Anaemia can have devastating results, especially when associated with thrombocytopenia. The author here report a case of 16-year-old female who presented with chief complaint of sudden, painless, nonprogressive diminution of vision in left eye past one day. Ocular examination revealed bilateral pale conjunctiva, bilateral retinal flame shaped haemorrhages, roth spots and large macular sub hyaloid haemorrhage in left eye. Complete haematological examination revealed severe megalobalstic anaemia (with Haemoglobin 4.4 gm%) with thrombocytopenia. Diagnosis of severe anaemic retinopathy due to megaloblastic anaemia with thrombocytopenia was made and the patient was advised propped up position, prescribed iron, folic acid, vitamin C and B12 supplementation. Patient underwent aggressive treatment of megaloblastic anaemia and was kept on follow-up. On follow-up, the retinal haemorrhage spontaneously resolved with clearance of fovea and the patient gained vision. Urgent diagnosis and management is mandatory in these cases. So, a good screening protocol should be established for the identification of nutritional anaemia in developing countries and compulsory fundus examination to be done of the identified subjects for anaemic retinopathy.
Case Report
A 16-year-old female presented with chief complaint of sudden painless, non-progressive diminution of vision in left eye for past one day. There was no history of hypertension, diabetes or any preceding ocular trauma, blood transfusion. Patient was very selective in food intake and vegetarian by diet.
On general examination, patient was afebrile, thin built with palmar pallor and with blood pressure 90/50 mm of Hg in right arm supine position. Pulse rate was 100/min.
On ocular examination, her visual acuity was 6/6 on Snellen’s chart right eye and only hand movement close to face with projection of rays accurate in all four quadrants in left eye. Her intraocular pressure by Goldman applanation tonometry was 12 mm of Hg and 8 mm of Hg in right and left eye respectively. Anterior segment examination revealed conjunctival pallor in both the eyes and sluggishly reactive pupil in left eye.
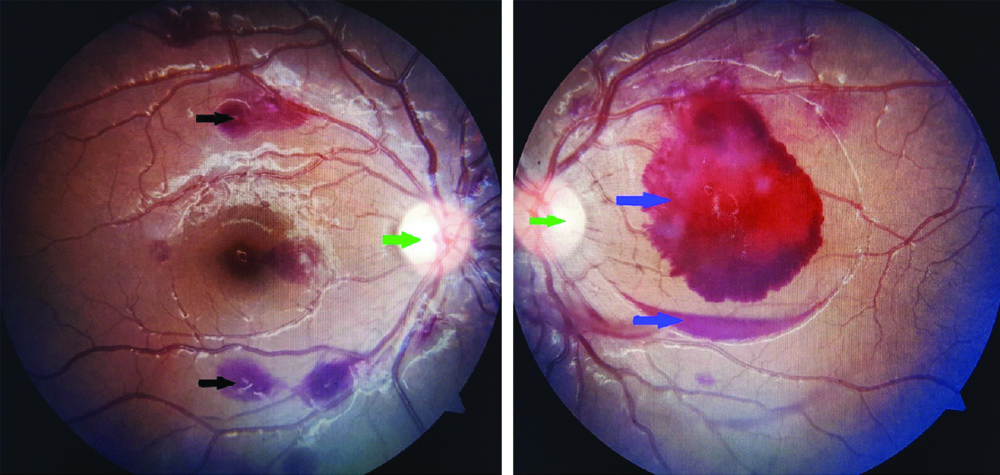
Fundus examination revealed mild disc pallor in both the eyes ([Table/Fig-1] green arrow), superficial flame shaped haemorrhages and roth spots ([Table/Fig-1] black arrow) along the superior and inferior vascular arcade in right eye and in left eye there was a large subhyaloid haemorrhage ([Table/Fig-1] blue arrow) of about 8 Disc Diameter (DD) at the macula.
Coloured fundus photograph demonstrating bilateral disc pallor (green arrow), roth spots (black arrow) and sub hyaloid haemorrhage in left eye (blue arrow).
