Dental prostheses are artificial substitutes for missing teeth, rehabilitating aesthetics and function [1]. Total and partial removable prostheses are conservative and low-cost rehabilitation treatments; therefore, they play an important socioeconomic function in Dentistry [2]. In addition to restoring masticatory function, rehabilitation has the potential to improve patients’ personal image, social interactions and quality of life [3].
Several instruments were developed in order to relate oral problems with quality of life and the health condition perceived by patients, called self-perception. Among these instruments are the OHIP-14 questionnaire and the VAS [4].
The OHIP-14 evaluates the impact of oral condition on quality of life through questions distributed across seven domains: functional limitation, physical pain, psychological discomfort, physical, psychological, social disability and disability in the performance of daily activities in the last 12 months, that are related to teeth, mouth and/or denture problems [5]. Recent studies using OHIP to assess removable rehabilitation achieved satisfactory results [6,7].
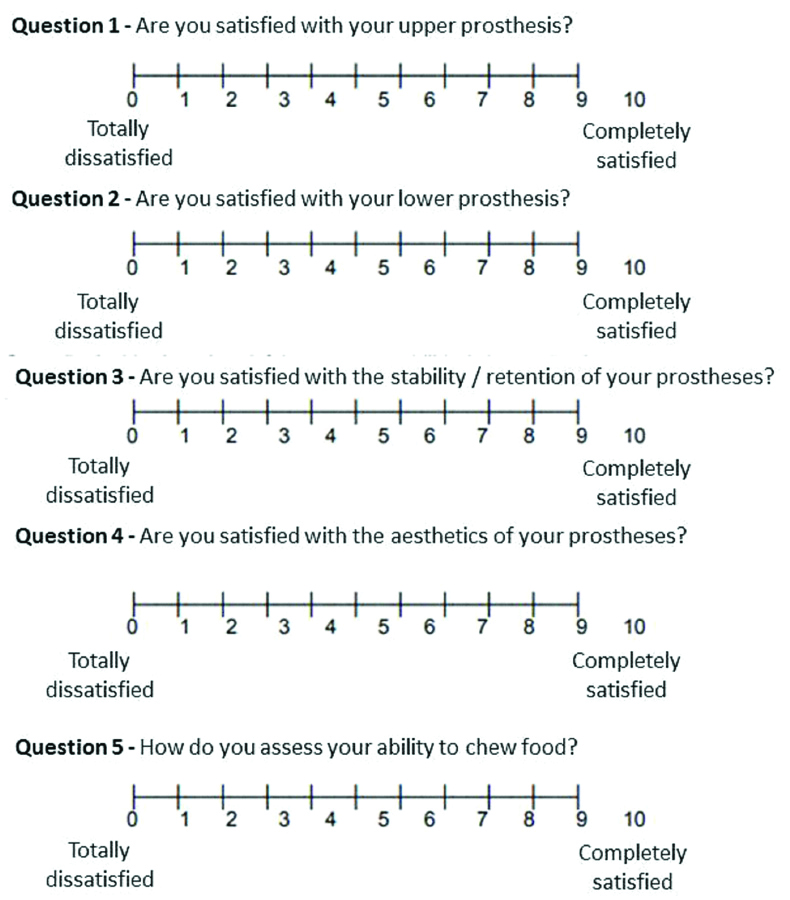
The VAS is a psychometric method to measure the satisfaction rate with rehabilitation. It consists of five questions: chewing function, satisfaction, comfort, stability/retention and aesthetics. VAS has been considered a very useful indicator when assessing questions related to the prosthetic therapy patients’ satisfaction [8,9].
Many are the factors that may interfere on patient’s self-perception and satisfaction with the rehabilitation. Psychoactive drugs, especially antidepressants, can cause dependence and reduce salivary flow, negatively interfering on the dental prostheses function [10-12]. An increase on the use of antidepressant medications by the population has been observed over the years, therefore, to understand the influence of these drugs on the overall experience with the rehabilitation using removable dental prostheses is important [10-13].
