Chromosomal abnormality is one of the causes of human genetic diseases or disorders, in which structural or numerical changes occur. Many diseases or disorders like mental retardation, primary amenorrhea, irregular menstruation, recurrent pregnancy loss, male infertility, disorders of sexual development and syndromes like Klinefelter syndrome, Turner syndrome, Edward’s syndrome, Down syndrome etc., are caused due to numerical or structural chromosomal aberration [1]. The involvements of chromosome abnormalities are known in many human genetic diseases and disorders. Cytogenetic analysis is essential to reveal chromosomal deletion, translocation, duplication, inversion and aneuploidy of the autosomes and sex chromosomes [2]. Chromosomal abnormalities occur around 0.5-1% of live births and it increases up to 2% of pregnancies in above 35-year-old pregnant women. Worldwide studies suggest that around 50% of pregnancies aborted spontaneously in first trimester are due to chromosomal abnormalities [3]. The awareness of the importance of chromosomal abnormalities as a cause of disorder and diseases has generated an increased demand for cytogenetic studies to settle down the unknown aetiologies of the anomalies [4]. The recent development of advanced molecular cytogenetic techniques allowed to address many chromosomal syndromes including deletions, duplications, microdeletions as well as rearrangements of chromosomes [2]. Numerical chromosome abnormalities are the main causes of genetic disorders in case of Down syndrome, Turner syndrome, Klinefelter syndrome, Patau syndrome, etc. However, structural rearrangements have been identified in many Turner syndrome and in a few Down syndrome patients [5,6]. Structural rearrangements of chromosomes and balance reciprocal translocation are responsible for the dysmorphic features or fertility problems in patients possessing these rearrangements [7]. In the recent years, chromosomal and molecular genetics analysis has become a very essential and important tool for genetic diagnosis and counselling, which deals with the human problems associated with the risk or recurrence of a genetic disorder in a family and helps to understand the diagnosis, prognosis, available management, and the options available [8]. Variations in frequencies of genetic diseases and disorders are linked to population and geographical variations. There are no registries or databases of genetic diseases and disorders in India. The study, which includes hospital-based patients from central Indian population, is first of its kind from central India. The data can be used for making national database for genetic disorders. The present study was carried out to identify the types and frequencies of chromosomal anomalies among the suspected patients referred to Human Genetics Division from hospital.
Materials and Methods
The present cross-sectional study was carried out in Human Genetics Division Mahatma Gandhi Institute of Medical Sciences, Wardha, Maharashtra, India retrospectively during the period of January 2000 to June 2019 to find out the prevalence and pattern of cytogenetic abnormalities among the 2215 referred patients of suspected genetic abnormalities. The cytogenetic analysis was performed after collecting detailed history of medical problems of the patients. The informed written consent form was taken from all the patients. Based on clinical findings all patients were grouped for karyotyping: 1) Down syndrome; 2) Male infertility; 3) Primary amenorrhea; 4) Recurrent pregnancy loss; 5) Ambiguous genitalia; 6) Congenital abnormalities; 7) Psychiatric disorders. For routine diagnosis of cytogenetic analysis, heparinised peripheral blood (2 mL) was collected from the patients and lymphocytes cultures were set up according to laboratory standardised technique [9]. Lymphocytes cultures were harvested and slides were prepared following conventional process and slides were stained with Giemsa-Trypsin-Giemsa (GTG) banding method. Karyotype was prepared following the guidelines of International system for Human Cytogenetics Nomenclature [10]. At least 30 good spread and sharp banded metaphases were analysed and the cytogenetic abnormalities (structural and numerical) were noted. Descriptive statistic method was used to analyse cytogenetic results. The post-test genetic counseling was provided to all the patients who were recruited for cytogenetic analysis.
Results
In the present study, 2215 patients with suspected chromosomal anomalies were referred from various clinical departments for cytogenetic analysis. The patients referred for cytogenetic analysis was distributed on the basis of clinical findings noted by clinicians. The percentages of cytogenetic analysis and different abnormal karyotypes are shown [Table/Fig-1,2 and 3].