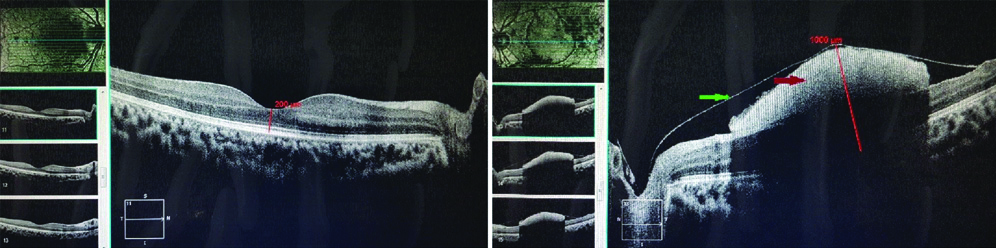
Optical coherence tomography demonstrated, Central Macular Thickness (CMT) of around 200 micron in right eye. In left eye, CMT was about 1000 micron with distortion of foveal and perifoveal contour and with a large dome shaped elevation ([Table/Fig-2] red arrow). There was posterior vitreous detachment ([Table/Fig-2] green arrow) at the elevated dome. The large hyper-reflective dome shaped elevation was casting shadow and obscured the underneath choroidal vasculature. Ganglion cell analysis revealed marked thinning in left eye forecasting poor visual prognosis. Optic nerve head analysis was comparable in both the eyes.
Optical coherence tomography revealing Central Macular Thickness (CMT) of around 200 micron in right eye and about 1000 micron in left eye with distortion of foveal and perifoveal contour by a large dome shaped elevation (red arrow). There was posterior vitreous detachment (green arrow) at the elevated dome.
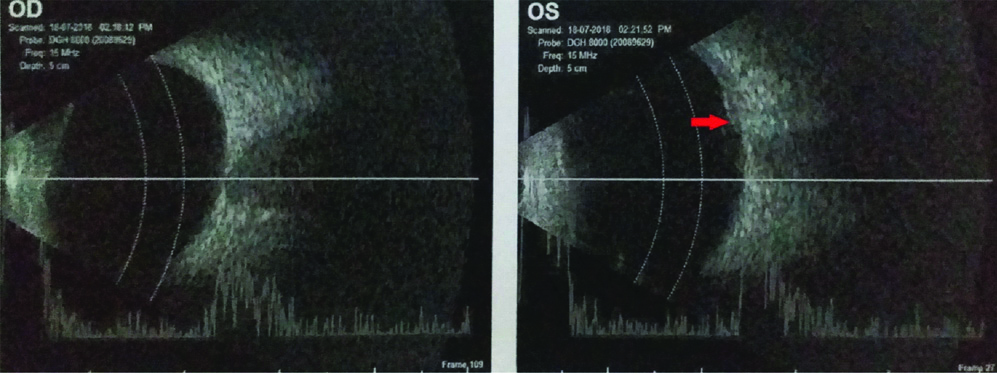
On USG B-scan, right eye posterior segment was normal but left eye revealed an elevation near the optic disc from posterior surface ([Table/Fig-3] red arrow) supporting the other findings. Axial length was 23.07 mm and 22.89 mm in right and left eye, respectively, supporting the fact that elevation at macula is present leading to decrease in axial length.
USG B scan demonstrating an elevation near the optic disc from posterior surface (red arrow).
Detailed ocular and systemic workup was done to detect the cause. Complete blood investigations revealed blood group as B positive, Haemoglobin 4.4 gm/dl (11.5-16.5 gm/dL), RBC count 1.23 million/cumm (4.0-5.5 million/cumm), TLC and DLC were within normal limits, Platelet count was only 1.1 lacs/cumm (4-5 lacs/cumm), there were no blast cells in peripheral smear, haematocrit 16.6% only (37%-48%), PT was 18 seconds (increased, normal 10-15 seconds), PT/INR was raised, aPTT was 42 seconds (25-35 seconds), ESR was 50 mm in first hour (0-20 mm first hour), plasma vitamin B12 only 41 mol/L (>400 mol/L), ferritin level was 8 microgm/L (12-270 microgm/L), normal folate levels, viral markers (HBsAg, Anti HCV, Anti HIV) were non-reactive, Kidney function test was within normal limits with mildly deranged Liver function test. Routine urine examination revealed pyuria. USG abdomen revealed cystitis and mildly altered ecotexure of liver.
