The diagnosis of OFB is difficult, especially when it is thin and small in size. The existence of OFB can be identified through various imaging tests. Birmingham Eye Trauma Terminology (BETT) and the Ocular Trauma Classification Group (OTCG) help ophthalmologists classify eye trauma [1,2]. This classification is utilised to determine the management whose primary purpose is to prepare the rehabilitation of the patients’ visual acuity. Several studies have been conducted to determine the factors that influence the expected final functional visual outcome. Recently, one of the most significant grading systems is the Ocular Trauma Score (OTS) [3,4]. OTS helps provide a predictive value of vision in open globe injury [5].
OTS is based on visual acuity and five anatomical characteristics. The visual prognosis would have a more favourable outcome if the primary damage is due to sharp object penetration confined only in the anterior segment of the eyes. The anterior segment comprises of conjunctiva, cornea, anterior chamber, and lens [6]. OTS predictive value would be utilised to compare visual acuity 60 days after OFB removal. The research result would provide clinicians with the data to help them decide the best management for OFB due to gun pellets. This notion is in relation to a previous study claiming that initial visual acuity is not the best nor the most reliable predictive factor for final visual acuity with multiple correspondence analysis [7].
The main objective of the study was to determine the prognostic value of visual acuity of patients with bullet trauma in the orbital cavity. In this case, there is a very high threat to vision, which is related to the need for hospitalisation. More specifically, the researchers aimed to provide data on the characteristics of patients who have experienced pellet injury in the orbital cavity at the study institution. All pellets in the orbital cavity were taken using a C-Arm fluoroscopy technique.
Materials and Methods
This study was conducted retrospectively using all medical records of patients with air gun pellets who were treated at Dr. Soetomo General Hospital, Surabaya, from 2011 until 2018. This study was approved by the Health Research Ethics Committee of Dr. Soetomo General Hospital/Faculty of Medicine, Universitas Airlangga (No.1135/KEPK/IV/2019) on April 25th, 2019.
The demographic data included several criteria; the first criterion was age-based on the classification of Neural Network Using GF-NET Aging Database and Wavelets. Other categories included sex, affected eyes (lateralisation), number of pellets in the orbital cavity based on orbital imaging review (skull plain x-ray and/or CT scan result). A complete eye examination included pre-operative and post-operative visual acuity, as well as post-traumatic ocular complications. The examination included eyeball rupture, endophthalmitis, perforation, and relative afferent pupillary defects in determining the OTS as seen in [Table/Fig-1] [8,9].
Ocular Trauma Score (OTS).
| Variable | Raw points |
|---|
| A. Initial visual acuity |
| - No Light Perception (NLP) | 60 |
| - Light Perception /Hand Movement (LP/HM) | 70 |
| - Counting Finger (CF)-20/400 | 80 |
| - 20/400 to 20/50 | 90 |
| - ≥20/40 | 100 |
| B. Eyeball Rupture | -23 |
| C. Endophthalmitis | -17 |
| D. Perforation of Trauma | -14 |
| E. Detached Retina | -11 |
| F. Relative Afferent Pupillary Defect (RAPD) | -10 |
NLP: No Light Perception; LP: Light Perception; HM: Hand Movement; CF: Counting Finger; RAPD: Relative Afferent Pupillary Defect
The Best-Corrected Visual Acuity (BCVA) was converted into the logarithm of the minimum angle of resolution (logMAR) unit and classified based on the assessment of visual acuity as in OTS. A more substantial log MAR value suggests a sharper vision and vice versa. The data classifications taken according to OTS standards included No Light Perception (NLP) equal to 3.00 logMAR; Light Perception (LP) equal to 2.80 logMAR; Hand Movement (HM) equal to 2.50 logMAR; Counting Fingeror CF-1/60 equal to 1.78 logMAR; 2/60 equal to 1.48 logMAR; 3/60 equal to 1.30 logMAR; 20/400, 20/200-20/50, and <20/40 data groups [10].
