Asymptomatic Solitary Mastocytoma with Negative Darier’s Sign
Azra Fathima1, Krishnakanth Muralidhar2, Mahalakshmi Veeraraghavan3, R Madhu4, Leena Dennis Joseph5, Murugan Sundaram6
1 Junior Resident, Department of Dermatology, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
2 Associate Professor, Department of Dermatology, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
3 Professor, Department of Dermatology, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
4 Professor, Department of Paediatric Surgery, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
5 Professor, Department of Pathology, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
6 Head, Department of Dermatology, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Azra Fathima, Ramachandra Nagar, Porur, Chennai, Tamil Nadu, India.
E-mail: drazrafathima@gmail.com
Mastocytosis is a heterogenous group of disorders characterised by clonal proliferation of mast cells accumulating in single or multiple organs in children or adults. Skin is the most common organ involved in children. It usually presents as a nodule or plaque, yellow to tan-brown in colour remaining asymptomatic or may become red and itchy on rubbing indicating Darier’s sign positivity which helps in clinical diagnosis of mastocytosis. This case is of a three-month-old baby who presented with solitary asymptomatic noduloplaque with negative Darier’s sign which was clinically suspected to be mastocytosis and was confirmed by histopathology and immunohistochemistry.
Good prognosis, Noduloplaque, Non-itchy, Paediatric mastocytosis
Case Report
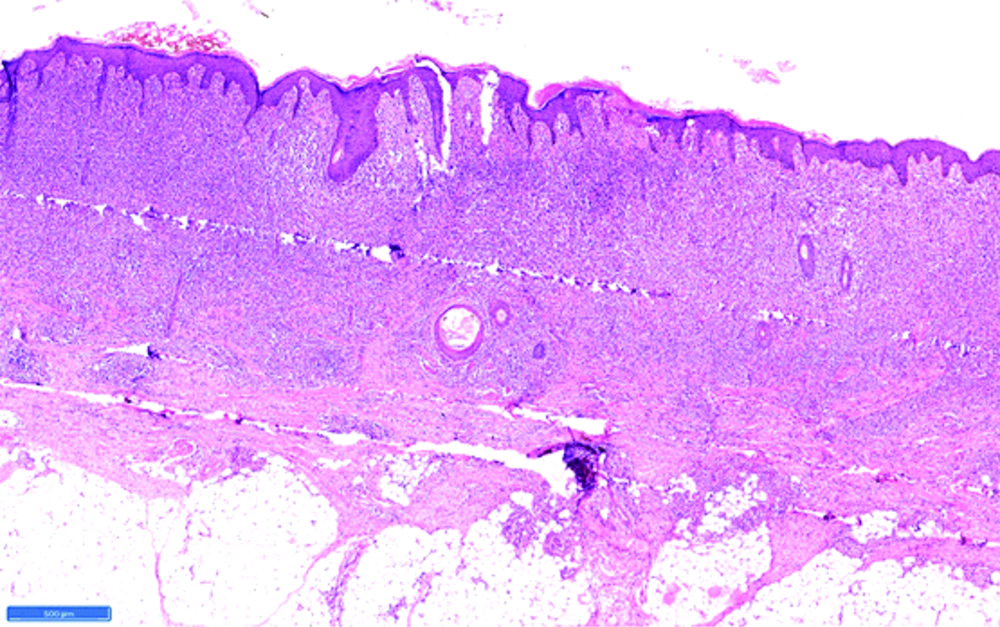
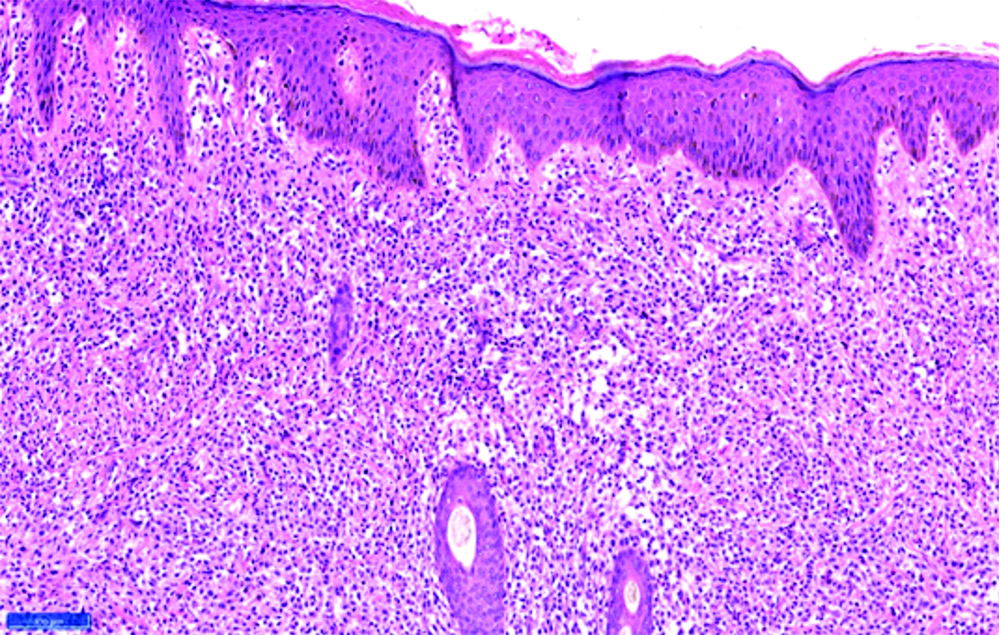
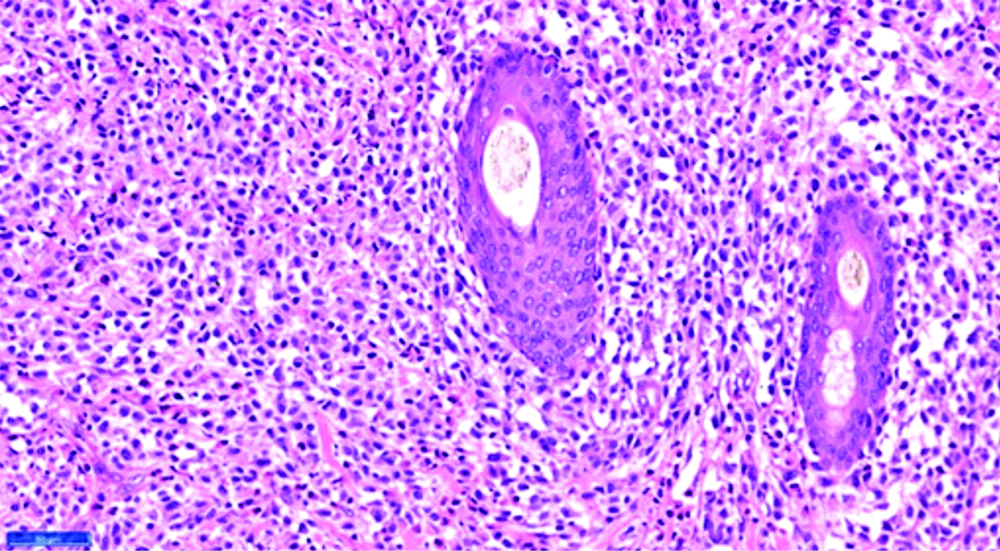
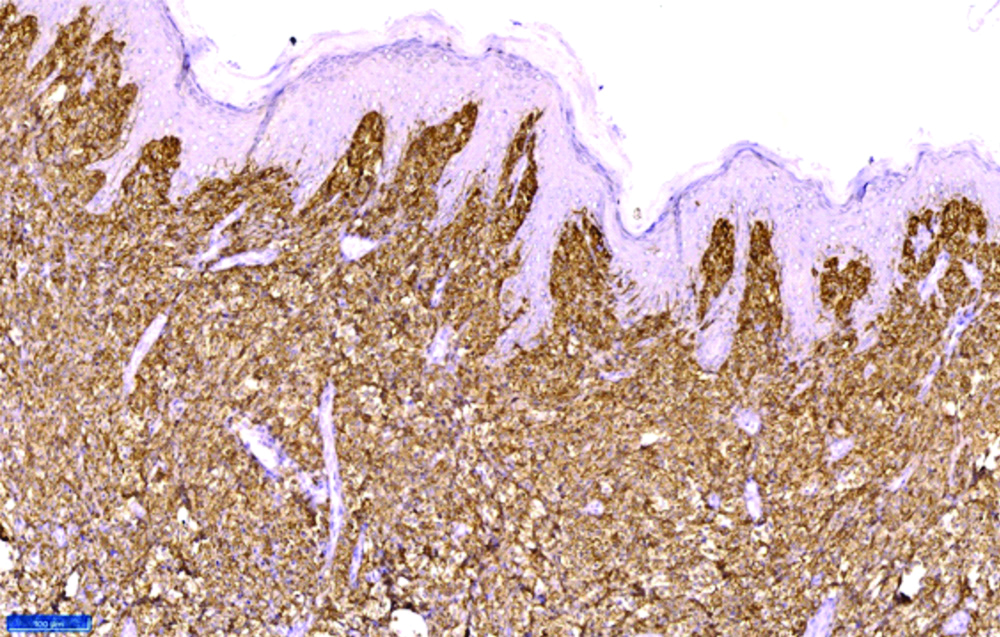
A three-month-old male baby presented with complaints of raised skin lesion over left leg since birth. He was a full term baby delivered by normal vaginal delivery, cried immediately after birth. Neonatal period was uneventful. Mother started noticing a dark coloured skin lesion over the left leg after birth which gradually increased in size to attain the present size. The lesion was asymptomatic and the parents reported with a concern that the lesion was increasing in size. The child was comfortable