Disregarding the patients condition that lead to the use of antidepressants, the continuous use of this drug may interfere with patients response to the reahabiliation. Therefore, the main objective of this study was to evaluate the oral health self-perception and satisfaction of patients under treatment with antidepressants (regardingless the reason) rehabilitated by bimaxillary removable dentures using OHIP-14 and VAS. The hypothesis tested is that the use of antidepressant drugs, the age, the number of remaining teeth, the prosthesis type and time of use of prosthesis do not interfere with self-perception of oral health and satisfaction about the rehabilitation treatment.
Materials and Methods
This cross-sectional study was carried out between March and December 2019 at the School of Dentistry of the University of Passo Fundo, Passo Fundo, RS, Brazil (FOUPF), after approval by the institution’s Research Ethics Committee (No. 2.877.046).
One hundred and seventy-five medical records of patients rehabilitated with removable total and/or partial dentures between 2014 and 2019 were analysed. Patient selection was based on the following criteria:
Inclusion criteria: Patients aged between 40 and 90-year-old who were simultaneously rehabilitated with removable denture (partial and/or total) between 2014 and 2019, including non-users and antidepressants users for more than 1 year. The study compared users of dental prostheses that had the characteristic of “being removable” and rehabilitating both dental arches. Only patients with removable complete dentures or partial removable Kennedy Class I prostheses (bilateral free extremity) were included in the study, in order to compare prostheses with similar biomechanical characteristics [14,15], without occlusal units after the axis of rotation of the removable partial dentures.
Exclusion criteria: Patients unable to return to the institution due to health, death, financial unavailability or who showed no interest in attending the re-evaluation appointment. Users of removable partial dentures other than Kennedy Class I (bilateral free extremity) or users of removable dentures installed prior to 2014 were also excluded from the study.
All 175 patients were contacted, but only 23 (13%) individuals aged from 40 to 90-year-old (mean age 61.57 years) met the study inclusion criteria and consent was taken. The patients who participated in the research were evaluated in an appointment at the Dental School clinics. In this appointment, the volunteers signed a consent form and underwent clinical examination performed by a calibrated professional (intra-examiner kappa coefficient of 0.84) [15].
Use of antidepressants for at least one year, patient’s age, number of remaining teeth, prosthesis type and duration of use were recorded. Following the examiner instructions, each participant responded to the OHIP-14 [6,16] and used the VAS [6,8] to describe satisfaction with the rehabilitation. The OHIP-14 and the VAS scale are validated and public domain questionnaires, used in the methodology of numerous previous articles [6,8,16]. The volunteer had 15 minutes to answer the questions in a private room. After this time, the questionnaires were collected by the examiner.
The OHIP-14 is a validated questionnaire, used by several studies in the health area (including Dentistry) [6,8]. It is worth mentioning that this questionnaire was not modified by the authors of this study, respecting the original [4] and Portuguese version [17]. The OHIP-14 is a form composed by seven domains: functional limitation, pain, psychological discomfort, physical limitations, psychological limitations, social limitations and social disadvantage [4]. In each domain there are two questions to be answered, whose ordinal answers, regarding the impact of oral health on quality of life, can vary from zero to four, in a Likert scale, coded as follows: 0=never; 1=rarely; 2=sometimes; 3=often; 4=always [16,18]. The total OHIP-14 raw data score can range from zero to 56, where higher scores mean more negative impact on oral health. Therefore, the lower the value, the lower the negative impact of oral health on quality of life. The same logic will apply to each dimension for impact, which in this case ranges from 0 to 8 [4,16].
To assess the degree of satisfaction with rehabilitation, the VAS can be used. For each question there is a scale from 0 to 10, with 0, at the extremes, totally dissatisfied and 10, completely satisfied. VAS has been considered a very useful indicator when evaluating questions related to patient satisfaction with prosthetic therapy [8,9,19]. In the present study, a scale from 0 (lowest prosthesis satisfaction index) to 10 (highest prosthesis satisfaction index) was shown to the patient at the moment of the clinical examination [Table/Fig-1]. The score indicated by the volunteer was recorded.
