There has been an increase over the past decades to combat recording Health-Related Quality of Life re-HRQoL certified patient components, especially chronic diseases due to lack of traditional results, often focusing on biological and physiological consequences, in capturing the impact of interventions on HRQoL of patients [1,2]. DM is well known for its metabolic influences, acute and chronic complications and impact on Quality of Life (QoL) [3]. It is considered one of the most common chronic disorders in countries, and its popularity was increasing due to lifestyle changes that led to physical inactivity and obesity. It was believed that diabetes affected 285 million adults (20-79 years) worldwide in 2010, and this figure would enlarge to 439 million adults by 2030 [4]. The DM commonness in the world’s countries showed a wide range; 4.6% in Yemen, 9.3% of the total US population, and 10.7% in the United Arab Emirates. Regionally, Africa had the lowest rate (2.4%), while the inflating prevalence of DM is bargained for Southeast Asian countries and Sub-Saharan Africa [5].
Diabetes was associated with the higher risk of some macro and micro-vascular complications. As a consequence, these complications led to the fatality rate of diabetic patients, twice higher than non-diabetic individuals of similarly age group. Furthermore, diabetic patients with complications had lower HRQoL than patients without complications [2]. The information about the patient’s HRQoL was commonly gathered using ‘Patient-Reported Outcome Measures’ (PROMs) [1,6]. These involved the patient responding a number of questions on the topic such as physical functioning, social role, and mental wellbeing, and may include both generic and disease-specific questions [1].
Diabetes is a life-long disease and a constantly rising incidence of diabetes had drawn the attention of the community healthcare with effective managing programmes [7]. These studies aimed to improve the HRQoL of diabetic people by providing proofs for informed decision-making. However, the differences of the research questions, tools, and population on these individual studies made the difficulty for reaching the clear answer applicable for policy-making purposes. In response to this, conducting a systematic review of individual studies to make the available evidence more accessible for policy-making was common in medical researches [2].
In this course, the current systematic review was conducted to describe the latest available information about HRQoL in people with diabetes in the Association of Southeast Asian Nations (ASEAN). Specifically, this review aimed to investigate how HRQoL was measured in the ASEAN diabetic population, what were the main methodological flaws of these studies, and which factors were mainly associated with HRQoL in people with diabetes.
Materials and Methods
Literature Search
A systematic literature inspection was severally realised in January 2018 to critique the studies which analysed the HRQoL of diabetic people in ASEAN. The results of this document search were verified and updated independently in February 2018. Studies published in January 2018 and earlier have been included in the review. National and International databases (Tạp chí y học Thành phồ Hồ Chí Minh (Y hoc Thanh Pho Ho Chi Minh), Tạp chí y học dụ’ phòng Viêt Nam (Vietnam Journal of Preventive Medicine), Tạp chí y học thụ’c hành (Journal of Practical Medicine), Pubmed, Medline, Web of Science, CINAHL, Scopus, PsycINFO, ERIC, Google and Google Scholar [8,9]) were searched through following search terms: “diabetes”, “quality of life”, “đái tháo sống (diabetes)” and “chắt lu’o’ng cuĉc sống (quality of life)”. The Vietnam journals were chosen because this research needs an overview of the QOL of diabetics in previous studies in ASEAN, especially in Vietnam.
This study followed the PRISMA guidelines [10].
Selection of Studies
Inclusion criteria: 1) the study assessed the diabetic patient HRQoL; 2) the investigation data described the population HRQoL; 3) the research was not a systematic reviewer; 4) the research has been published in Vietnamese or international journals; 5) the study object is the population of ASEAN countries.
Exclusion criteria: 1) the research did not judge the HRQoL of diabetic people; 2) the study did not dissect any data about the HRQoL of the study population (e.g., the study was related to instrument development in diabetic patients); 3) the review articles; 4) the study was not published in journals (e.g., conference abstracts and dissertations); 5) the study was not applied to the populations of ASEAN countries.