with the examination and had a solitary well-defined noduloplaque of size 2 × 3.5 cm, skin coloured, soft to firm in consistency, non-tender over the extensor aspect of left leg as depicted in [Table/Fig-1]. Darier’s sign was negative. A diagnosis of solitary mastocytoma was made and differentials like xanthogranuloma and melanocytic naevus were considered. Routine blood investigations including complete blood count, peripheral smear and serum tryptase levels were found to be within normal limits. Excision biopsy was done and histopathological examination showed sheets of cells arranged in the superficial and deep dermis as shown in [Table/Fig-2,3]. The infiltrate was present around adnexal structures as depicted in [Table/Fig-4]. The cells had moderate to scanty cytoplasm and vesicular nucleus. No evidence of any giant cell or atypia or epidermotropism was noted. Giemsa stain was done and metachromatic staining of mast cells was demonstrated. A diagnosis of mastocytoma was made and further confirmation was done with immunohistochemistry, which expressed vimentin and CD117 positivity as shown in [Table/Fig-5]. Immunohistochemistry was negative for S100 and HMB-45. The child is currently under follow-up.
A single nodulo-plaque over the anterior aspect of leg.

Histopathological examination showing diffuse infiltrate over the entire dermis (H&E,10X).
Histopathological examination mast cell infiltration in dermis (H&E,40X).
Histopathological examination (High power) showing diffuse mast cell infiltration around appendages.
Immunohistochemistry showing CD117 positivity throughout the dermis.
Discussion
Mastocytosis is a disease with different clinical variants, characterised by pathological increase in mast cells in skin and extracutaneous sites like bone marrow, spleen, lymphnodes and liver. Solitary mastocytoma is the second common type contributing 10% to 15% of cutaneous mastocytosis [1,2]. Mastocytosis can present in two age related patterns: paediatric-onset and adult-onset. In paediatric-onset mastocytosis, cutaneous involvement of mast cells is most common and systemic involvement is very rare. Adult-onset mastocytosis is characterised by systemic involvement and increased severity. Prevalence of solitary mastocytoma is unknown in Indian population. In western literature, annual incidence of 5-10 new cases per million population has been projected. Mastocytosis can present during any age. Approximately, in 15% of children, the disease is congenital and in 50% of children the onset is between birth and two years [3].
