Iliac Vein Compression- The May-Thurner Syndrome Diagnosed by CT Angiography
Shibani Mehra1, Mayank Choudhary2
1 Professor, Department of Radiodiagnosis, RML Hospital ABVIMS, Delhi, India.
2 Senior Resident, Department of Radiodiagnosis, RML Hospital ABVIMS, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shibani Mehra, C 1/36, SDA, Delhi, India.
E-mail: shibani.mehra@yahoo.in
Chronic venous insufficiency and venous ulcers are a frequent cause of morbidity in diabetic as well as non-diabetic patients. Pelvic veins can often be involved by thrombosis. Imaging with Doppler sonography is essential to diagnose venous thrombosis. However, pelvic vein compression by an adjacent coursing artery is an unusual cause of lower limb venous obstruction, limb swelling and non-healing ulcers. Diagnosis of iliac vein obstruction and identification of compression by the iliac artery requires radiological imaging, with CT angiography being the current favoured modality. Here, a case 23-year-old male presented with painless swelling of the left leg since three years duration with a venous ulcer on the lateral aspect of lower leg since two years. In order to ascertain the cause of pelvic iliac vein compression(as detected on Venous Doppler ultrasonography), Dual-phase thin-section abdominal and bilateral lower limb Computed Tomography (CT) Angiography with venography run were performed, which showed the right common iliac artery compressing the left common iliac vein at its origin Based on these imaging findings, a radiological diagnosis of May-Thurner syndrome was made which highlights that non-thrombotic occlusion of pelvic veins can be a cause of unilateral lower limb swelling and long standing venous ulcer.
Doppler sonography, Extrinsic pelvic vein compression, Left common iliac vein, Right common iliac artery
Case Report
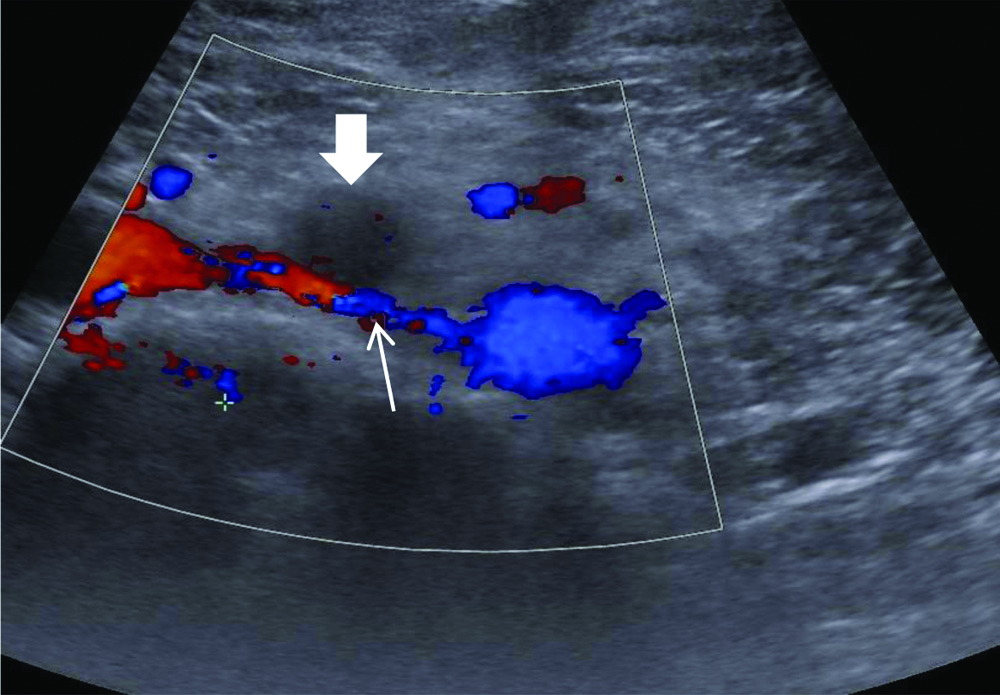
A 23-year-old male presented with painless swelling of the left leg since three years duration with a venous ulcer on the lateral aspect of lower leg since two years. There was no history of diabetes, smoking, or deep venous thrombosis. On venous Doppler ultrasonography (US) the superficial and deep veins of lower limb were found to be normal in caliber with normal patency and waveform. However, the left common iliac vein was seen compressed at the origin, and was significantly narrowed in diameter of its course along with attenuated ipsilateral external iliac vein [Table/Fig-1a,b]. In order to ascertain the cause of pelvic iliac vein compression, Dual-phase thin-section (section thickness, 1.25 mm) abdominal and bilateral lower limb Computed Tomography (CT) Angiography with venography run were performed on a 128 slice MDCT scanner (Siemens Somatom Definition Flash), acquiring images below infrarenal aortic level. A power injector was used to administer intravenous iodinated contrast through a 20 gauge catheter in the right antecubital vein. The total amount of contrast medium used was 2 mL/kg with a flow rate of 5.5 mL/sec to ensure good opacification of venous system. Images were acquired within seconds of injection, in the arterial phase, and then in the venous phase after a 120 second delay. Three-dimensional volume rendered and Maximum Intensity Projection (MIP) images were evaluated.