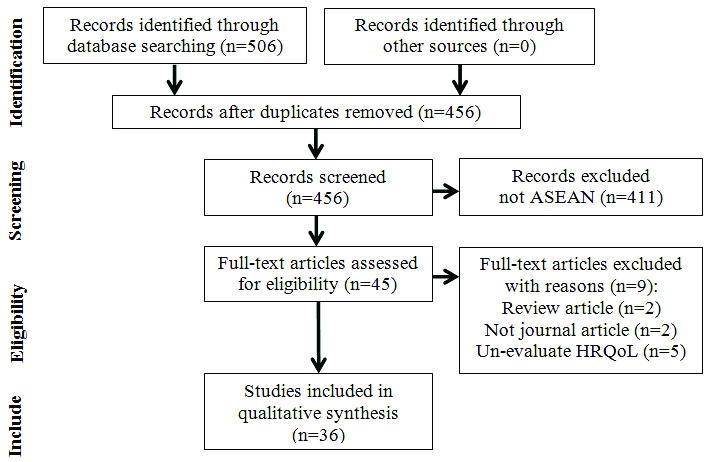
The initial search resulted in 506 documents. After excluding replicas and non-relevant studies, 45 articles were determined for full-text examination. The reference lists of these 45 documents were manually searched. Totally, 36 publications were included for the review [Table/Fig-1]. In cases where multiple publications were produced from a single study, the paper with the most comprehensive data was included.
Flow diagram of the literature search.
Data withdrew from the selected studies is as follows: publication year, country and the investigating year, study design, sample size, type of diabetes, the samples’ age range, diabetic duration, the HRQoL measurement tool, the HRQoL main predictors, and statistical analysis methods.
Results
General Characteristics
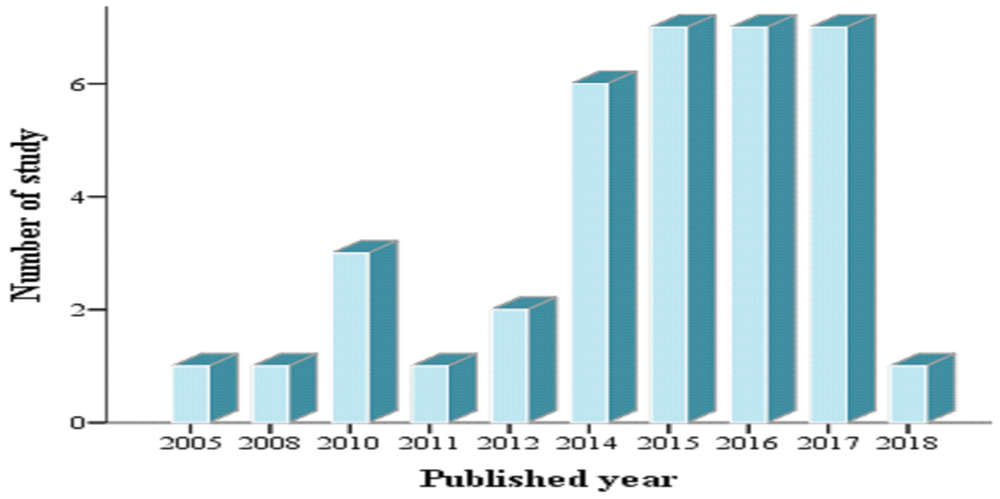
The features of the 36 eligible studies [3,5,7,11-43] for this criticism are demonstrated in [Table/Fig-2]. The first inquiry in Singapore was proclaimed in 2005, in 2008, however, a follow-up analysis was declared in Thailand. Then there were few publications per year on the topic, until 2013, when seven articles were published in 2015, 2016 and 2017 [Table/Fig-3].
Characteristics of the studies included in the review [3,5,7,11-43].