Visual Analog Scale (VAS) [20].
Statistical Analysis
The collected data were recorded in Microsoft Excel 2010™. Subjective indicators (OHIP-14 and VAS) were considered continuous variables for subsequent statistical analysis. The impact of oral clinical characteristics (type and duration of prosthesis use) and general health conditions (functional capacity and antidepressants use) on the values of OHIP-14 and VAS were evaluated by the Mann-Whitney test (p≤0.05) using the SPSS (Statistical Package for the Social Sciences, version 24.0, SPSS Inc., Chicago, IL, USA).
Results
The hypothesis of the present study was rejected, since the use of antidepressant drugs interferes with patients’ self-perception of oral health and satisfaction about the rehabilitation treatment. In addition, the present study correlated essential clinical aspects like the patient’s age group, the number of remaining teeth, the prosthesis type and duartion of use of prosthesis with the results of the OHIP-14 and the VAS scale. Sample characterisation is shown in [Table/Fig-2].
Characterisation of the studied sample.
| Variables | n | % |
|---|
| Age (year) | 40-60 | 11 | 47.8 |
| 60-90 | 12 | 52.2 |
| Use of antidepressant | Non user | 15 | 65.2 |
| User | 8 | 34.8 |
| Prosthesis type | Upper and lower total prosthesis | 8 | 34.8 |
| Upper total prosthesis and lower partial prosthesis | 9 | 39.1 |
| Upper and lower partial denture | 6 | 26.1 |
| Year of installation | 2014 | 1 | 4.3 |
| 2015 | 2 | 8.7 |
| 2016 | 2 | 8.7 |
| 2017 | 7 | 30.4 |
| 2018 | 5 | 21.7 |
| 2019 | 6 | 26.1 |
| Remaining teeth | 0 | 8 | 34.8 |
| 1-10 | 12 | 52.3 |
| +10 | 3 | 12.9 |
Analysis of OHIP-14 and VAS results showed that type of prosthesis and number of remaining teeth did not influence on oral health self-perception and patient satisfaction (p>0.05) [Table/Fig-3,4]. Individuals older than 60 presented greater physical disability using total and partial prostheses (p=0.04) [Table/Fig-5]. The research was carried out in 2019. Therefore, patients who had their prostheses installed between 2014 and 2016 (prostheses for more than three years in use) had a lower functional domain than patients with prosthesis installed between 2017 and 2019 (prostheses in use for less than three years) (p=0.03). It was also noted that patients who underwent rehabilitation more recently (less than three years) resulted in greater ability to chew (p=0.02) when compared to patients using prostheses with longer time in function [Table/Fig-6].
Comparison between the type of prosthesis and the results of the OHIP-14 domains and the VAS results.
| OHIP-14 | VAS |
|---|
| Prosthesis type | General score | Functional domain | Physical pain | Psychological discomfort | Physical disability | Psychological disability | Social disability | Social disdvantage | Ability to chew | Satisfaction with the lower prosthesis | Satisfaction with the upper prosthesis | Prosthesis stability/retention | Prosthesis aesthetics |
|---|
| Upper and lower total prosthesis | Mean | 8.00 | 1.62 | 2.37 | 1.50 | 1.37 | 0.75 | 0.37 | 0.25 | 8.87 | 5.87 | 8.87 | 8.37 | 9.12 |
| N | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 |
| SD | 9.81 | 2.77 | 2.61 | 2.07 | 2.19 | 1.38 | 0.74 | 0.70 | 0.84 | 3.97 | 1.45 | 1.92 | 1.45 |
| Upper total prosthesis and lower partial prosthesis | Mean | 9.55 | 1.77 | 2.22 | 1.77 | 1.11 | 1.66 | 1.00 | 0.88 | 8.11 | 6.44 | 9.11 | 8.77 | 9.44 |
| N | 9 | 9 | 9 | 9 | 9 | 9 | 9 | 9 | 9 | 9 | 9 | 9 | 9 |
| SD | 13.43 | 2.33 | 2.77 | 2.63 | 2.31 | 2.64 | 2.00 | 1.69 | 1.53 | 3.94 | 1.69 | 1.30 | 1.33 |
| Upper and lower partial denture | Mean | 5.50 | 1.00 | 2.33 | 0.66 | 0.66 | 0.66 | 0.16 | 0.33 | 8.50 | 9.33 | 9.16 | 9.50 | 9.33 |
| N | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 6 |
| SD | 6.37 | 1.54 | 1.96 | 1.21 | 0.81 | 1.21 | 0.40 | 0.81 | 0.54 | 1.03 | 2.04 | 0.83 | 0.81 |
| p-value* | 0.77 | 0.81 | 0.99 | 0.61 | 0.80 | 0.53 | 0.46 | 0.51 | 0.39 | 0.17 | 0.94 | 0.38 | 0.88 |
*Mann-Whitney test (p≤0.05); SD: Standard deviation
Comparison between the number of remaining teeth with the results of the OHIP-14 domains and the VAS results.
