Double Thrombosis- Interesting Case of Polycythemia Vera
Subashini Subramanian1, Siva Ranganathan Green2
1 Postgraduate, Department of General Medicine, Mahatma Gandhi Medical College and Research Institute, Pondicherry, India.
2 Associate Professor, Department of General Medicine, Mahatma Gandhi Medical College and Research Institute, Pondicherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Siva Ranganathan Green, Mahatma Gandhi Medical College and Research Institute, Pondicherry, India.
E-mail: srgreen@mgmcri.ac.in
Polycythemia vera is a myeloproliferative disorder which has a varied manifestation, one of it being venous thrombosis and arterial thrombosis which significantly contributes to the mortality and morbidity. A 30-year-old male with history of deep vein thrombosis presented with history of headache and seizures and was diagnosed to have cortical venous sinus thrombosis with Magnetic Resonance Imaging (MRI) brain and complete blood count showed elevated haemoglobin and Packed Cell Volume (PCV). On evaluation patient was found to be positive for Polycythemia vera. We report this case with recurrent venous thrombosis which is a rare manifestation of polycythemia. Patient was managed with Adequate hydration, phlebotomy, Heparin, aspirin, Tablet Acetrom and Tablet. Hydroxyurea Patient was discharged after improving symptomatically.
Cortical venous sinus thrombosis, Deep vein thrombosis, Janus kinase (JAK)-2
Case Report
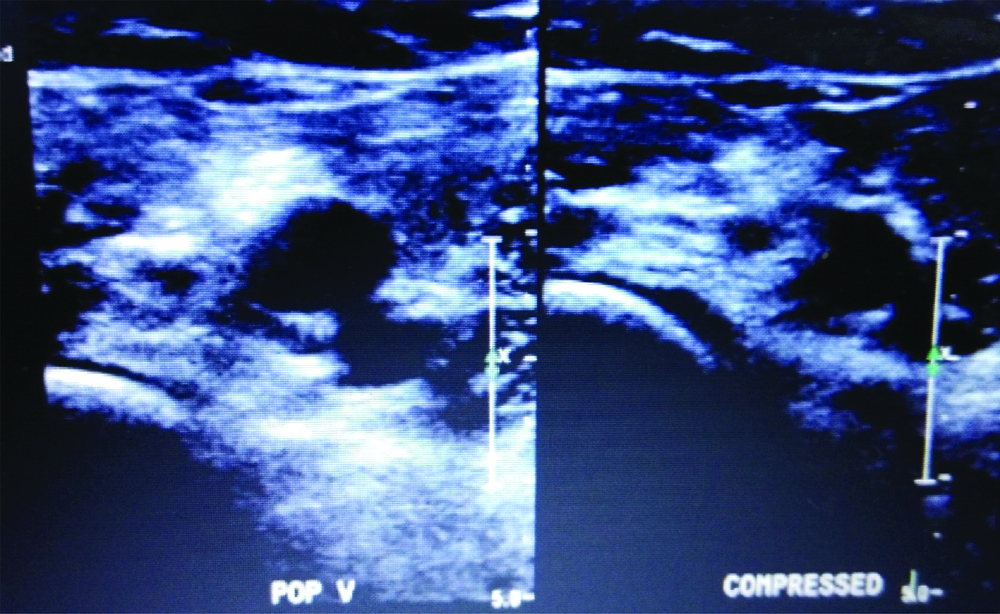
A 30-year-old male who had an episode of spontaneous right lower limb deep vein thrombosis nine months back [Table/Fig-1] without any significant past medical history and was treated with anticoagulants previously. Patient was evaluated for common hypercoagulable states like serum homocysteine, protein C, protein S, antithrombin deficiency and factor five laden mutation was done and found to be negative. Now, patient presented with history of two episode of unprovoked seizures and severe headache and multiple episode of vomiting for the past two days. On examination, patient was conscious, oriented to time place and person, with pulse rate -96/min and Blood pressure: 140/70 mmHg and systemic examination was normal. Fundus examination showed an established bilateral papilloedema. Routine blood investigations showed haemoglobin of 21.6 gm/dL, PCV of 61.5%, platelets was 4.56 lacs. Other investigations were within normal limit.
USG Doppler showing-right popliteal vein thrombosis.