Distribution of referred suspected patients in following groups and its abnormal cytogenetic data from blood specimen.
| Reasons for referral | Total number and % of referred patients of different groups | No. and % of abnormal cytogenetic patients in different groups |
|---|
| Down syndrome | 214 (*F) | 98 (59.75%) |
| 128 (#M) | 66 (40.25%) |
| 342 (15.44%) | 164 (47.95%) |
| Primary amenorrhea | 383 (17.29%) | 36 (9.40%) |
| Recurrent pregnancy loss | 768 (34.67%) | 20 (2.60%) |
| Male infertility | 473 (21.35%) | 30 (6.34%) |
| Ambiguous genitalia | 72 (3.25%) | 6 (8.33%) |
| Congenital abnormalities | 147 (6.63%) | 13 (8.84%) |
| Psychiatric | 30 (1.35%) | 2 (6.66%) |
| Total | 2215 | 271 (12.23%) |
*F: Female; #M: Male
Distribution of numerical and structural chromosomal abnormalities in different groups detected among 271 cases.
| Numerical aberration | Structural aberration |
|---|
| Types of abnormal karyotypes of different groups | No. of patients with abnormal karyotype | Types of abnormal karyotypes of different groups | No. of patients with abnormal karyotype |
|---|
| Down syndrome | | Down syndrome | |
| Trisomy 21 (47,XY,+21/47,XX,+21) | 152 | Robertsonian translocation 46,XX/46,XX,t(21;21) | 10 |
| Mosaic karyotype (46,XX/47,XX,+21) | 1 | Reciprocal translocation | 1 |
| Primary amenorrhea | | Primary amenorrhea | |
| 45X | 6 | 45,X/46,X,i(Xq); 45,X/46,X,der(X) | 5 |
| Mosaic45X/46XY, 45,X/46,XX;(45,X/47,XXX)47,XXX | 8 | 46,X,r(X) | 1 |
| Sex reverse female/Complete androgenInsensitive syndrome (46,XY) | 16 |
| Recurrent pregnancy loss | | Recurrent pregnancy loss | |
| 47,XXX;Mosaic (45,X/46,XX) | 2 | Reciprocal translocation | 10 |
| Robertsonian translocation | 2 |
| Inversion | 6 |
| Male infertility | | Male infertility | |
| 47,XXY | 26 | 46,XYq-46,XX (sex reverse male) | 2 |
| 47,XYY | 1 | Reciprocal translocation46,XY,t(1q;22q) | 1 |
| Ambigous genitalia | | Ambiguous genitalia | |
| Mosaic (45,X/46,XY;46,XY/47,XXY) | 3 | (46,XY,der(9); sex reverse male: 46,XX) | 3 |
| Congenital abnormalities | | Congenital anomalies | |
| Autosomal trisomies(47,XY,+13, 47,XX,+18,) | 4 | 46,XX,der(15); 46,XX,inv(9);Reciprocal translocation; | 9 |
| Psychiatric | | Psychiatric | |
| 47,XX,(+mar) | 1 | Robertsonian translocation 45,XX,t(13;14) | 1 |
| Total | 204 (75.27%) | Total | 67 (24.72%) |
Grand total (Numerical + Structural) 204+67=271
Distribution of different types of abnormal karyotypes in different groups of 271 patients.
| Diagnosis and abnormal karyotypes | Number of patients with abnormal karyotypes | Percentage of different groups with abnormal karyotypes |
|---|
| Down syndrome | 164 | | 60.51 | Intra group (%) |
| 47,XX,+21 or 47,XY,+21 | | 152 | | 92.68 |