On ultrasound grey scale image showing right common iliac artery (open arrow) causing compression of left common iliac vein (arrow) at its origin and significantly narrowed distal most left common iliac vein (arrow).

Colour doppler image showing right common iliac artery (open arrow) causing compression of left common iliac vein (arrow) at its origin and significantly narrowed distal most left common iliac vein (arrow).
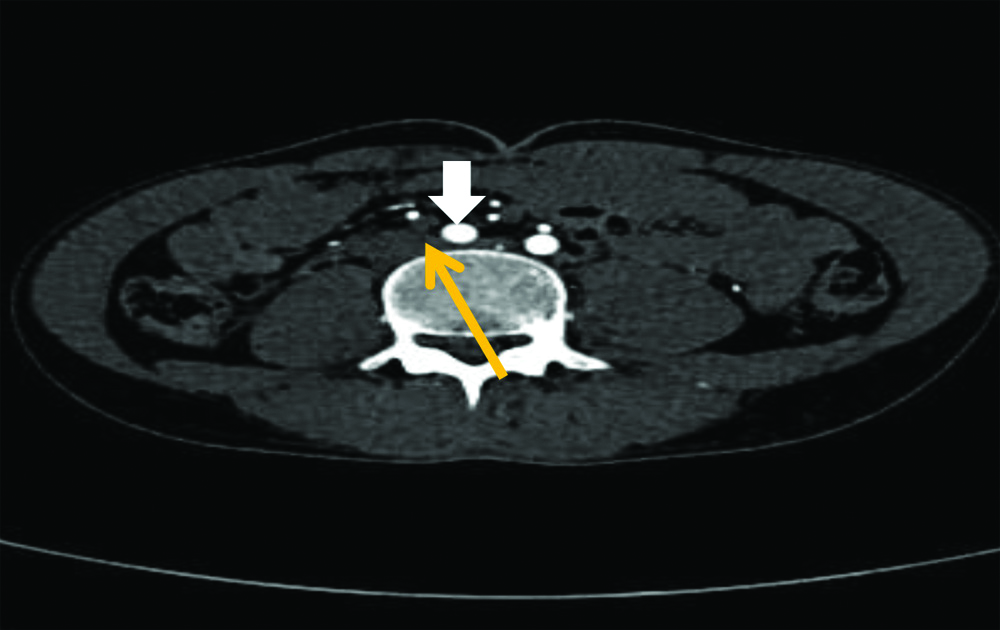
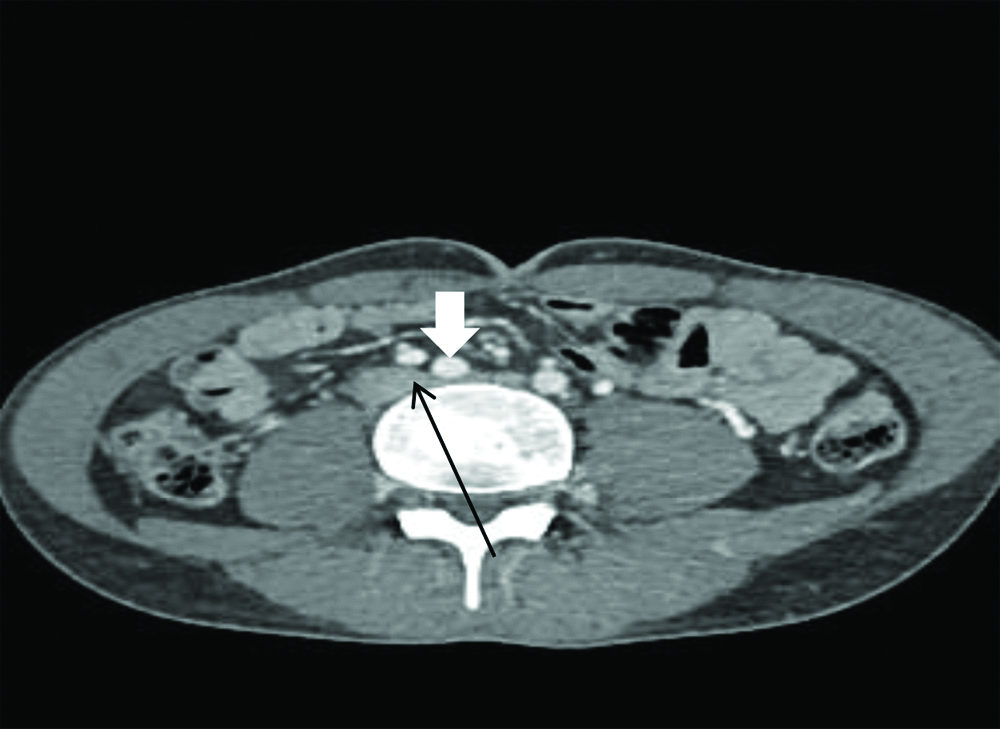
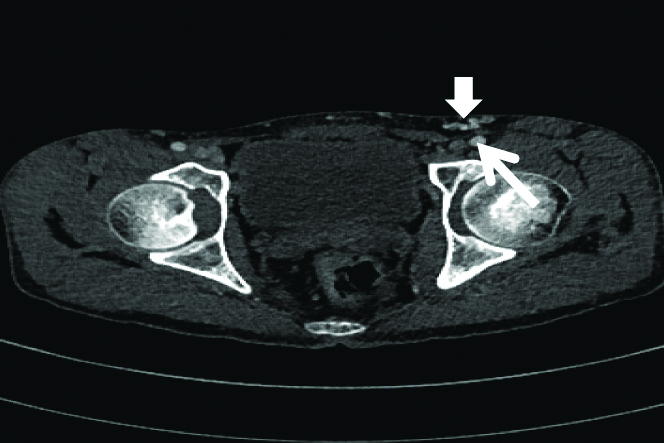
CT Angiography Images demonstrated normal anatomy of aortic bifurcation and lower limb arteries. However, the pelvic vessels were seen to be abnormal in course and caliber. The right common iliac artery was seen compressing the left common iliac vein at its origin [Table/Fig-2a,b]. The diameter of left common iliac vein was significantly narrowed, with marked narrowing of the left external iliac vein which was seen becoming normal in caliber diameter, just before crossing the inguinal ligament with an adjacent collateral vessel seen supplying it [Table/Fig-3]. Multiple venous collateral channels were seen in left lower abdominal wall and left inguinal region. The lower limb venous system was normal. Based on imaging findings of a pelvic artery causing compression of the accompanying vein, a radiological diagnosis of May-Thurner syndrome was made. The patient was taken-up for surgery subsequent to the radiological diagnosis, with the purpose of circumventing the iliac vein occlusion, and a saphenous vein graft was placed connecting iliac vein to the ipsilateral common femoral vein. On clinical follow-up after six weeks of the bypass procedure, the venous ulcer and lower limb swelling had both disappeared.
CT angiography axial image showing right common iliac artery (open arrow) causing compression of left common iliac vein (yellow arrow) at its origin.