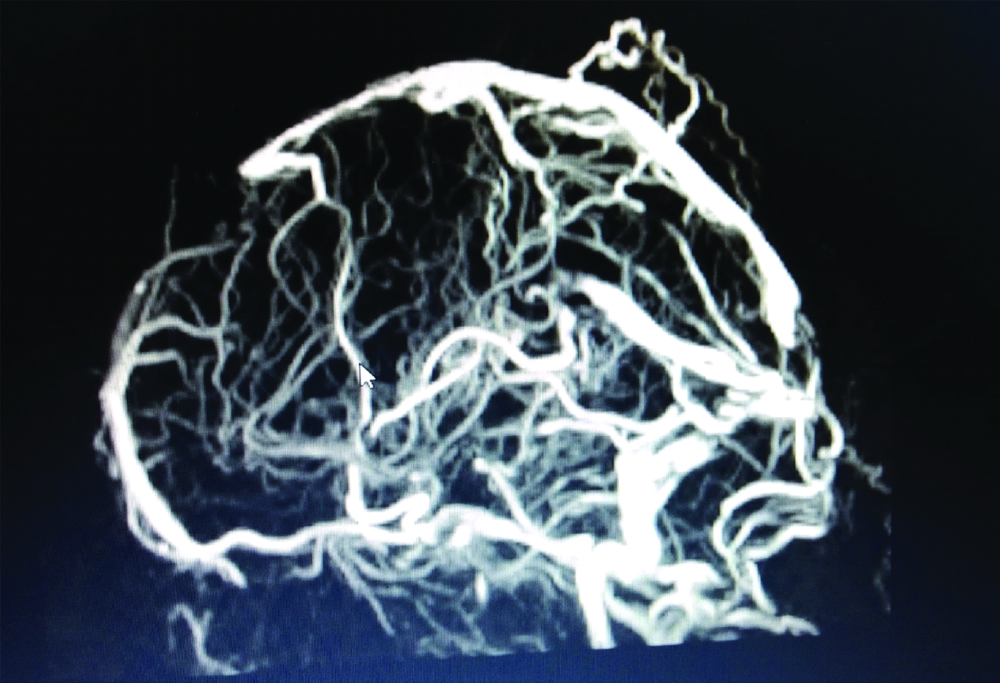
MRI brain was done with MR venogram which revealed a diffuse thrombosis of the both superficial and deep cortical venous system [Table/Fig-2]. Patient was started on systemic parenteral anticoagulation and bridged with oral vitamin k antagonist. Patient was well-hydrated, in spite of adequate hydration, patients haemoglobin and PCV were elevated with no other risk factor for secondary polycythemia and hence patient was worked-up for polycythemia vera. Serum erythropoietin was found to be low and Janus Kinase (JAK)-2 point mutation was positive. Patient was diagnosed to have polycythemia vera.
MRI brain-MRV showing cortical vein thrombosis.
Adequate hydration was done and weekly twice phlebotomy was done and low molecular weight Heparin 60 mg subcutaneous was started and aspirin 150 mg followed by oral anticoagulation, Tablet Acetrom and Tablet. Hydroxyurea 500 mg was also started. Weekly twice phlebotomy was done to maintain and target PCV of less than 45%. Patient improved symptomatically with no further seizures, no headache and hence was discharged with Tablet Acetrom 2 mg and Tablet Acetazolamide 250 mg twice daily.
Discussion
Polycythemia vera is one of the most common haematological disease encountered in haematological practice. Due to its varied clinical manifestations, polycythemia vera is less recognised unless it manifest with devastating complications. Among the complications vascular thrombosis is the most common complication with very high mortality and morbidity. Various mechanisms’ were attributed to the pathogenesis of thrombosis in polycythemia vera [1]. Arterial thrombosis was about 50-60% and most common ones being stroke, myocardial infarction and also peripheral vascular disease. The remaining were venous thrombosis predominantly the cerebral venous sinuses, deep vein thrombosis and also splenic vein thrombosis [2]. In present case, both events were venous thrombosis which were deep vein thrombosis first and cortical venous sinus thrombosis. MRI brain is the preferred investigation of choice for cortical venous sinus thrombosis as there will be an abnormal absence of flow void in T2 and T1 weighted images and also MR Venography shows filling defects [3]. The common presenting manifestations were headache, seizures, focal neurological deficit and altered sensorium, the most common differential were arterial stroke, hypoglycaemia, migraine, meningitis and head injury [4]. The most common clinical manifestations of polycythemia vera were pruritus, headache, dizziness, blurring of vision, reddened face, unexplained weight loss, shortness of breath and clinical features secondary to thrombotic manifestations [2]. In present case, only the clinical features secondary to thrombosis in cortical venous sinus were present, isolated presentation with cortical venous thrombosis without any other manifestations is comparatively rare.