| t(13;21), (14;21), t(21;21) | | 10 | | 6.10 |
| Reciprocal translocation t(9;21) | | 1 | | 0.61 |
| Mosaic (46,XX/47,XX,+21) | | 1 | | 0.61 |
| Primary amenorrhea | 36 | | 13.31 | |
| 45,X | | 6 | | 16.67 |
| 46,Xi(Xq) | | 3 | | 8.33 |
| 45,X/46,XX or XY; 45,X/46,X,der(X); 47,XXX,Mosaic karyotype | | 10 | | 27.78 |
| 46,X(r),X | | 1 | | 2.78 |
| Sex reverse (10); female/complete androgen insensitive syndrome (6) | | 16 | | 44.44 |
| Recurrent pregnancy loss | 20 | | 7.38 | |
| Reciprocal translocation | | 10 | | 50.00 |
| Robertsonian translocation | | 2 | | 10.00 |
| Inversion | | 6 | | 30.00 |
| Numerical aberration | | 2 | | 10.00 |
| Male infertility | 30 | | 11.07 | |
| 47,XXY | | 26 | | 86.67 |
| 46,XX | | 1 | | 3.33 |
| 47,XYY | | 1 | | 3.33 |
| 46,XYq- | | 1 | | 3.33 |
| Reciprocal translocation t(1q;22q) | | 1 | | 3.33 |
| Ambiguous genitalia | 6 | | 2.21 | |
| Congenital anomalies | 13 | | 4.79 | |
| Psychiatrics | 2 | | 0.73 | |
| Total | 271 | | 100 | |
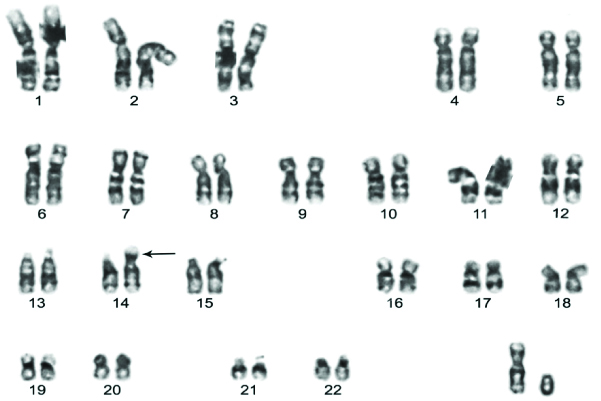
Down syndrome: Among the 342 (15.44%) clinically suspected Down syndrome patients, 164 cases were confirmed with Down syndrome and out of which 98 (59.75%) were females and 66 (40.25%) were males [Table/Fig-1,2]. Trisomy 21 was observed as most common type of Down syndrome (92.68%) followed by Robertsonian translocation and mosaic [Table/Fig-3,4]. The common type of Robertsonia translocation was noted between 14;21 followed by 13;21 and 21;21 and a rare reciprocal translocation involving chromosome 9;21 were also noted [Table/Fig-3].
The karyotype showing typical Robertsonian translocation t(14;21) in Down syndrome case.
Primary amenorrhea: Out of 383 females, 36 (9.40%) cases with primary amenorrhea were confirmed for cytogenetic abnormalities with Turner’s syndrome, testicular feminisation or sex reversal females karyotype [Table/Fig-1,2]. The percentages of different types of abnormal karyotypes in pure Turner, mosaic Turner, sex reversal female and other types of amenorrhea cases are shown in [Table/Fig-3].
The karyotype showing Reciprocal translocation {46,XY,t(2p;3q)} in recurrent pregnancy loss suspected male.
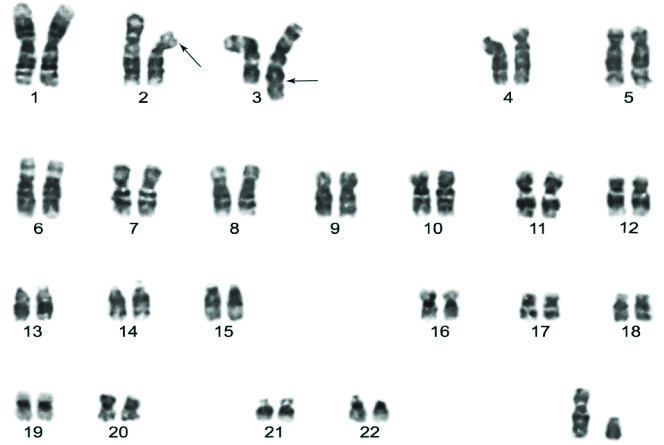
Recurrent pregnancy loss: The clinically suspected referred 384 couples (768 individuals) of recurrent pregnancy loss were successfully karyotyped and results indicated that 20 (2.60%) cases with various types of abnormal karyotypes. The reciprocal translocations were most common chromosomal abnormalities [Table/Fig-5] followed by inversion, Robertsonian translocation and numerical chromosome abnormalities. The percentages of different types of abnormal karyotypes are shown in [Table/Fig-3].