| OHIP-14 | VAS |
|---|
| Categories for remaining teeth | General score | Functional domain | Physical pain | Psychological discomfort | Physical disability | Psychological disability | Social disability | Social disdvantage | Ability to chew | Satisfaction with the lower prosthesis | Satisfaction with the upper prosthesis | Prosthesis stability/retention | Prosthesis aesthetics |
|---|
| Totally edentulous | Mean | 8.00 | 1.62 | 2.37 | 1.50 | 1.37 | 0.75 | 0.37 | 0.25 | 8.87 | 5.87 | 8.87 | 8.37 | 9.12 |
| N | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 |
| SD | 9.81 | 2.77 | 2.61 | 2.07 | 2.19 | 1.38 | 0.74 | 0.70 | 0.83 | 3.97 | 1.45 | 1.92 | 1.45 |
| From 1 to 10 remaining teeth | Mean | 8.16 | 1.58 | 2.16 | 1.41 | 0.91 | 1.33 | 0.75 | 0.66 | 8.16 | 7.16 | 8.91 | 8.83 | 9.33 |
| N | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 |
| SD | 11.76 | 2.156 | 2.40 | 2.35 | 2.02 | 2.34 | 1.76 | 1.49 | 1.33 | 3.63 | 1.92 | 1.19 | 1.23 |
| More than 10 teeth remaining | Mean | 7.00 | 1.00 | 2.66 | 1.00 | 1.00 | 1.00 | 0.33 | 0.66 | 8.66 | 9.33 | 10.00 | 10.00 | 9.66 |
| N | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 |
| SD | 9.53 | 1.73 | 2.88 | 1.73 | 1.00 | 1.73 | 0.57 | 1.15 | 0.57 | 1.15 | 0.00 | 0.00 | 0.57 |
| p-value* | 0.98 | 0.91 | 0.95 | 0.94 | 0.88 | 0.81 | 0.80 | 0.74 | 0.38 | 0.37 | 0.57 | 0.27 | 0.81 |
|---|
*Mann-Whitney test (p≤0.05); SD: Standard deviation
Relation between the age of patients and the results of the OHIP-14 domains and the VAS results.