Pathogenesis remains unknown. A transient dysregulation in the stem cell factor which is a growth factor needed for mast cell growth and differentiation has been identified thus leading to increased production or decreased apoptosis of mast cells [2]. Childhood mastocytosis can occur in any age less than 16 years, and is usually identified prior to two years of age. Urticaria pigmentosa (70-90%) is the most common clinical pattern of childhood mastocytosis, followed by solitary mastocytoma (10-35%), diffuse cutaneous mastocytosis (1-3%), and a rare form called as telengiectasia macularis eruptive perstans [4].
Majority of solitary mastocytomas occur in infancy, typically by three months of age. Clinically, they present as a single indurated macule, papule, or plaque, red-brown in colour over the extremities, trunk, or head and neck. The clinical features are not due to accumulation of mast cells but due to release of mediators of mast cells which may vary from pruritus, blistering to flushing, urticaria and anaphylaxis [2]. Darier’s sign can be elicited in 50% of patients [5]. Two cases of trauma induced solitary mastocytoma under a tight bracelet were reported [5]. Complete blood count and serum tryptase levels and skin biopsy should be initially done in all patients. If there is an abnormal complete blood count and serum tryptase more than 20 ng/mL, bone marrow biopsy and aspiration is indicated [6]. Usually, bone marrow aspiration and biopsy are not recommended in acute onset mastocytosis below five years of age. Skin biopsy shows mast cell accumulation in the dermis. Mast cells can be differentiated by metachromatic staining with Giemsa and Toluidine dyes. Positive immunostaining for tryptase and c-KIT confirms the diagnosis [7]. The differential diagnosis of xanthogranuloma and melanocytic naevus was ruled out in present patient due to absence of foamy macrophages and immunohistochemistry being negative for HMB-45 respectively.