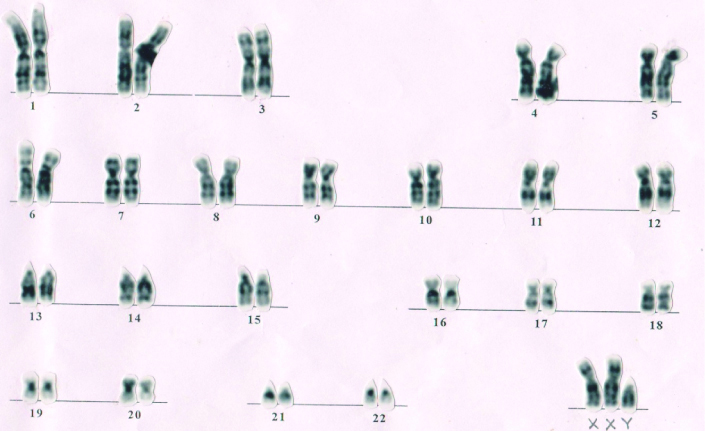
Male infertility: Of the 473 azoospermic and oligozoospermia infertile males, 30 (6.34%) infertile males had abnormal karyotypes [Table/Fig-1]. 47,XXY karyotype (Klinefelter syndrome) [Table/Fig-6] was most prevalent and other abnormal karyotype 47,XYY, 46,XYq-, 46,XX and one autosomal reciprocal translocation were also noted [Table/Fig-2,3].
The karyotype showing 47, XXY Klinefelter syndrome in a infertile male.
Ambiguous genitalia: Cytogenetic analysis of 72 suspected cases confirmed 6 (8.33%) abnormal karyotypes. Karyotype analysis revealed that 3 cases had different types of mosaic karyotypes and 3 cases had structural aberrations [Table/Fig-2].
Congenital anomalies: Of the 147 cases of congenital developmental abnormality, 13 (8.84%) cases had cytogenetic abnormalities. Four cases showed autosomal trisomy involving chromosome 13 or 18 and other 9 cases had different kinds of structural abnormalities [Table/Fig-2].
Psychiatric disorder: Psychiatric disorders of 30 cases were karyotyped and only 2 (6.66%) cases showed abnormal karyotypes. One abnormal karyotype with structural abnormalities having translocation of 13;14 chromosome and another one having numerical aberrations with a marker chromosome [Table/Fig-1,2].
Discussion
Numerical and structural chromosomal abnormalities are responsible for human genetic diseases or disorder. Many disorders like different kinds of syndrome, primary amenorrhea, recurrent abortions, male infertility, and abnormal sexual development are caused due to numerical or structural chromosomal aberrations [2]. A total of 2215 clinically suspected referred cases were evaluated for cytogenetic analysis to rule out chromosomal abnormalities. The overall incidence of cytogenetic abnormalities was found in 271 (12.23%) suspected cases [Table/Fig-1]. Out of 271 patients, 204 (75.27%) cases had numerical chromosomal abnormalities followed by structural abnormalities 67 (24.72%) cases [Table/Fig-2]. Present study data is on the same line with previous studies which had reported the prevalence, and types of chromosomal abnormalities in the cases suspected with genetic disorders [1,2,4,11]. In this study, the referred patients were classified in seven different groups on the basis of their clinical phenotypes reported by clinicians.
Down Syndrome
Down syndrome was characterised clinically in 1866 and genetic basis of the syndrome was understood 1959. Down syndrome is the most prevalent autosomal (chromosome # 21) disorder with a global incidence of 1 in 700 live births. Down syndrome patients suffer from systemic disorders to mental retardation with a distinct and typical phenotype [12]. The meiotic non-disjunction results in the origin of extra 21 in 95%, where as de-nova Robertsonian translocation of various types like t (13;21), t (14;21), t (15,21), or hereditary t (21;21) and mosaic karyotypes contribute to the remaining 5%. Translocation in Down syndrome can be de novo in origin that occurred at the time of conception due to abnormal parental gametogenesis or inherited from a parent carrying Robertsonian translocation [6,13].
The present study indicated that Down syndrome was the most common chromosomal disorder. One hundred and fifty two cases (92.68%) had free trisomy 21 that caused Down syndrome either girl or boy followed by translocations of 13;21, 14;21 or 21;21 in 10 (6.10%) cases. Translocation of 21;21 in 1 (0.61%) case was observed and only 1 (0.61%) Down syndrome patient showed mosaic karyotype [Table/Fig-3]. The study noted a very unusual and rare reciprocal translocation involving chromosome 9 and 21 in one referred and cytogenetically confirmed Down syndrome patient [Table/Fig-4]. Present study finding supports the previous studies reported cytogenetic analysis of Down syndrome cases with higher percentage of free trisomy 21 (95%) followed by translocation type of Down syndrome, hereditary type and mosaic case contribute to the remaining 5% [14]. This syndrome is caused by paternal meiotic error in 10-20% cases while rest is contributed by the mother, probably the advanced maternal age (>35 years) [15].