| First author (Published year) | Country | Language | Data year | Study design | Sample characteristics | HRQoL Instrument |
|---|
| Type of diabetes (%) | Sample size | Age range | Female (%) | Diabetes duration (mean) | |
|---|
| Perwitasari DA et al., (2017) [42] | Indonesia | English | 2017 | Cross-sectional | Type 2 (100) | 86 | >18 | 57 | 7.31 | EQ-5D |
| Perwitasari DA and Urbayatun S (2016) [37] | Indonesia | English | Not mention | Cross-sectional | Type 2 (100) | 65 | NA | 52.3 | NA | DQLCTQ |
| Faridah IN and Dewintasari V (2017) [38] | Indonesia | English | 2016 | Cross-sectional | Type 2 (100) | 52 | >18 | 75 | NA | DQLCTQ |
| Faridah IN et al., (2017) [39] | Indonesia | English | 2017 | Cross-sectional | Type 2 (100) | 80 | >18 | 65 | 4.82 | EQ-5D |
| Alfian SD et al., (2016) [40] | Indonesia | English | 2014 | Cross-sectional | Type 2 (100) | 91 | ≥18 | 71 | NA | D-39 |
| Andayani TM et al., (2010) [41] | Indonesia | English | 2007-2008 | Observational prospective | Type 2 (100) | 115 | NA | 49.57 | 12.53 | DQLCTQ |
| Daher AM et al., (2016) [5] | Malaysia | English | Not mention | Cross-sectional | Type 2 (100) | 256 | 30-80 | 58.6 | NA | ADDQoL-18 |
| Daher AM et al., (2015) [3] | Malaysia | English | 2012 | Cross-sectional | Type 2 (100) | 256 | 30-80 | 58.6 | NA | ADDQoL-18 |
| Chew B-H (2015) [27] | Malaysia | English | 2012-2013 | Cross-sectional | Type 2 (100) | 700 | ≥30 | 52.8 | 6.5 | WHOQOL-BREF |
| Chew B-H et al., (2015) [32] | Malaysia | English | 2012-2013 | Cross-sectional | Type 2 (100) | 700 | ≥30 | 52.8 | NA | WHOQOL-BREF |
| Imran KM et al., (2010) [33] | Malaysia | English | Not mention | Cross-sectional | Type 2 (100) | 150 | ≥18 | 42 | NA | SF-36 |
| Low LL et al., (2014) [34] | Malaysia | English | 2012-2013 | Cross-sectional | Type 2 (100) | 12 | 50-62 | 58.33 | 8.7 | In-depth interviews |
| Bujang MA et al., (2017) [35] | Malaysia | English | Not mention | Cross-sectional | Type 2 (100) | 290 | ≥18 | 49 | NA | DQOL |
| Manan MM et al., (2014) [36] | Malaysia | English | 2012 | Cross-sectional | Type 2 (100) | 179 | ≥60 | 54.7 | 10.89 | PAID |
| Butt M et al., (2016) [7] | Malaysia | English | 2013-2014 | RCT | Type 2 (100) | 73 | NA | 57.6 | NA | EQ-5D-3L |
| Tan MC et al., (2014) [11] | Malaysia | English | 2010-2011 | Cross-sectional | Type 2 (100) | 313 | 30-78 | 52.1 | 10.1 | 15D |
| Goh SG et al., (2015) [12] | Malaysia | English | Not mention | Cross-sectional | Type 2 (100) | 451 | NA | 37.9 | 14 | AsianDQOL |
| Goh SG et al., (2015) [13] | Malaysia | English | Not mention | Cross-sectional | Type 2 (100) | 647 | >18-80 | 34.6 | 4 | AsianDQOL |
| Azmi S et al., (2018) [14] | Malaysia | English | 2015 | Cross-sectional | Type 2 (100) | 816 | ≥18 | 43.8 | 8.9 | SF-36 |