| OHIP-14 | VAS |
|---|
| Age groups | General score | Functional domain | Physical pain | Psychological discomfort | Physical disability | Psychological disability | Social disability | Social disadvantage | Ability to chew | Satisfaction with the lower prosthesis | Satisfaction with the upper prosthesis | Prosthesis stability/retention | Prosthesis aesthetics |
|---|
| Individuals between 40 and 60 years old | Mean | 5.27 | 1.18 | 1.63 | 0.90 | 0.36 | 0.72 | 0.45 | 0.45 | 8.54 | 8.09 | 9.18 | 9.18 | 9.36 |
| N | 11 | 11 | 11 | 11 | 11 | 11 | 11 | 11 | 11 | 11 | 11 | 11 | 11 |
| SD | 5.90 | 1.53 | 1.68 | 1.13 | 0.67 | 1.42 | 0.82 | 0.82 | 1.36 | 2.94 | 1.32 | 1.25 | 1.20 |
| Individuals over 60 | Mean | 10.41 | 1.83 | 2.91 | 1.83 | 1.75 | 1.41 | 0.66 | 0.58 | 8.41 | 6.00 | 8.91 | 8.50 | 9.25 |
| N | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 |
| SD | 13.07 | 2.79 | 2.87 | 2.69 | 2.45 | 2.31 | 1.72 | 1.50 | 1.12 | 3.60 | 1.63 | 1.46 | 1.22 |
| p-value* | 0.24 | 0.50 | 0.21 | 0.30 | 0.04 | 0.40 | 0.71 | 0.80 | 0.80 | 0.17 | 0.70 | 0.27 | 0.83 |
*Mann-Whitney test (p≤0.05); SD: Standard deviation
Relationship between prosthesis usage time and the results of the OHIP-14 domains and the VAS results.
| OHIP-14 | VAS |
|---|
| Prosthesis usage time | General score | Functional domain | Physical pain | Psychological discomfort | Physical disability | Psychological disability | Social disability | Social disdvantage | Ability to chew | Satisfaction with the lower prosthesis | Satisfaction with the upper prosthesis | Prosthesis stability/retention | Prosthesis aesthetics |
|---|
| 3-6 years | Mean | 9.72 | 1.94 | 2.61 | 1.66 | 1.38 | 1.38 | 0.72 | 0.66 | 8.3 | 6.8 | 8.8 | 8.6 | 9.2 |
| N | 18 | 18 | 18 | 18 | 18 | 18 | 18 | 18 | 5 | 5 | 5 | 5 | 5 |
| SD | 11.16 | 2.38 | 2.63 | 2.30 | 2.09 | 2.09 | 1.48 | 1.32 | 1.2 | 4.08 | 1.78 | 1.67 | 1.78 |
| Up to 3 years | Mean | 1.60 | 0.00 | 1.20 | 0.40 | 0.00 | 0.00 | 0.00 | 0.00 | 9.1 | 7.0 | 9.1 | 8.8 | 9.3 |
| N | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 18 | 18 | 18 | 18 | 18 |
| SD | 1.14 | 0.00 | 0.83 | 0.54 | 0.00 | 0.00 | 0.00 | 0.00 | 0.7 | 3.58 | 1.64 | 1.45 | 1.08 |
| p-value* | 0.12 | 0.03 | 0.25 | 0.24 | 0.15 | 0.15 | 0.25 | 0.28 | 0.02 | 0.89 | 0.71 | 0.70 | 0.83 |
*Mann-Whitney test (p≤0.05); SD: Standard deviation
On assessment of patient’s questionnaire, it was noted that 8 out of 23 patients (34.78%) used antidepressants. This class of drugs may interfere in the use of removable prostheses mainly because they reduce the amount of saliva and can negatively interfere in the patients’ subjective perception of oral health [10-12]. In this study, the use of antidepressants was statistically associated with several aspects addressed in OHIP-14: higher overall score in the OHIP-14 questionnaire (p=0.04), higher average physical pain (p=0.03), more psychological discomfort (p=0.03) and more physical disability (p=0.03). When analysing the results of VAS, it was observed that patients not using antidepressants had greater satisfaction with the stability/retention of prostheses (p=0.01) when compared to those using this medication [Table/Fig-7].