Primary Amenorrhea
Primary amenorrhea is the failure of menses and subjects do not attain menarche by the age of 16 years. Sex chromosomal abnormality is the most important cause of primary amenorrhea [16]. Cytogenetic studies of primary amenorrhea suggest that there is a relationship between the primary amenorrhea and abnormal karyotype involving sex chromosomes and the changes of sex chromosome may be structural or numerical [17].
Primary amenorrhea is caused by several genetic and non-genetic factors in female [16]. Chromosomal abnormalities causing Turner syndrome, sex reversal female, androgen insensitivity syndrome are the most important causes of primary amenorrhea [18]. The frequency of abnormal karyotypes in primary amenorrhea varies in between 10% to 25% [11]. The present study revealed 36 (9.40%) primary amenorrhea cases having chromosomal anomalies with numerical and structural abnormalities [Table/Fig-1]. Distribution of pure Turner syndrome, Turner syndrome with structural anomalies of X chromosome and mosaic Turner’s syndrome, primary amenorrhea with 46,XY karyotype, sex reversal and complete androgen insensitivity syndrome have been depicted [Table/Fig-2]. The percentages of different types of abnormal karyotypes encountered in primary amenorrhea cases are shown in [Table/Fig-3]. Interestingly, sex reversed female and androgen insensitivity syndrome cases with 46,XY karyotype were the high and leading percentages (44.44%). Rajasekhar M et al., reported higher proportion of mosaics Turners syndrome than the classic Turners syndrome and Duarte AC et al., also reported most common Turners syndrome mosaic than classical monosomy 45,X [19,20]. The present findings also suggest that mosaic karyotype of Turner syndrome is more than the classical monosomy (45,X). Sex chromosomal anomalies are one of the major aetiological factors for primary amenorrhea cases. The present study indicated that karyotype analysis of all primary amenorrhea or suspected cases is essential for correct diagnosis and counseling.
Recurrent Pregnancy Loss
Three or more consecutive pregnancy losses before 20 weeks of gestation are known as recurrent pregnancy loss. Worldwide, recurrent pregnancy loss affects near about 10%-15% couples of all clinically recognised pregnancies [21]. Chromosomal anomalies affect nearly 2%-8% of couples with recurrent pregnancy loss [22].
The chromosomal abnormality is one of the important causes of recurrent pregnancy loss in married couples. The genetic factors including cryptic chromosomal abnormality, monogenic mutation, genomic imprinting, and inactivation of X chromosome are elucidating idiopathic cause of recurrent pregnancy loss in couple [23]. Around 15-20% of human pregnancies have been terminated spontaneously up to first trimester, and chromosomal anomalies are responsible for recurrent pregnancy loss in 50% cases in developing foetus [21]. Out of 384 recurrent pregnancy loss couples (768 male and female individuals), the study found 20 (2.60%) chromosomal anomalies in one of the partners of the couple [Table/Fig-1]. There were four types of chromosomal aberrations namely reciprocal translocation, Robertsonian translocation, inversion, and numerical anomalies in the pregnancy loss cases [Table/Fig-2]. The numerical and structural chromosomal aberrations were observed 10% and 90% in the recurrent pregnancy loss group respectively. Balanced reciprocal translocation (50%) is the main cause of chromosomal anomalies in recurrent pregnancy loss. In the present study, frequency of structural chromosomal anomalies is significantly much higher in recurrent pregnancy loss than numerical anomalies [Table/Fig-3]. The carriers of the balanced reciprocal translocation [Table/Fig-5] produce abnormal gametes and the embryos produce by these abnormal gametes are aborted [24,25]. The studies on chromosomal anomalies will help to rule out the possible genetic causes of recurrent pregnancy loss. The chromosomal analysis helps in genetic counseling and appropriate management of the couples with recurrent pregnancy loss.