| Hasan SS et al., (2014) [15] | Malaysia | English | Not mention | Case-control | Type 2NDM | 640 | 35-75 | 100 | NA | MENQOLSF-12 |
| Samah S et al., (2016) [16] | Malaysia | English | 2015 | Cross-sectional | Type 2 (100) | 202 | ≥18 | 70.8 | 7 | DQoL-BCI |
| Hasan SS et al., (2016) [17] | Malaysia | English | 2012-2013 | Case-control | Type 2NDM | 640 | 27-70 | 100 | NA | MENQOL |
| Jannoo Z et al., (2015) [19] | Malaysia | English | Not mention | Cross-sectional | Type 2 (100) | 596 | >18 | 47.6 | 9.66 | ADDQoL-19 |
| Jannoo Z et al., (2017) [18] | Malaysia | English | Not mention | Cross-sectional | Type 2 (100) | 497 | 25-85 | 46.3 | 9.97 | ADDQoL-19SF-36 |
| Wee HL et al., (2005) [20] | Singapore | English | 1998-1999 | Cross-sectional | Type 1Type 2 | 5,224 | 21-65 | 48.9 | NA | SF-36SF-6D |
| Quah JH et al., (2011) [21] | Singapore | English | 2009 | Cross-sectional | Type 2 (100) | 699 | >21 | 55.5 | NA | EQ-5D |
| Co MA et al., (2015) [22] | Singapore | English | Not mention | Cross-sectional | Type 2 (100) | 213 | 21-64 | 36.6 | 9.3 | ADDQoL-19 |
| Man RE et al., (2016) [23] | Singapore | English | 2010-2013 | Cross-sectional | Type 1Type 2 | 390 | 22-78 | 29.7 | 11.5 | IVI |
| Shim YT et al., (2012) [24] | Singapore | English | 2009 | Cross-sectional | Type 2 (100) | 301 | ≥21 | 48.9 | NA | EQ-5DADDQoL-19 |
| Verma SK et al., (2010) [25] | Singapore | English | 2006-2007 | Cross-sectional | Type 1(3.6) Type 2 (96.5) | 537 | ≥21 | 41.3 | 10.2 | SF-36 |
| Maudrene TL et al., (2014) [26] | Singapore | English | 2011-2013 | Cross-sectional | Type 2 (100) | 212 | 21-65 | 37 | NA | WHOQOL-BREF |
| Riandini T et al., (2017) [43] | Singapore | English | 2014-2017 | Cross-sectional | Type 2 (100) | 160 | 40-79 | 41.9 | 13.37 | EQ-5D-5L |
| Zhang XH et al., (2012) [28] | Singapore | English | Not mention | Cross-sectional | Type 1 (26.47)Type 2 (73.53) | 68 | 33-72 | 44.12 | NA | ADDQoL-19EQ-5DSF-6D |
| Wichit N et al., (2017) [29] | Thailand | English | Not mention | RCT | Type 2 (100) | 140 | ≥35 | 75.7 | 6 | SF-12 |
| Sakthong P et al., (2008) [30] | Thailand | English | 2007 | Cross-sectional | Type 2 (100) | 303 | 27-90 | 71 | 12.2 | EQ-5D |
| Hoang TN and Dao NTB (2014) [31] | Vietnam | Vietnamese | 2011 | Cross-sectional | Type 2 (100) | 200 | NA | 76.5 | 5.8 | SF-36 |
Number of study by year of publication.
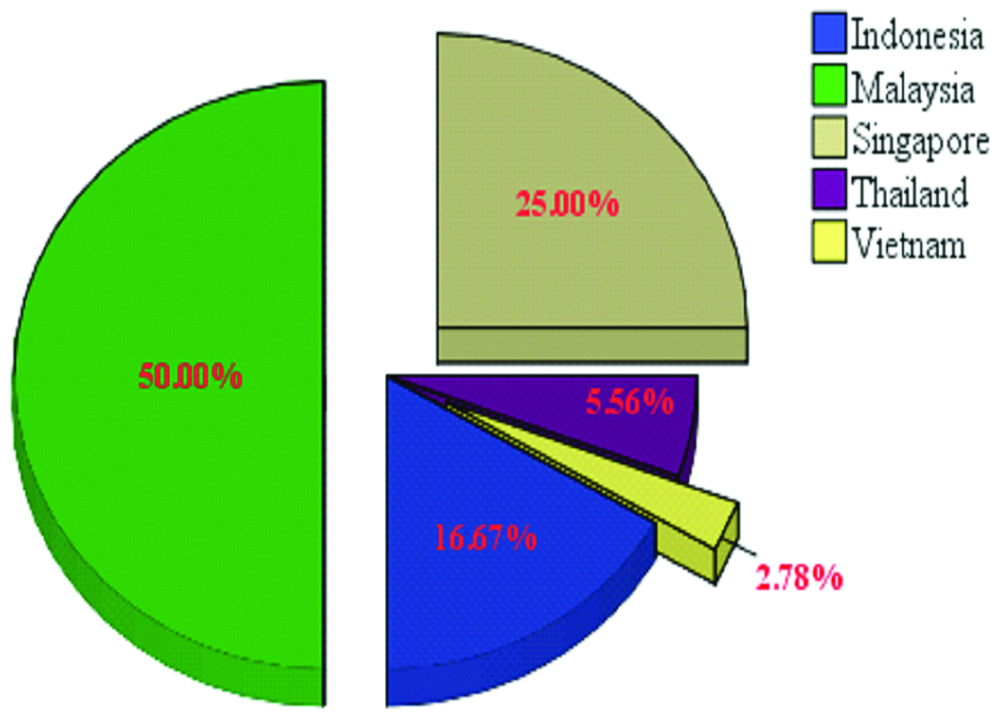
The HRQoL of diabetic people was elaborated in 5 of the 10 countries of the ASEAN. Among them, 18 out of 36 studies (50%) were conducted in Malaysia, while in Vietnam there was only one study (2.78%) [Table/Fig-4]. Sample sizes across the studies ranged from 12 to 5,224 participants. The majority of the studies (97.22%) were promulgated in an English language journal, only one professed in a Vietnamese journal. A cross-sectional design was the dominant style of the studies (n=31).