In this study, the orbital cavity foreign body was an air shotgun pellet and made of metal. The surgery used C-Arm guidance (OEC Brivo Prime C-Arm, GE Healthcare), performed under general anaesthesia in all patients, and was carried out by the same operator. Patients with previous ocular disease, previous ocular trauma, and/or incomplete medical records were excluded from this study.
Statistical Analysis
The statistical analysis was performed with SPSS version 16.0 for Windows. The differences in logMAR value of BCVA between pre-operative and post-operative conditions on each variable (visual acuity, foreign body, OTS score, complication, and type of operation) were tested using the Kruskal-Wallis Test and Wilcoxon-Signed Rank Test for each level. Next, the change in the value of the BCVA during pre-operative and post-operative conditions on day 1, day 7, and day 60 were tested using the Friedman Test. In the case of the correlation between variables, the authors applied Spearman Correlation and linear regression. All tests set the level of significance at 95% with a p-value of smaller than 0.05.
Results
The study found that 30 patients, 27 men (90%) and three women (10%) from 30 years to 52 years, were diagnosed with air gun pellet injury with an average age of 29.03±15.54. The most affected age group was the adult group (19-59-year-old), amounting to 21 people (70.00%), as seen in [Table/Fig-2]. All patients included in this study had undergone C-arm guided surgery under general anaesthesia, where all the pellets were successfully removed. No patients experienced surgical complications or required secondary or additional surgeries. The post-operative follow-up was limited to 60 days.
| Characteristic | Result |
|---|
| Average age (years) | 29.03±15.54 |
| Age |
| Children (0-12-year-old) | 5 (16.67%) |
| Adolescent (13-18-year- old) | 4 (13.33%) |
| Adult (19-59-year-old) | 21 (70.00%) |
| Elderly (≥60-year-old) | 0 (0%) |
| Sex |
| Male | 27 (90%) |
| Female | 3 (10%) |
| Lateralisation |
| Oculi Dextra (OD) | 14 (46.67%) |
| Oculi Sinistra (OS) | 16 (53.33%) |
From the surgical data, 14 patients were diagnosed with pellet penetration in their right eyes (46.67%), and 16 patients experienced it in their left eyes (53.33%). Total of 27 (90%) had single pellet incident. Two patients (6.67%) experienced multiple pellets and the remaining one patient (3.33%) experienced double bullet incident. The other complications recorded were eyeball rupture and retinal detachment, endophthalmitis, perforation trauma and relative afferent pupillary defects [Table/Fig-3].
The characteristics of best-corrected visual acuity on pre- and post-operative seen from the aspects of the number of bullets as foreign objects in orbital cavity, trauma scores, the condition of the affected eye complications and type of surgery.