As the patient was very thin built with blood pressure 90/50 mm of Hg, she was prone for poor exercise intolerance and cardiomyopathy. So, she was examined in details with echocardiography for excluding any pathology, if any. Cardiac evaluation revealed normal heart sounds with normal ECG, however 2D echocardiography revealed mild asymptomatic Atrial septal defect (L to R).
So, the diagnosis of severe megaloblastic anaemic retinopathy (L>R) with thrombocytopenia was made. Patient was advised to maintain propped up position and was subjected to aggressive treatment for megaloblastic anaemia under guarded visual prognosis in left eye. Patient was prescribed E/D Nepafenac in both eyes, also given Injection Ferric carboxymaltose 1000 mg i.v., oral antibiotics for pyuria, folic acid, Vitamin B12 and C supplementation.
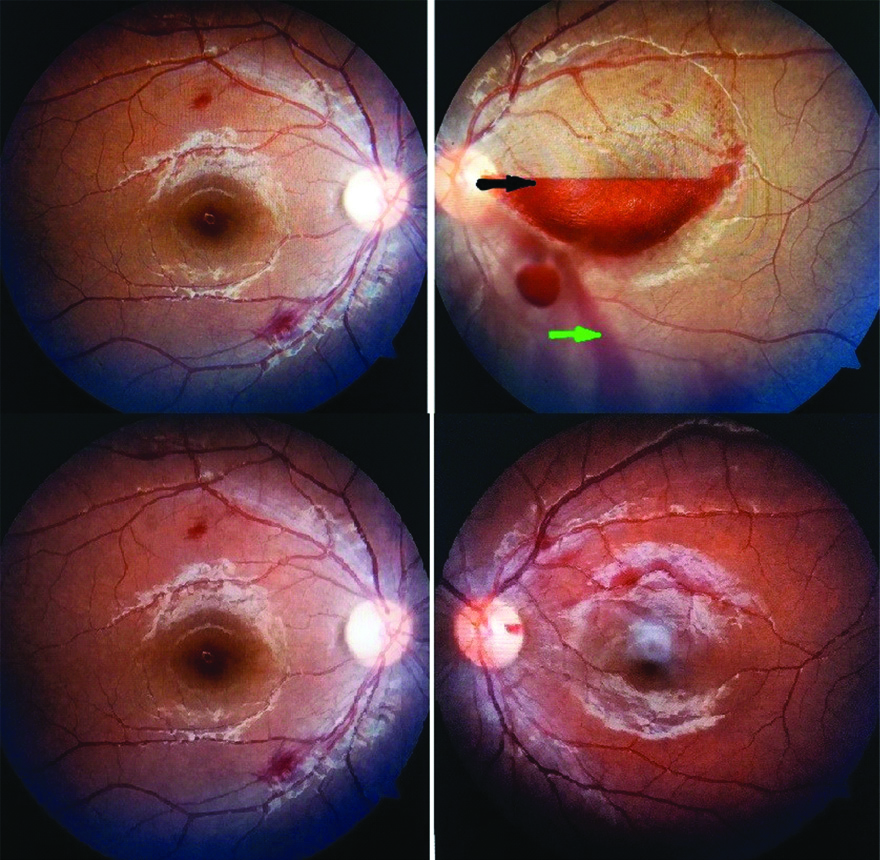
On follow-up after five days, patient’s visual acuity improved to 6/60 in left eye. On follow-up examination, the flame shaped haemorrhages in right eye resolved [Table/Fig-4] and in the left eye the large subhyaloid haemorrhage acquired a typical boat shaped configuration ([Table/Fig-4] black arrow) with dripping of blood to vitreous ([Table/Fig-4] green arrow), possibly due to spontaneous rupture into vitreous cavity [Table/Fig-4], further decreased severity of haemorrhage and finally total resolution of macular bleed [Table/Fig-4]. This had led to clearance of blood from macula and thus, improvement in visual acuity up to 6/9 in left eye till the last follow-up up to 45 days. So, no active intervention was done as the patient showed spontaneous resolution of signs and symptoms by treating the anaemic component.
Coloured fundus photograph demonstrating resolving retinal haemorrhage in right eye and typical boat shaped sub hyaloid haemorrhage (black arrow) with seeping blood in vitreous (green arrow) and subsequent clearance of macula in left eye.