The proportion of study by country.
In terms of the diabetic type, 31 studies covered only type 2 Diabetic Mellitus, but no study has been done solely in people with type 1 diabetes. In the remaining studies, there were two combinations of type 2 diabetic and non-diabetic people in the sample. The age of participants ranged from 18 to 90-year-old. In most studies, women constituted the plurality of the study participants, specifically, two researches only analysed female patients. The mean duration of diabetic patients ranged from 4 to 14 years [Table/Fig-2].
Health-Related QOL Instrument
Regarding the measuring device used for the HRQoL evaluation of the study population, 17 different implements were used in the studies. Fourteen studies used a generic measure, two research used two generic tools, 16 investigations employed a disease-specific utensil and three studies applied both generic and disease-specific devices, one analysis used two generic and one specific questionnaire. The EQ-5D was used in 8 researches. The SF-36 was employed in 7 papers. The ADDQoL-19 was applied by 5 studies; DQLCTQ and WHOQOL-BREF were exerted by 3 studies; SF-12, SF-6D, ADDQoL-18, AsianDQOL, and MENQOL were utilised by 2 studies; and each of the others habituated one study [Table/Fig-5].
PROMs used in eligible studies.
| Instrument | Type | Domains/Subscales | Studies |
|---|
| 15D (15 dimensions instrument) | Generic | 15 dimensions | [11] |
| - Mobility- Vision- Hearing- Breathing- Sleeping- Eating- Speech- Elimination | - Sexual activity- Usual activities- Metal function- Discomfort and symptoms- Depression- Distress- Vitality |
| EQ-5D (EuroQOL-5D Health Utility Index) | Generic | EQ-5D- Anxiety/depression (1)- Mobility (1)- Pain/discomfort (1)- Self-care (1)- Usual activities (1) | EQ-thermometer- Global health (1) | [7] [39] [42] [21] [43] [30] [24] [28] |
| SF-12 (MOS 12-item Short Form Health Survey) | Generic | - Bodily pain (1)- Energy/Vitality (1)- General health (1)- Mental health (2) | - Physical functioning (2)- Role limitation-emotional (2)- Role limitation-physical (2)- Social functioning (1) | [29] [15] |
| SF-36 (MOS 36-item Short Form Health Survey) | Generic | 36 items in 8 domains | [14] [31] [18] [33] [21] [25] [20] |
| - Bodily pain (2)- General health (5)- Mental health (5)- Physical functioning (10) | - Vitality (4).- Role limitation-emotional (3)- Role limitation-physical (4)- Social functioning (2) |
| SF-6D (MOS 6-item Short Form Health Survey) | Generic | Six dimensions | [20] [28] |
| - Bodily pain (1)- Energy/Vitality (1)- Mental health (1) | - Physical functioning (1)- Role limitation (1)- Social functioning (1) |
| WHOQOL-BREF (World Health Organization QOL Brief Questionnaire) | Generic | 26 items in 4 domains | [27] [32] [26] |
| - Physical health (7)- Psychological (6) | - Social relationships (3)- Environment (8) |
| ADDQoL-18 (Audit of Diabetes-Dependent QOL-18) | Specific | 18 items | [3] [5] |
| - Freedom to eat- Working life- Living conditions- Family life- Freedom to drink- Finances- Worries about the future- Self-confidence- Motivation | - Physical activity- Holidays/leisure activities- Ease of travelling- Friendships, social life- Sex life- Physical appearance- Reliance on Others- Reaction of society- Enjoyment of food |
| ADDQoL-19 (Audit of Diabetes-Dependent QOL-19) | Specific | 19 items | [22] [18] [19] [24] [28] |
| - Freedom to eat- Working life- Living conditions- Family life- Freedom to drink- Financial situation- Feelings about the future- Self-confidence- Motivation | - Physical activities- Holidays- Leisure activities- Personal life- Travel- Social life- Sex life- Physical appearance- Reliance on Others- Reaction from others |