Relationship between antidepressant use and the results of the OHIP-14 domains and the VAS results.
| OHIP-14 | VAS |
|---|
| Use of antidepressants | General score | Functional domain | Physical pain | Psychological discomfort | Physical disability | Psychological disability | Social disability | Social disdvantage | Ability to chew | Satisfaction with the lower prosthesis | Satisfaction with the upper prosthesis | Prosthesis stability/retention | Prosthesis aesthetics |
|---|
| No antidepressant-use | Mean | 4.80 | 1.06 | 1.66 | 0.73 | 0.46 | 0.53 | 0.33 | 0.20 | 8.4 | 7.2 | 9.1 | 9.3 | 9.6 |
| N | 15 | 15 | 15 | 15 | 15 | 15 | 15 | 15 | 15 | 15 | 15 | 15 | 15 |
| SD | 4.88 | 1.66 | 1.67 | 1.03 | 0.91 | 1.24 | 0.72 | 0.56 | 1.12 | 3.8 | 1.40 | 0.72 | 0.61 |
| Antidepressant-use | Mean | 13.87 | 2.37 | 3.50 | 2.62 | 2.25 | 2.12 | 1.0 | 1.12 | 8.5 | 6.6 | 8.87 | 7.8 | 8.6 |
| N | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 |
| SD | 15.19 | 3.02 | 3.20 | 3.02 | 2.76 | 2.58 | 2.07 | 1.80 | 1.19 | 3.37 | 2.10 | 2.0 | 1.76 |
| p-value* | 0.04 | 0.19 | 0.03 | 0.03 | 0.03 | 0.06 | 0.26 | 0.07 | 0.94 | 0.71 | 0.72 | 0.01 | 0.51 |
*Mann-Whitney test (p≤0.05); SD: Standard deviation
Discussion
The present study investigated the influence of continuous use of antidepressants on the self-perception of oral health and satisfaction of a patients group rehabilitated by bimaxillary removable dentures. Some studies report that antidepressants can cause interference with oral health and the function of complete dentures [11,21,22]. However, in other populations it was not possible to identify the effects of drugs with dissatisfaction or difficulty in using full dentures [23].
Tooth loss (total or partial) causes changes physical, psychological and social, leading to psychological shocks, depression or decreased self esteem [24]. Such condition can contribute to high drug use, mainly antidepressants, which directly influence the development of bruxism and dissatisfaction with the prostheses. Adverse effects of psychotropic drugs in the etiology of bruxism are still not well understood. In addition, research on the use of psychoactive drugs is commonly overlooked during anamnesis, making the matter even more complex for health professionals [25]. Based on the results presented for this study, it can be said that the unique point of this research is that the continuous use of antidepressants can influence the perception of oral health and the satisfaction of users of removable bimaxillary dental prostheses.
The use of antidepressants was significantly associated to several factors investigated using OHIP-14. The users of this class of drugs had a higher overall score, a higher average of physical pain, greater psychological discomfort and greater physical disability. Notably, antidepressant medications may result in reduced salivary flow (xerostomia), directly interfering with the adaptation and effectiveness of dental prostheses [10-13] and weakning the patient’s psychological aspect [11,26].
In data found by VAS, it can be observed that patients using antidepressant were less satisfied about prostheses’ stability and retention. This may be caused by psychological issues, such as depression, anxiety and emotional aspects of antidepressant users, that may negatively interfere on their satisfaction [27]. Besides that, the stomatognathic complex remains stable in non-antidepressant users, presenting fewer alterations such as xerostomia or bruxism [28].
It is noteworthy that serotonin, the main neurotransmitter on which antidepressants act, may have an appetite-regulating role and in the choice of macronutrients, promoting a reduction in appetite and the preferential choice for protein foods, which can generate fragility of the body mucous membranes [29]. Lakey SL et al., found that continued use of antidepressants can also lead to weight loss and muscle mass reduction [30]. Both the fragility of the mucous membranes and the reduction of motor coordination are situations that decrease patients adaptation to dental prostheses and their satisfaction with the rehabilitation.
When studying 201 Brazilians elderly, Bandeira VAC et al., described an association of fragility syndrome with the use of antidepressants [31]. According to the authors, the syndrome is characterised by a decline in energy and is related to changes in the musculoskeletal, neuroendocrine and immune systems that affect, especially, the loss of muscle mass, changes in appetite and chronic inflammatory state. Still, the fragility phenotype involves five components: unintentional weight loss, fatigue, decreased handgrip strength, slow gait and low level of physical activity. Although, it cannot be said that all patients who used antidepressants in the present study had fragility syndrome (a theme for future studies), it is possible to correlate the use of that class of drugs with the lowest self-perception of oral health and lowest satisfaction in relation to dental prostheses.