Further, the patient was lost to follow-up for subsequent evaluation.
Discussion
Anaemia is characterised by decrease in number of RBC or decrease in haemoglobin in RBC’s or both. Anaemia is an important risk factor for the development of retinopathy. The clinical retinal signs of anaemic retinopathy are non-specific and may very closely resemble hypertensive or diabetic retinopathy [1]. The risk of retinopathy goes hand in hand with severity of anaemia, particularly when the haemoglobin level is below 6 gm/dl [2]. Ocular manifestations of anaemia could be conjunctival pallor, retinal haemorrhages which can be in any layer, cotton wool spots due to retinal nerve fiber layer hypoxia and infarction, roth spot, venous dilatation and arteriolar tortuosity. The combination of severe anaemia and thrombocytopenia is likely to produce retinal haemorrhages in a majority of patients [3,4].
Megaloblastic anaemia commonly develops disc pallor. The only source of vitamin B12 is animal origin, so pure vegetarians are more prone to develop megaloblastic anaemia. Retinopathy is uncommon in patients with haemoglobin levels 8 g/dL or more. The association of thrombocytopenia, especially less than 50×109/L, with anaemia increases the incidence of retinopathy [2]. Development of anaemic retinopathy can be due to multiple factors as anoxia, angiospasm, venous stasis, increased capillary permeability, thrombocytopenia, increased blood viscosity, etc.
Anaemic retinopathy is usually asymptomatic unless it affects the macula. The retinopathy resolves with the management of anaemia. Decreased vision in anaemic retinopathy can be due to haemorrhage involving macula, macular edema, macular star, disc edema, optic neuropathy or retrobulbar neuritis [5]. Approximately, 28% of anaemic patients have some form of retinopathy. If thrombocytopenia is associated, the incidence increases to 38% [5].
Retinal findings in anaemia include haemorrhages as most common finding which is mainly superficial and flame shaped, found in nerve fibre layer of retina. The haemorrhages can be of any type and involve any layer of retina. Index case demonstrated classical picture of flame shaped and subhyaloid haemorrhage (classic boat shaped). Roth spots were also present. Roth spots are also found in sub-acute bacterial endocarditis, leukaemia, hypertension, diabetes, HIV retinopathy and carbon monoxide poisoning [6]. There can be also presence of cotton wool spots that are infarcts of the nerve fibre layer of the retina due to retinal hypoxia associated with anaemia. More profound anaemia is required to produce cotton wool spots than to produce haemorrhages. Although, the patient had severe anaemia but cotton wool spots were not found. Associated retinal oedema, venous tortuosity and rarely disc edema and macular star can also be present in these cases. Besides these common clinical findings, specific anaemia can be associated with few specific findings. Vitamin B12 deficiency is notorious to develop optic neuropathy with centro caecal scotoma [6]. The patient also had mild disc pallor at presentation which recovered after aggressive treatment. Anaemia with leukaemia can have additional retinal findings as retinal leukaemic infiltrates, vascular sheathing, serous retinal detachment secondary to choroidal infiltration, microaneurysms and rarely retinal neovascularisation [6]. Iron deficiency can also represent as central retinal vein occlusion, branch retinal artery occlusion, papilloedema and rarely anterior ischemic optic neuropathy [7-9]. Anaemia associated with dengue can have additional retinal findings as dengue maculopathy, vasculitis, exudative retinal detachment and branch retinal vein occlusion [10-13].
Very few cases of retinopathy due to megaloblastic anaemia have been reported from India [14,15]. The patient, as reported by Mishra A et al., underwent resolution and no active ocular surgical intervention was required [15]. The index patient, vegetarian by diet, had classical manifestations of severe vitamin B12 deficiency megaloblastic anaemic retinopathy. The co-existence of thrombocytopenia is probably due to impaired DNA synthesis leading to impaired thrombopoiesis. Vitamin B12 supplementation in the patient showed good response with resolution of retinal findings associated with spontaneous rupture of sub hyaloid haemorrhage into vitreous cavity with clearance of macula associated with excellent regain in visual acuity.
Conclusion(s)
This case is just an addition to the prevalence of anaemic retinopathy in the general population and may represent just the tip of the iceberg. We recommend good screening protocols for the identification of nutritional anaemia in developing countries and strongly suggest compulsory fundus examination of the identified subjects for anaemic retinopathy.