| AsianDQOL (Asian Diabetes QOL Questionnaire) | Specific | 21 items in 5 dimensions | [12] [13] |
| - Financial (5)- Energy level (3)- Memory (4) | - Relationship (3)- Diet (6) |
| D-39 (Diabetes 39) | Specific | 39 items | [40] |
| - Anxiety and worry (4)- Social and peer burden (5)- Sexual functioning (3) | - Energy and mobility (15)- Diabetes control (12) |
| DQLCTQ (Diabetes QOL Clinical Trial Questionnaire) | Specific | 57 items in 8 domains | [41] [38] [37] |
| - Physical function- Energy/fatigue- Health distress- Mental health- Satisfaction (DQOL) | - Treatment satisfaction- Treatment flexibility- Frequency of symptoms- 1 global health question- 1 transition question |
| DQOL (DiabetesQOL) | Specific | - Worries- future effects of diabetes (4)- Worries- social/vocational issues (7) | - Impact of treatment (20)- Satisfaction with treatment (15) | [35] |
| DQoL-BCI (Diabetes QOL-Brief Clinical Inventory) | Specific | 15 items in 4 dimensions: | [16] |
| - Satisfaction- Impact | - Social worry- Vocational worry |
| IDI (In-depth interviews) | Specific | A deeper understanding of the patients | [34] |
| - Reaction to diagnosis- Their experiences with the management of T2DM | - Perceptions towards T2DM- How these affect their QoL. |
| IVI (Impact of Visual Impairment questionnaire) | Specific | 28 items in three subscales | [23] |
| - Mobility and independence (11) | - Reading and accessing information (9)- Emotional well-being (8). |
| MENQOL (Menopause-Specific QOL) | Specific | 29 items in 4 dimensions | [15, 17] |
| - Vasomotor aspects (3)- Psychosocial aspects (7) | - Physical aspects (16)- Sexual aspects (3) |
| PAID (Problem Areas in Diabetes Scale) | Specific | 20 items | [36] |
HRQoL in Diabetic and Non Diabetic Patients
Two studies, which inspected the consequence of diabetes on HRQoL, were specifically on menopausal women [Table/Fig-5]. These compared HRQoL in people with and without diabetes and recorded the negative integration of type 2 diabetes on the HRQoL of menopausal women.
Diabetes-Related Complications
Seventeen studies observed the forces of diabetes-related complications on the HRQoL in diabetic patients. These researchers perceived that these complications had the pessimistic impacts on the HRQoL of diabetic patients.
Other Predictors of HRQOL
The joinder between HRQoL and some demographics, socioeconomic and clinical predictors were probed in twenty-nine studies. Among them, there were eighteen studies which discovered a disadvantage fusion between age and HRQoL; however, seven investigations showed that these were non-significant. Moreover, 22 studies assessed the gender and HRQoL of which 12 articles showed that females had a lower HRQoL than males, four studies showed the gender-related QoL of diabetic patients was lower and others expanded non-significant. Also, there was the difference of HRQoL between ethnicities which were demonstrated in 12 papers. In addition, there were four researches which compared religion and HRQoL, but only three studies were significant.
Fourteen studies only described the relationship between socioeconomic (including income, education, employment) and HRQoL while there were seven investigations which showed that the better the socioeconomic status, the better the HRQoL. Others discussed why the QoL of diabetes were not improving. The marital status of diabetics was analysed in 10 studies, and found to be unrelated to the HRQoL of diabetic people. However, two researches showed that the size of the family touched on the HRQoL of a diabetic, and it improved if they lived in a large house.
