1097912121013 [Google Scholar] [CrossRef] [PubMed]
[5]. Miglioretti DL, Johnson E, Williams A, Greenlee RT, Weinmann S, Solberg LI, Paediatric computed tomography and associated radiation exposure and estimated cancer riskJAMA Paediatr 2013 167:700-07.10.1001/jamapediatrics.2013.31123754213 [Google Scholar] [CrossRef] [PubMed]
[6]. Chandler JR, Langenbrunner DJ, Stevens ER, The pathogenesis of orbital complications in acute sinusitisLaryngoscope 1970 80(9):1414-28.10.1288/00005537-197009000-000075470225 [Google Scholar] [CrossRef] [PubMed]
[7]. Hicks CW, Weber JG, Reid JR, Moodley M, Identifying and managing intracranial complications of sinusitis in children: A retrospective seriesPaediatr Infect Dis J 2011 30(3):222-26.10.1097/INF.0b013e3181f8639821416657 [Google Scholar] [CrossRef] [PubMed]
[8]. Giusan AO, Kubanova AA, Uzdenova RKh, Rhinosinusogenic complications: The prevalence and principles of treatmentVestn Otorinolaringol 2010 4:64-67. [Google Scholar]
[9]. Bedwell J, Bauman NM, Management of paediatric orbital cellulitis and abscessCurr Opin Otolaryngol Head Neck Surg 2011 19(6):467-73.10.1097/MOO.0b013e32834cd54a22001661 [Google Scholar] [CrossRef] [PubMed]
[10]. Soon VT, Paediatric subperiosteal orbital abscess secondary to acutesinusitis: A 5-year reviewAm J Otolaryngol 2011 32(1):62-68.10.1016/j.amjoto.2009.10.00220031268 [Google Scholar] [CrossRef] [PubMed]
[11]. Meara DJ, Sinonasal disease and orbital cellulitis in childrenOral Maxillofac Surg Clin North Am 2012 24(3):487-96.10.1016/j.coms.2012.05.00222857719 [Google Scholar] [CrossRef] [PubMed]
[12]. Jain A, Rubin PA, Orbital cellulitis in childrenInt Ophthalmol Clin 2001 41(4):71-86.10.1097/00004397-200110000-0000911698739 [Google Scholar] [CrossRef] [PubMed]
[13]. Watts P, Preseptal and orbital cellulitis in children: A reviewPaediatrics and Child Health Symposium: Eyes and ENT 2012 22(1):01-08.10.1016/j.paed.2011.04.002 [Google Scholar] [CrossRef]
[14]. Welkoborsky HJ, Graß S, Deichmuller G, Bertram O, Hinni ML, Orbital complications in children: Differential diagnosis of a challenging diseaseEur Arch Otorhinolaryngol 2015 272(5):1157-63.10.1007/s00405-014-3195-z25056021 [Google Scholar] [CrossRef] [PubMed]