[1]. Weiss LM, Anaemic retinopathyPa Med 1966 69:35-36.10.1177/0040571X6606954714 [Google Scholar] [CrossRef]
[2]. Carraro MC, Rossetti L, Gerli GC, Prevalence of retinopathy in patients with anaemia or thrombocytopeniaEur J Haematol 2001 67(4):238-44.10.1034/j.1600-0609.2001.00539.x11860445 [Google Scholar] [CrossRef] [PubMed]
[3]. Rubenstein RA, Yanoff M, Albert DM, Thrombocytopenia, anaemia, and retinal hemorrhageAm J Ophthalmol 1968 65:435-39.10.1016/0002-9394(68)93098-5 [Google Scholar] [CrossRef]
[4]. Lam S, Lam BL, Bilateral retinal hemorrhages from megaloblastic anaemia: Case report and review of literatureAnn Ophthalmol 1992 24:86-90. [Google Scholar]
[5]. Loewenstein JI, Retinopathy associated with blood anomalies. In: Jakobieck F (ed)Clinical Ophthalmology. Revised ed 1995 3(85)PhiladelphiaJ.B. Lippincott Company:995-1000. [Google Scholar]
[6]. Kaur B, Taylor D, Fundus hemorrhages in infancySurv Ophthalmol 1992 37:1-17.10.1016/0039-6257(92)90002-B [Google Scholar] [CrossRef]
[7]. Tashiro T, Takahashi H, Masuda H, Ichioka T, Complication of central retinal vein occlusion in iron deficiency anaemiaMeikai Daigaku Shigaku Zasshi 1990 19:437-42. [Google Scholar]
[8]. Kacer B, Hattenbach LO, Horle S, Scharrer I, Kroll P, Koch F, Central retinal vein occlusion and nonarteritic ischemic optic neuropathy in 2 patients with mild iron deficiency anaemiaOphthalmologica 2001 215:128-31.10.1159/00005084311244344 [Google Scholar] [CrossRef] [PubMed]
[9]. Imai E, Kunikata H, Udono T, Nakagawa Y, Abe T, Tamai M, Branch retinal artery occlusion: A complication of iron-deficiency anaemia in a young adult with a rectal carcinoidTohoku J Exp Med 2004 203:141-44.10.1620/tjem.203.14115212150 [Google Scholar] [CrossRef] [PubMed]
[10]. Bacsal KE, Chee SP, Cheng CL, Flores JV, Dengue-associated maculopathyArch Ophthalmol 2007 125:501-10.10.1001/archopht.125.4.50117420370 [Google Scholar] [CrossRef] [PubMed]
[11]. Chang PE, Cheng CL, Asok K, Fong KY, Chee SP, Tan CK, Visual disturbances in dengue fever: An answer at last?Singapore Med J 2007 48:e71-73. [Google Scholar]
[12]. Chan DP, Teoh SC, Tan CS, Nah GK, Rajagopalan R, Prabhakaragupta MK, Eye Institute dengue- related ophthalmic complications workgroup. Ophthalmic complications of dengueEmerg Infect Dis 2006 12:285-89.10.3201/eid1202.05027416494756 [Google Scholar] [CrossRef] [PubMed]
[13]. Su DH, Bacsal K, Chee SP, Flores JV, Lim WK, Cheng BC, Prevalence of dengue maculopathy in patients hospitalized for dengue feverOphthalmology 2007 114:1743-47.10.1016/j.ophtha.2007.03.05417561258 [Google Scholar] [CrossRef] [PubMed]
[14]. Vidya H, Neelam P, Anupama B, Sowmya PD, Subhyaloid haemorrhage in severe dimorphic anaemiaand thrombocytopaenia- A case reportJournal of Clinical and Diagnostic Research 2010 4(5):3201-02. [Google Scholar]
[15]. Mishra A, Gururaja R, Aggarwal S, Bhargav N, Chaudhary N, Megaloblastic anaemia in a teenage patientMed J Armed Forces India 2015 71(Suppl 2):S435-39.10.1016/j.mjafi.2014.10.00526843761 [Google Scholar] [CrossRef] [PubMed]