| Variable | Level | Number (n) | Best Corrected Visual Acuity (BCVA) | Increase (+) or decrese (-) of visual acuity | Changes |
|---|
| Pre | Post |
|---|
| Average±Standard deviation | pa | Average±Standard deviation | pa | Average±Standard deviation | pb Comparison Pre and Post |
|---|
| Visual acuity |
| Mean | 30 | 2.04±1.07 | | 2.07±1.13 | | + | 0.03±0.06 | 0.937 |
| Modus | 30 | 2.9 | | 2.6 | | | 0.3 | |
| NLP | 6 | 2.80±0.30 | <0.001 | 2.80±0.29 | <0.001 | + | 0.00±0.01 | 0.564 |
| LP/HM | 12 | 2.90±4.71 | | 2.94±0.11 | | + | 0.04±4.60 | 0.317 |
| CF-20/400 | 6 | 1.40±0.11 | | 1.73±0.75 | | + | 0.33±0.64 | 0.655 |
| 20/200-20/50 | 2 | 0.20±0.00 | | 0.30±0.14 | | + | 0.10±0.14 | 0.317 |
| > 20/40 | 4 | 0.28±0.28 | | 0.37±0.28 | | + | 0.09±0.00 | 0.180 |
| Bullet foreign body |
| Single | 27 | 2.16±1.06 | 0.317 | 1.99±1.18 | 0.597 | - | 0.17±0.12 | 0.478 |
| Double | 1 | 1.30±0 | | 2.90±0 | | + | 1.60±0 | 0.157 |
| Multiple | 2 | 1.3±1.83 | | 2.75±0.21 | | + | 1.45±1.62 | 0.317 |
| Visual acuity on OTS score |
| 1 | 6 | 1.69±1.52 | 0.024 | 2.10±1.38 | <0.001 | + | 0.41±0.14 | 0.317 |
| 2 | 14 | 2.35±0.89 | | 2.07±1.07 | | - | 0.28±0.18 | 0.357 |
| 3 | 4 | 2.37±0.97 | | 2.49±0.89 | | + | 0.12±0.08 | 0.655 |
| 4 | 1 | 1.56±1.22 | | 1.33±1.64 | | - | 0.23±0.42 | 1.000 |
| 5 | 5 | 1.75±0.78 | | 1.88±1.24 | | + | 0.13±0.46 | 0.655 |
| Complication |
| No complication | 5 | 0.28±0.28 | 0.022 | 0.90±1.15 | 0.270 | + | 0.62±0.87 | 0.180 |
| Eyeball rupture | 6 | 2.63±0.71 | | 2.68±0.74 | | + | 0.05±0.03 | 0.317 |
| Endophthalmitis | 5 | 2.64±0.79 | | 2.90±0.30 | | + | 0.26±0.41 | 0.655 |
| Perforation trauma | 9 | 2.55±0.63 | | 2.42±0.92 | | - | 0.13±0.29 | 1.000 |
| Detached retina | 6 | 2.58±0.64 | | 1.93±1.28 | | - | 0.65±0.64 | 0.109 |
| Relative afferent pupillary defect | 10 | 2.27±0.94 | | 2.32±1.08 | | + | 0.05±0.14 | 0.854 |
| Type of surgery |
| Primary repair | 0 | (0/30) | | (0/30) | | | (0/30) | |
| Exploration and/or primary repair, and/or by C-Arm guide | 30 | 2.04±1.07 (30/30) | | 2.07±1.13 (30/30) | | + | 0.03±0.06 (30/30) | 0.937 |
| Enucleation | 0 | (0/30) | | (0/30) | | | (0/30) | |
aKruskal-Wallis Test; bWilcoxon-Signed Rank Test
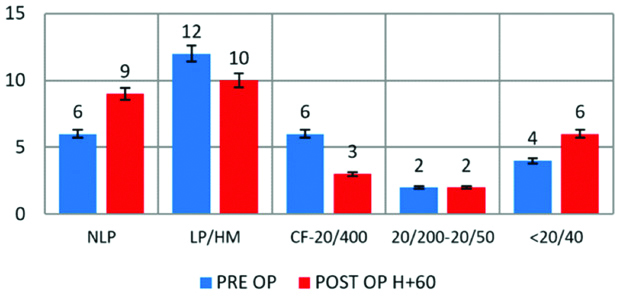
Pre-operative and Post-operative Visual Acuity
The Pre-operative visual acuity of NLP was found in six patients (20%), LP or HM in 12 patients (40%), CF-20/400 in 6 patients (20%), as well as visual acuity at the rate of ≥20/20. On average, patients came with 2.04±1.07 of visual acuity, and most of them scored 2.9 on OTS. The initial OTS score mostly indicated score 2 in 14 cases (46.67%), as seen in [Table/Fig-3].