Policitemia GIS study and European Collaboration on Low-Dose Aspirin in Polycythemia Vera (ECLAP) study found that most of the time (64%) the thrombotic events precedes the diagnosis of polycythaemia vera [5]. Various mechanism were attributed for the thrombosis in polycythemia which were increased leucocyte-platelet aggregation, overexpression of activation and adhesion molecules and endothelial activation [6].
Various risk factors were associated with the increased incidence of thrombosis, most common among them were in age more than 65 years, prior history of thrombosis, total leucocyte count more than 11000/cubic mm. Thrombocytosis and increased inflammatory markers like C-reactive protein were the common factors which when present increases the risk of thrombosis [7]. In present case, patient was young which is usually not associated with thrombosis, but he had thrombocytosis and prior history of thrombosis. Cytoreduction therapy and treatment with hydroxyurea significantly reduces the incidence of recurrent thrombosis in patients with polycythemia that to who were having a JAK2 V617F mutation. In present case patient was also JAK2 positive and hence started on hydroxyurea.
As per recent guidelines all patients with polycythemia vera and cortical venous thrombosis should be treated with long term anticoagulation and also with cytoreduction therapy. Low molecular weight heparin should be preferred followed by oral vitamin k antagonist. Recently increasing use of newer oral anticoagulation has been on the rise but the clinical trial based evidence is not yet fully established [8]. The role of low dose aspirin and JAK2 inhibitors in patients with polycythemia has also not been fully analysed and not routinely recommended [9].
Conclusion(s)
Polycythemia vera is one of the most common myeloproliferative disorder encountered in clinical practice. Among its various manifestations, thrombosis which is not to be forgotten and it has its own mortality and morbidity. Both arterial and venous thrombotic events are common. An effective diagnosis and treatment will drastically improve the clinical outcome.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Feb 04, 2020
Manual Googling: Apr 06, 2020
iThenticate Software: Apr 21, 2020 (11%)
[1]. Griesshammer M, Kiladjian JJ, Besses C, Thromboembolic events in polycythemia veraAnn Hematol 2019 98(5):1071-82.10.1007/s00277-019-03625-x30848334 [Google Scholar] [CrossRef] [PubMed]
[2]. Kaifie A, Kirschner M, Wolf D, Maintz C, Hänel M, Gattermann N, Bleeding, thrombosis, and anticoagulation in myeloproliferative neoplasms (MPN): Analysis from the German SAL-MPN-registryJ Hematol Oncol 2016 9:1810.1186/s13045-016-0242-926944254 [Google Scholar] [CrossRef] [PubMed]
[3]. Walecki J, Mruk B, Nawrocka-Laskus E, Piliszek A, Przelaskowski A, Sklinda K, Neuroimaging of Cerebral Venous Thrombosis (CVT)- Old dilemma and the new diagnostic methodsPol J Radiol 2015 80:368-73.10.12659/PJR.89438626251677 [Google Scholar] [CrossRef] [PubMed]
[4]. Alvis-Miranda HR, Castellar-Leones SM, Alcala-Cerra G, Moscote-Salazar LR, Cerebral sinus venous thrombosisJ Neurosci Rural Pract 2013 4(4):427-38.10.4103/0976-3147.12023624347950 [Google Scholar] [CrossRef] [PubMed]
[5]. Gruppo Italiano Studio PolicitemiaPolycythemia Vera: The natural history of 1213 patients followed for 20 yearsAnn Intern Med 1995 123(9):656-64.10.7326/0003-4819-123-9-199511010-000037574220 [Google Scholar] [CrossRef] [PubMed]
[6]. Landolfi R, Cipriani MC, Novarese L, Thrombosis and bleeding in polycythemia vera and essential thrombocythemia: Pathogenetic mechanisms and preventionBest Practice & Research Clinical Haematology 2006 19(3):617-33.10.1016/j.beha.2005.07.01116781491 [Google Scholar] [CrossRef] [PubMed]
[7]. Martin K, Risk factors for and management of mpn-associated bleeding and thrombosisCurr Hematol Malig Rep 2017 12(5):389-96.10.1007/s11899-017-0400-328948496 [Google Scholar] [CrossRef] [PubMed]
[8]. McMullin MFF, Mead AJ, Ali S, Cargo C, Chen F, Ewing J, A guideline for the management of specific situations in polycythaemia vera and secondary erythrocytosisBritish Journal of Haematology 2019 184(2):161-75.10.1111/bjh.1564730426472 [Google Scholar] [CrossRef] [PubMed]
[9]. Bose P, Verstovsek S, JAK2 inhibitors for myeloproliferative neoplasms: What is next?Blood 2017 130(2):115-25.10.1182/blood-2017-04-74228828500170 [Google Scholar] [CrossRef] [PubMed]