Based on the number of lesions, the involvement of lymph nodes and distant metastases, WHO system classifies cutaneous mastocytosis into four stages [8]. Present patient had a solitary lesion with no lymph node involvement and hence was considered to be in stage 1. Considering the benign nature of mastocytosis, the primary emphasis is to prevent the mast cell mediator release by avoiding the triggering factors like acute temperature changes, rubbing the skin lesion, insect bite, stress and drugs which include codeine, aspirin, morphine, alcohol and radiocontrast substances having iodine. Topical treatment options include corticosteroids and calcineurin inhibitors [1]. Treatment of acute mast cell activation includes education of parents and caretakers regarding epinephrine auto injector use in case of hypotension due to acute mast cell degranulation, H1 and H2 antihistaminics, topical and oral cromolyn sodium [4]. Factors strongly associated with disease resolution in paediatric-onset mastocytosis include a lower age at onset (<2 years), lower extent of skin affected and a normal bone-marrow examination [9].
Conclusion(s)
Paediatric onset mastocytosis differs in presentation and prognosis from adults. A physical examination with positive Darier’s sign and symptoms related to mast cell mediator release helps in clinical diagnosis which were absent in this patient. This baby was referred to us as a case of chronic abscess treated with antibiotics. Hence, a high degree of suspicion is required in asymptomatic patients as Darier’s sign is not always positive and clinico-pathological correlation will help in these situations.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jan 31, 2020
Manual Googling: Mar 12, 2020
iThenticate Software: Apr 16, 2020 (7%)
[1]. Sukesh MS, Dandale A, Dhurat R, Sarkate A, Ghate S, Case Report: Solitary mastocytoma treated successfully with topical tacrolimusF1000 Research 2014 3:18110.12688/f1000research.3253.125210620 [Google Scholar] [CrossRef] [PubMed]
[2]. Castells M, Metcalfe DD, Escribano L, Guidelines for the diagnosis and treatment of cutaneous mastocytosis in childrenAm J Clin Dermatol 2011 12(4):259-70.10.2165/11588890-000000000-0000021668033 [Google Scholar] [CrossRef] [PubMed]
[3]. Srinivas S, Dhar S, Parikh D, Mastocytosis in childrenIndian J Paediatr Dermatol 2015 16(2):57-63.10.4103/2319-7250.154801 [Google Scholar] [CrossRef]
[4]. Tamay Z, Özçeker D, Current approach to cutaneous mastocytosis in childhoodTurk Arch Pediatr Pediatri Arş 2016 51(3):123-27.10.5152/TurkPediatriArs.2016.241827738395 [Google Scholar] [CrossRef] [PubMed]
[5]. Koh WL, Tay YK, Sim CS, Solitary mastocytoma arising from a tight infant identification braceletIndian J Paediatr Dermatol 2018 19(3):25810.4103/ijpd.IJPD_85_17 [Google Scholar] [CrossRef]
[6]. Ferrante G, Scavone V, Muscia MC, Adrignola E, Corsello G, Passalacqua G, The care pathway for children with urticaria, angioedema, mastocytosisWorld Allergy Organ J 2015 8(1):510.1186/s40413-014-0052-x25674297 [Google Scholar] [CrossRef] [PubMed]
[7]. Valent P, Akin C, Metcalfe DD, Mastocytosis: 2016 updated WHO classification and novel emerging treatment conceptsBlood 2017 129(11):1420-27.10.1182/blood-2016-09-73189328031180 [Google Scholar] [CrossRef] [PubMed]
[8]. Ahmed A, Jan A, MastocytomaIn: StatPearls [Internet] 2020 [cited 2020 Mar 8] Treasure Island (FL)Stat Pearls PublishingAvailable from: http://www.ncbi.nlm.nih.gov/books/NBK538252/ [Google Scholar]
[9]. Matito A, Azaña JM, Torrelo A, Alvarez-Twose I, Cutaneous mastocytosis in adults and childrenImmunol Allergy Clin North Am 2018 38(3):351-63.10.1016/j.iac.2018.04.001 [Google Scholar] [CrossRef]