Pre-operative and post-operative visual acuity examination on day 1 (D+1) suggested an increase in the number of patients with NLP from 6 to 9 cases. The number of LP/HM decreased in several patients from 12 to 10, CF-20/400 by 3 out of 6 cases, and visual acuity of 20/200-20/50 remained two cases. On the other hand, the visual acuity of ≥20/40 increased from 4 cases to 6 cases. The first days of the pre-operative and post-operative visual examination showed no significant difference in results with a p-value of 0.580, as seen in [Table/Fig-4].
The data of real age, lateralisation, logMAR best visual acuity, OTS score, and the number of bullets in patients who have suffered from air gun pellets.
| No | Age | Lateralisation | Pre-operative of BCVA (logMAR) | Post-operative of BCVA (LogMAR) | OTS score | Number of bullets |
|---|
| Day-1 | Day-7 | Day-60 |
|---|
| 1 | M/6 | OS | 0.30 | 0.30 | 0.30 | 0.18 | 4 | S |
| 2 | F/50 | OS | 1.48 | 1.48 | 0.40 | 0.40 | 5 | S |
| 3 | M/14 | OD | 1.78 | 1.78 | 2.50 | 2.50 | 5 | D |
| 4 | M/2 | OD | 2.50 | 2.50 | 2.50 | 2.50 | 5 | S |
| 5 | F/16 | OD | 1.78 | 1.78 | 1.78 | 1.78 | 5 | S |
| 6 | M/20 | OD | 0.00 | 0.00 | 2.50 | 2.50 | 1 | MT |
| 7 | M/17 | OD | 2.50 | 2.50 | 2.50 | 2.50 | 1 | S |
| 8 | M/19 | OD | 3.00 | 3.00 | 3.00 | 3.00 | 1 | S |
| 9 | M/21 | OS | 0.00 | 0.00 | 0.00 | 0.00 | 1 | S |
| 10 | M/11 | OS | 0.18 | 0.18 | 0.18 | 0.18 | 1 | S |
| 11 | M/35 | OD | 3.00 | 3.00 | 3.00 | 3.00 | 1 | S |
| 12 | M/20 | OS | 1.48 | 1.30 | 1.30 | 1.30 | 2 | S |
| 13 | M/33 | OD | 3.00 | 3.00 | 3.00 | 3.00 | 2 | S |
| 14 | M/22 | OS | 2.50 | 3.00 | 3.00 | 3.00 | 2 | S |
| 15 | M/12 | OS | 2.50 | 2.30 | 2.30 | 2.30 | 3 | S |
| 16 | M/49 | OS | 2.30 | 2.50 | 2.30 | 2.30 | 3 | S |
| 17 | M/48 | OS | 2.50 | 2.50 | 0.48 | 0.48 | 2 | S |
| 18 | F/52 | OS | 0.30 | 0.30 | 0.30 | 0.30 | 2 | S |
| 19 | M /50 | OS | 0.10 | 0.10 | 0.10 | 0.10 | 2 | S |
| 20 | M/3 | OS | 2.50 | 3.00 | 3.00 | 3.00 | 2 | MT |
| 21 | M/18 | OD | 3.00 | 3.00 | 3.00 | 3.00 | 2 | S |
| 22 | M/40 | OD | 2.50 | 2.50 | 2.50 | 2.50 | 1 | S |
| 23 | M/33 | OS | 2.50 | 2.50 | 2.50 | 2.50 | 2 | S |
| 24 | M/41 | OD | 2.30 | 2.30 | 2.30 | 2.30 | 3 | S |
| 25 | M/34 | OS | 1.48 | 2.30 | 2.30 | 1.48 | 3 | S |
| 26 | M/51 | OD | 3.00 | 3.00 | 3.00 | 3.00 | 3 | S |
| 27 | M/33 | OD | 3.00 | 3.00 | 3.00 | 3.00 | 3 | S |
| 28 | M/43 | OS | 0.60 | 0.60 | 0.60 | 0.60 | 3 | S |
| 29 | M/39 | OS | 1.30 | 1.30 | 1.30 | 0.18 | 4 | S |
| 30 | M/39 | OD | 2.50 | 3.00 | 3.00 | 3.00 | 4 | S |
M: Male; F: Female; OD: Oculi dextra; OS: Oculi sinistra; OTS: Ocular trauma score; S: Single: D: Double; MT: Multiple
Furthermore, the cases that experienced significant changes between pre-operative and post-operative days were observed until the 60th day. On the other hand, the visual acuity of ≥20/40 increased from 4 cases to 6 cases. Pre-operative and post-operative visual acuity on the 60th day also indicated no significantly different results with a p-value of 0.73, as seen in [Table/Fig-5].