CT venography axial image showing right common iliac artery (open arrow) causing compression of left common iliac vein (black arrow) at its origin.
CT venography axial image showing inguinal venous collaterals (open arrow) and left external iliac artery (white arrow).
Discussion
May-Thurner syndrome is caused by compression of the left common iliac vein by the right common iliac artery as it passes over the vein [1]. This unusual venous system disorder characterised by iliac vein compression causing stasis in venous flow because of the intimal changes was first described by May R and Thurner J in 1957 in cadavers [2]. The reason behind the compression of iliac vein in the pelvis by the artery could be the course of the right common iliac artery as it crosses the left common iliac vein. May R gave the hypothesis that due to proximity of the vein and the artery at the crossing-over point, transmitted arterial pulsations which cause vessel walls to rub against each other, leading to chronic mural irritation which results in proliferation of the endothelium [2]. The condition has also been described as the iliac compression syndrome or Cockett syndrome and another explanation given for it is formation of adhesions or bands between the anterior and posterior vessel walls [3]. This phenomenon of venous compression is akin to the nut cracker syndrome described with superior mesenteric artery compression.
This syndrome is an uncommon cause of venous obstruction in the lower extremity and can be seen in 2%-5% of patients who undergo evaluation for lower extremity venous ulcers [4]. This peculiar form of compression is mostly left sided, is seen more often in females in their second to third decade, and pregnancy is often the triggering factor. Non-thrombotic venous occlusion is the basic pathogenesis of this entity, and is better considered an anatomic variant rather than pathology.