People with lower HbA1c generally have a higher HRQoL (this showed in 16 studies [3,5,7,11,13,14,16,19,21,23,25,26,33,35,38,41]. There was only one study [20] which claimed negative interrelations between blood pressure and HRQoL. Similarly, a study [11] confirmed that blood lipid decreased the QoL of diabetic patients. In 8 studies [7,11,22,23,29,30,32,36], the lower level of HRQoL was found among people who had the higher BMI. Eight studies instituted that there were negative association between HRQoL and diabetic duration, four papers reported the unrelated. In general, there were thirteen investigations [3,5,7,11-13,18,22,25,28,32,37,40] which analysed the association between treatment and HRQoL which expanded to a mixed result as the major research found that HRQoL improved; however, in one study [21], diet didn’t change the HRQoL, during treatment with insulin there were the lower decrease in HRQoL than with oral treatment, but the combined treatment showed the best improvement on HRQoL. In addition, in the four studies [36-38,42], the therapy adherence increased the HRQoL.
Discussion
To our knowledge, this was the first time; the current study had reviewed the results of 36 identified studies examining HRQoL among ASEAN diabetic patients. The findings of this review described that generally, diabetic people had worse HRQoL than their healthy counterparts. In addition, the conclusions indicated that diabetes-related complications had significantly pessimistic impact on HRQoL among diabetic patients in ASEAN countries. In general, the associations between covariates and HRQoL in the reviewed ASEAN studies were in line with their international twins.
The reviewed studies suffered from major methodological and reporting flaws which affected the quality of the discovers and limited their validity and generalisability [7,11,14,19,21,25,26,31,36-38,40-42,44,45]. The reviewed investigations mainly applied the non-random sampling methods, which selected the clinics [7,11,14,19,25,31,36-38,40-42,44,45], leading to possible selection bias. Moreover, calculation of sample size was unclear (a convenience sample [34] in the plurality of the studies. While the most studies were observational (only two randomised controlled trials [7,29], the univariate analysis was used for data analysis and the minimum effort was made to control any imbalance in the covariates leading to potential confounder and selection biases. Among the studies which employed multivariate analysis, some of the main confounding factors (such as diabetes-related complications and duration of diabetes) were not controlled, raising the possibility of confounder bias. In addition, these studies didn’t explain their limitations adequately and did not comment on the potential biases in their reported results. Although the generic tools were used more than specific tools, the limitations of these tools in capturing HRQoL of diabetic patients were not fairly explained. Moreover, several studies failed to validate the instruments before putting them to use in a new population (particularly, IDI instrument on Low LL et al., [34]) and only referred to application of the instruments in a diabetic population in other countries or a general population in the ASEAN countries (as MENQOL in the study of Hasan SS et al., 2014 [15] and 2016 [17]). It seems that similar to few other settings, ASEAN researchers have used the instruments applied in other studies without worrying about their content. However, there were three studies which checked questionnaire before analysis of the HRQoL of diabetic patient (two in Singapore [26,28] and one in Malaysia [12].
Limitation(s)
The results of the current review should be interpreted in the light of a few limitations. Firstly, although Vietnamese databases used in this review consisted of a majority of articles published nationally, there is a possibility that some studies may not be included in these databases. Secondly, as a wide range of instruments were used in the reviewed studies and the transparency of reported results was limited, it was not possible to apply statistical methods such as meta-analysis to test the association between the covariates and HRQoL.
Conclusion(s)
The growing interest in evaluating HRQoL among people with diabetes was observed in ASEAN over the last decade. The elicitations of this review showed that the HRQoL of diabetic people were lower than healthy people. The findings also indicated that better socioeconomic status, better control of risk factors and complications were associated with a better HRQoL among the patients with diabetes. Moreover, treatment adherence improved HRQoL. The reviewed studies suffer from major methodological and reporting flaws which limit the validity and generalisation of their findings.
Declaration: This work has been presented in Proceedings of ISER 151st International Conference, London, UK, 18th-19th August 2018 (http://www.worldresearchlibrary.org/up_proc/pdf/1852-153906830248-54.pdf).