The number of cases on each category based on OTS classification.
The OTS comparison between the pre-operative and post-operative visual acuity experienced various changes (both increase and decrease). Six patients with an OTS score of 1 suggested a score change on the average logMAR score from 1.69±1.52 to 2.10±1.38 with a p-value of 0.317. As many as 14 patients got the OTS score of 2, which decreased from 2.35±0.89 to 2.07±1.07 with a p-value of 0.357. Meanwhile, the highest OTS score of 5 occurred in five patients with an increase from 1.75±0.78 to 1.88±1.24 with a p-value of 0.655, as seen in [Table/Fig-3]. [Table/Fig-4] compared the final outcome in BCVA in 60 days and expected BCVA by OTS prediction value. There were significant differences in all OTS scores.
Management of Air Gun Pellet Injury in the Orbital Cavity
The average score of pre-operative visual acuity compared to post-operative visual acuity increased from 2.04±1.07 to 2.07±1.13 with a p-value of 0.937, as seen in [Table/Fig-3].
The Predictive Value of Post-operative Visual Acuity
[Table/Fig-6] shows that there were no significant differences between pre-operative, post-operative visual acuity on D+1, D+7, D+60, and OTS score with a p-value greater than 0.05. The correlation test between pre-operative and post-operative visual acuity using the C-Arm guidance found the correlation score of 82.3%, while the correlation of post-operative visual acuity with OTS was the same but with a lower strength of 38.2%. Therefore, it can be concluded that pre-operative visual acuity and post-operative visual acuity have a greater correlation compared to the OTS and post-operative visual acuity.
Correlation test of the results of pre-operative visual acuity to post-operative visual acuity day 1, day 7, day 60 and the OTS.
| Visual acuity | N | Average | SD | p-value |
|---|
| Pre-operative | 30 | 2.043 | 1.08713 | p>0.05a |
| Post-operative day-1 | 30 | 2.083 | 1.10300 |
| Post-operative day-7 | 30 | 2.107 | 1.10763 |
| Post-operative day-60 | 30 | 2.073 | 1.14949 |
| OTS | 30 | 2.600 | 1.32873 |
aFriedman Test
From the follow-up data, the authors noted that patients OTS score 1 tend to have a worse prognosis, in which 75% of them suffered from NLP at D+60, and 25% of them experienced HM/LP [Table/Fig-7].
Visual outcome analysis compared to predicted visual outcome by OTS score (Kuhn et al.’s table).
| OTS | NLP | LP/HM | CF-20/400 | 20/200-20/50 | ≥20/40 | p-value* |
|---|
| (%) | |
|---|
| 1 | 75/74 | 25/15 | 0/7 | 0/3 | 0/1 | 0.006 |
| 2 | 0/27 | 100/26 | 0/18 | 0/15 | 0/15 | <0.001 |
| 3 | 0/2 | 0/11 | 100/15 | 0/31 | 0/41 | <0.001 |
| 4 | 0/1 | 0/2 | 0/3 | 100/22 | 0/73 | <0.001 |
| 5 | 0/0 | 0/1 | 0/1 | 0/5 | 100/94 | <0.001 |
*chi-square test
Discussion
Foreign body trauma in the orbital cavity can cause severe morbidity. In this study, nine cases (25%) had complications in the form of eyeball perforation and consecutive rupture of the eyeballs in six cases (16.67%).