The overlying right common iliac artery, due to its anatomic proximity, induces a partial obstruction of the iliac vein coursing below it, firstly by mechanical compression of the vein against the vertebrae, as it crosses over; and secondly by inducing a reactive intimal hypertrophy which results from development of shear stress between the anterior and posterior vein walls, due to presence of constant arterial pulsations [5]. Pelvic vein compression/occlusion can be intrinsic or extrinsic in aetiology. Intrinsic cause of pelvic vein occlusion is usually because of thrombotic occlusion subsequent to ante-grade extension of thrombus from the deep veins of the lower limb or due to retrograde extension of an Inferior Vena Cava (IVC) thrombus. Development of thrombus within the pelvic veins primarily is seen in association with hypercoagulable conditions. On the other hand, extrinsic iliac vein compression can be caused by non-thrombotic vein occlusion secondary to vein lumen obliteration from a duplicated IVC, iliac artery aneurysms, pelvic masses or pelvic metastatic lymphadenopathy [5,6]. In the present case, there was no pelvic mass, the IVC was patent with normal phasic flow and there was no deep vein thrombosis. Doppler ultrasound demonstrated the left common iliac vein to be narrow. However, CT angiography with indirect venography enabled identification of the right common iliac artery to be the cause of extrinsic compression of the adjacent iliac vein. Early diagnosis and intervention is important to prevent life threatening complications such as recurrent pulmonary embolism. Recurrent episodes of deep venous thrombosis and phlegmasia cerulea dolens are other vascular associations [5]. IVC obstruction can also be an associated complication. Most cases described in literature demonstrate deep vein thrombosis as the presenting feature or an association of venous compression [4,5]. However, present case is unusual as there was no associated deep vein thrombosis in the lower limbs nor in the pelvic veins, and moreover, the patient was a young male.
The diagnosis cannot be made clinically and radiology plays an important role in detecting the condition. The modality of choice in these patients is bilateral limb CT Angiography with indirect venography. MDCT technology has evolved significantly, allowing quick acquisition of large volume of data from a large area, the helical oversampling with motion reduction providing excellent spatial resolution to depict the vascular anatomy [6]. The vascular tree can be well evaluated in axial as well as coronal planes and MIP images can be generated. The diagnostic technique used till a decade ago for pelvic venous obstruction was an iliac phlebography performed via femoral vein access which could demonstrate vein compression as well as haemodynamics and severity of the compression by measuring the pressure gradient. Yet any extrinsic aetiology of compression could not be determined since catheter venography cannot provide extravascular information. The other major drawback of catheter venography is its invasive nature. CT Angiography is much more acceptable to patients because it is non-invasive in nature. This has led to CT angiography with sequential indirect venography becoming the “go to” and ‘sought after’ modality. MDCT angiography with venography has the advantage of demonstrating vascular anatomy, the abnormal anatomic relation of the artery and the vein, and extrinsic compression of vein by the artery [7]. Moreover identification of pelvic lymphadenopathy and masses causing pelvic vein compression is facilitated. MR angiography with venography is another alternative imaging option to evaluate the vascular tree and can detect aetiology of pelvic venous compression to be due to adjacent iliac artery, but its cost is a deterrent and it is less easily available.
Thin section CT angiography (3-5 mm) followed by CT venography is extremely useful to identify iliac artery compression to be the aetiology of venous ulcer, and to distinguish intrinsic thrombotic iliac vein occlusion from non-thrombotic extrinsic compressive occlusion [8]. Diagnostic CT imaging features of May-Thurner syndrome are a narrowed, obliterated or cord like irregular left common iliac vein with an overlying dilated or prominent right common iliac artery. A long segment obstruction with extension of compression to the ipsilateral external iliac vein can often be seen. Numerous pelvic or abdominal wall collaterals can be seen reinstating the supply from the lower limb veins in chronic obstruction [8]. The obstructed segment may be secondarily thrombosed. Depending on the site of maximum compression, three morphological types of May-Thurner syndrome are described lateral at the vein margin, central causing narrowing of the AP diameter of the vein, or partial obliteration of the vein segment resulting in fenestrated appearance. Further the condition has been classified into three types depending on the length of iliac vein compressed and severity of compression. Compression may be focal (Type 1) seen just at the cross-over point of right common iliac artery, may extend from the cross-over point to the external and internal iliac vein confluence, with luminal narrowing (Type II), or wherein entire left common iliac vein is markedly compressed and cord like (Type III) [8]. The IVC should be assessed in all patients to rule out associated caval obstruction [9].