In order to reduce the risk of bias, in this study the patients were divided into three subgroups (type of prosthesis): “Users of upper and lower total dentures” (n=8), “Users of upper and lower partial dentures” (n=6), and “Users of upper total dentures and lower partial dentures” (n=9). Based on the score of OHIP-14 and VAS found in this research, the type of prosthesis had no influence on patients self-perception of oral health and satisfaction. Similar results were found in a previous study [14] that showed no difference on general satisfaction (VAS scale), aesthetics or comfort between partial or total removable prostheses users.
Conversely, Beloni WB et al., demonstrated that patients rehabilitated with complete dentures had a greater impact on quality of life (p=0.01), reported better stability (p=0.01) and masticatory function (p=0.01) compared to those rehabilitated with partial removable dentures [32]. The recall time of Beloni WB et al., study was shorter than the previous mentioned studies: patients were called just two months after finishing the prosthetic rehabilitation [32]. Therefore, a difference in self-perception of oral health and satisfaction between patiens rehabilitated with complete and partial dentures could be expected within the first months of prosthesis function. However, this difference may decrease over the years, because of the decrease in the satisfaction with the masticatory function observed in this study.
The influence of the number of remaining teeth present at the clinical examination (varying from zero- complete edentulous arch - to more than 10 teeth) on health self-perception and patient satisfaction was also analysed in the present study. However, no statistically significant association was found, which agrees with a previous study [15]. However, a systematic review of the literature by De Kok IJ et al., showed that the number of remaining teeth in users of conventional removable dentures is directly related to their degree of satisfaction [33]. The differences among these results may be attributed to the number of patients analysed: De Kok IJ et al., in a systematic review analysed data from 4002 patients, while the present study evaluated 23 patients [33].
Significant results were obtained with the application of OHIP-14 in the present study with respect to the relationship between patients’ physical disability and age. Patients older than 60 presented greater physical disability in the use of removable prostheses. This can be explained by the difficulty of chewing food associated with changes that occur in the stomatognathic system with age, such as decreased salivary flow, muscle tone and motor coordination [34]. This result also adds to the statement by De Kok IJ et al., according to which, the older the patients, the lower the acceptability of removable prostheses [33].
It was observed that patients who had their prostheses in function from less than three years showed greater functional domain in the use of prostheses (detected by OHIP-14) and a greater ability to chew (detected by the VAS scale). According to Ribeiro FS et al., new prostheses generally result in an increase in patient satisfaction and quality of life because they have better technical qualities (e.g., retention, stability, cutting ability and grinding of the bolus), besides exerting a positive psychological effect on the patient [35]. In addition, Divaris K et al., state that as the time of use of the prosthesis increases, the ability to cut and grind the food decreases, mainly due to the wear of the prostheses artificial teeth over the time [36]. Besides that, the residual alveolar ridge remodeling can reduce the contact between the base of the prosthesis and the fibromucosa.
Limitation(s)
The small number of participants can be considered a limitation of the present study.
Conclusion(s)
Patients using antidepressants had a higher overall OHIP score, a higher average of physical pain, greater psychological discomfort, physical disability and less satisfaction with the stability/retention of removable prostheses, indicating that the use of such a class of drugs negatively influences the rehabilitated patient. It was also noted that older patients have greater physical disability in the use of removable prostheses, and that the time of use of the prostheses directly interferes with the functional domain and ability to chew of users.
*Mann-Whitney test (p≤0.05); SD: Standard deviation
*Mann-Whitney test (p≤0.05); SD: Standard deviation
*Mann-Whitney test (p≤0.05); SD: Standard deviation
*Mann-Whitney test (p≤0.05); SD: Standard deviation
*Mann-Whitney test (p≤0.05); SD: Standard deviation