Fulcher TP et al., mentioned that perforation complications could reach 20%, while Dolars BA et al., stated that it might only reach 9%. Both studies considered that the orbital cellulitis complication was higher than the perforation [11,12].
A study conducted by Shuttleworth GN and Galloway PH, indicates that patients with trauma from air shotgun bullets have an average pre-operative score of 1.23±1.05 and increased significantly to 0.81±1.25. Furthermore, a study conducted by Tabatabaei SA et al., states that LogMAR for eye care was 2.56±1.38, which increased statistically and significantly to 2.05±1.5 in six months of post-treatment. Both studies included all types of air shotgun, and their bullets explained that their pre-operative and post-operative visual acuity was better than other foreign body trauma caused by other injuries [13,14].
From the observations made in each category of visual acuity based on OTS, there was an increase in the number of post-operative NLP patients. In the LP/HM and CF-20/400 groups, there could be better or worse visual acuity at the end of the follow-up, respectively, from 12 cases (40%) into 10 cases (33.3%) and from 6 cases (20%) into 3 cases (10%). In this study, the modus value of logMAR of pre-operative visual acuity changed from 2.50 to 3.00. Nevertheless, the mean value of the logMAR of pre-operative visual acuity was 2.01, and the mean value of post-operative D+60 reached 1.60.
In the OTS grading designed by Kuhn F et al., 74% of the patients in OTS score 1 were predicted to have NLP VA in 6 months after the accident, while 15% of the patients would have HM/LP VA [15]. In this study, 100% of the patients in OTS score 2 have HM/LP VA. These findings differ from OTS predicted VA by Kuhn F et al., reaching 27% [15]. Similar findings were also observed in OTS score 3, 4, and 5. The results from this study were significantly different from Kuhn F et al., OTS study, implying that it might not be applicable for patients with specific ocular trauma due to metallic foreign bodies such as pellets.
A research found that 48.3% of open globe injury resulted in a non-functional initial visual acuity [16]. On the other side, 41% of them still had initial visual acuity >6/60. At the end of the treatment, the study found that the visual acuity improved; non-functional initial visual acuity increased from 48.3% to 40%, while the visual acuity >6/60 improved from 41% to 60%. The prediction of poor visual acuity becomes more significant because of the risk factors, including poor initial acuity, injury effects on the eyelids, and the presence of detached retina. The study conducted by Ma J et al., mentioned that out of 56 patients studied for three years, 54 patients (96.4%) suffered from metal foreign body trauma. The average initial visual acuity was 2.3 logMAR [17]. This study shows that patients diagnosed with metal object trauma have poor initial visual acuity. Good visual acuity before surgery is a significant predictor of good final visual acuity. Poor initial visual acuity is also a significant predictor of poor final visual acuity [18]. This situation contradicts the research by Valmaggia C et al., which claims that initial visual acuity is not the best and most reliable predictive factor for final visual acuity with multiple correspondence analysis [7].
Limitation(s)
This study was limited to a small number of samples, with a short follow-up period of 60 days from the extraction. All samples studied had undergone OFB extraction using C-Arm. Therefore, the outcome of patients not undergoing OFB extraction was not studied.
Conclusion(s)
This study found that injuries resulted from the air gun pellets penetrating into the orbital cavity are more common in adult male patients. In this study, patients undergoing foreign body extraction guided by C-Arm did not experience statistically significant visual acuity worsening. OTS is used to predict the prognosis of visual acuity. However, it seems that OTS overestimates the final visual acuity in patients with a metallic OFB injury.
NLP: No Light Perception; LP: Light Perception; HM: Hand Movement; CF: Counting Finger; RAPD: Relative Afferent Pupillary Defect
aKruskal-Wallis Test; bWilcoxon-Signed Rank Test