Various interventional and surgical treatment options exist to relieve the venous compression in May-Thurner syndrome namely-placement of stent in the obstructed vein, angioplasty of the occluded vein segment called patch-angioplasty and even surgical relocation of the right common iliac artery behind either the left common iliac vein or behind the IVC. The palma cross-over is another vascular surgical technique wherein a temporary arteriovenous fistula is created to relieve the compression by bypassing the common femoral vein with the help of a contralateral saphenous vein graft [10]. The long-term success rate with the therapeutic maneuver using bypass graft has been reported to be 40%-88%. In case of thrombosis complicating the compressed iliac vein, catheter directed thrombolytic therapy is viable treatment recourse [11].
The clinical and radiological diagnosis of May-Thurner syndrome should be kept in mind when evaluating any patient between the 2nd and 4th decades of life with a history of persistent left lower extremity swelling, venous ulcers or deep venous thrombosis. The case being presented is unique as there was no association with DVT. Therefore, CT angiography is useful in evaluation of all suspected vascular aetiologies and must be included in clinical work-up.
Conclusion(s)
It is important for both clinicians and radiologists to be aware of this unusual cause of pelvic venous compression and CT angiography with acquisition of venography phase in the second run, must be advised in all non-diabetic patients presenting with long standing venous ulcers.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 21, 2019
Manual Googling: Feb 14, 2020
iThenticate Software: Apr 18, 2020 (13%)
[1]. Duran C, Rohatgi S, Wake N, Rybicki FJ, Steigner M, May-Thurner Syndrome: A case reportEurasian J Med 2011 43(2):129-31.10.5152/eajm.2011.2925610179 [Google Scholar] [CrossRef] [PubMed]
[2]. May R, Thurner J, The cause of the predominantly sinistral occurrence of thrombosis of the pelvic veinsAngiology 1957 8(5):419-27.10.1177/00033197570080050513478912 [Google Scholar] [CrossRef] [PubMed]
[3]. Cockett FB, Thomas ML, The iliac compression syndromeBr J Surg 1965 52(10):816-21.10.1002/bjs.18005210285828716 [Google Scholar] [CrossRef] [PubMed]
[4]. Wan-Ling MW, Tzeng WZ, Wu RW, Tsai WL, Chen MC, Lin PC, Comprehensive MDCT evaluation of patients with suspected May-Thurner syndromeAm J of Roentgenol 2012 199(5):W638-45.10.2214/AJR.11.804023096209 [Google Scholar] [CrossRef] [PubMed]
[5]. Cil BE, Akpinar E, Karcaaltincaba M, Akinci D, Case 76 May-Thurner SyndromeRadiology 2004 233(2):361-65.10.1148/radiol.233203015215516613 [Google Scholar] [CrossRef] [PubMed]
[6]. Fleischmann D, Hallett RL, Rubin GD, CT angiography of peripheral arterial diseaseJ Vasc Interv Radiol 2006 17(1):03-26.10.1097/01.RVI.0000191361.02857.DE16415129 [Google Scholar] [CrossRef] [PubMed]
[7]. Brinegar KN, Sheth RA, Khadenhosseni A, Bautista J, Oklu R, Iliac vein compression syndrome clinical imaging and pathological findingsWorld J Radiol 2015 7(11):375-81.10.4329/wjr.v7.i11.37526644823 [Google Scholar] [CrossRef] [PubMed]
[8]. Srisajjakul S, Prapasilp P, Bangchokdee S, Imaging features of vascular compression in abdomen: Fantasy, phenomenon or true syndromeIndian J Radiol Imaging 2017 27(2):216-24.10.4103/ijri.IJRI_7_1728744083 [Google Scholar] [CrossRef] [PubMed]
[9]. Jeon UB, Chung JW, Jae HG, Kim HC, Kim SJ, Ha J, May-Thurner syndrome complicated by acute iliofemoral vein thrombosis: Helical CT venography for evaluation of long-term stent patency and changes in the iliac veinAm J of Roentgen 2010 195(3):751-57.10.2214/AJR.09.279320729456 [Google Scholar] [CrossRef] [PubMed]
[10]. Alduck Am, Sullivan GO, CT Venography: Technique and indicationsEndovascular 2018 17(7):60-62. [Google Scholar]
[11]. Patel NH, Stookey KR, Ketcham DB, Cragg AH, Endovascular management of acute extensive iliofemoral deep venous thrombosis caused by May-Thurner syndromeJ Vasc Interv Radiol 2000 11(1):1297-302.10.1016/S1051-0443(07)61304-9 [Google Scholar] [CrossRef]