Male Infertility
Now-a-days, infertility is a major reproductive health problem. Globally, 15% couples are infertile and both infertile males and females are in equal proportion i.e., around 50% of infertile cases cause is attributed to male partners [26]. Many genetic and non-genetic aetiological conditions including chromosomal aberrations or genetic mutations have been identified for male infertility [27]. Many infertile males have altered seminal parameters such as oligozoospermia, azoospermia, asthenozoospermia or Oligoasthenoteratozoospermia (OAT) [28]. There are intricate genetic and complex endocrine factors, which are highly coordinated and synchronised to govern normal spermatogenesis. Failure of these regulatory events is a possible cause of abnormal spermatogenesis [29]. Genes controlling spermatogenesis are present on both sex chromosomes and autosomes. Structural and numerical aberrations of sex chromosomes disturb the spermatogenesis [27]. Y chromosome holds the key for spermatogenesis as there are genes namely RBM genes, DAZ genes and some other genes on Y chromosome which are responsible for normal spermatogenesis. All the genes come into action in different phase of spermatogenesis cascade. Microdeletions or mutations in Y chromosome genes results in abnormal spermatogenesis and male infertility [30].
In the retrospective study 473 infertile males were referred for cytogenetic analysis. Out of 473 infertile azoospermic and oligozoospermic males, the study found 30 (6.34%) infertile males with various type of chromosomal abnormalities [Table/Fig-1,2 and 3] including Klinefelter syndrome (47,XXY) [Table/Fig-6], patients with karyotype 47,XYY, Yq deletion karyotype (46,XYq-) and sex reversal male (46,XX), 46,X,inv(Y). Autosomal reciprocal translocation, t(1q;22q), only in one oligozoospermic males was noted. Recent studies showed that the 47,XYY karyotype may be associated with altered meiotic segregation, resulting in sperm apoptosis and necrosis, leading to sub-fertility or infertility in male [28]. In the Yq arm deleted infertile males, spermatogenesis specific AZF regions were deleted and it leads to azoospermic or severe oligozoospermic condition. In Y inversion cases, the spermatogenesis controlling regions (AZF) region in q arm of Y chromosome is disturbed and give rise to azoospermic and abnormal spermatogenesis [30]. The translocated type of karyotype hampered the normal gametogenesis process and may be associated with altered meiotic segregation which may be responsible for abnormal sperm count [25].
Ambiguous Genitalia
The incidence of genital ambiguity that results in the child’s sex being uncertain is 1 per 4500 [31]. An understating of sex determination and differentiation is essential to take appropriate investigation for the proper diagnosis, treatment, and counseling [32]. The development of external or internal genital tracts is very much under the strict control of genetic cascade and hormonal pathways [33]. Defects in the genetic or hormonal pathways including gene mutations or chromosome aberrations, in appropriate hormone levels or end organ unresponsiveness may results in genital ambiguity [31].
Abnormal sexual differentiation pathway formed intersexuality due to chromosomal abnormality or gene mutation in sex differentiation genes [34]. Male or female pseudohermaphroditism and hermaphroditism is the ideal example of ambiguous genitalia. Ambiguous genitalia has found in live birth child due to structural genetic abnormality or mosaicism of sex chromosome [35]. In the present study, out of 72 referred cases of ambiguous genitalia, 6 (8.33%) had chromosomal abnormality [Table/Fig-1]. Among 6 cases of genetic abnormalities, 3 cases had mosaic karyotype involving sex chromosome and 1 case had 46,XX,der(9) and other 2 cases had 46,XX karyotype suggesting sex reversal conditions [Table/Fig-2,3]. Remaining 66 cases with normal karyotypes might have sex chromosomal or autosomal gene mutations which were responsible in phenotypic and sexual differentiations.
Congenital Anomalies
Congenital anomalies are important causes for infant mortality and they remain a leading cause of death among infants all over the world [36]. Chromosome abnormalities account for nearly 15% of the major congenital anomalies and are associated with 25% of perinatal deaths due to congenital anomalies [37]. The most common chromosome abnormalities showing congenital anomalies in live birth babies are trisomy of chromosome 21, 18, 13 and also sex chromosomal abnormalities [38]. Children with sex chromosome abnormalities may not have any problem requiring investigation in childhood but they may need investigation later in life during adolescent period or reproductive phase. Besides trisomies of chromosome 21, 18, and 13 and sex chromosome abnormalities, unbalanced translocations, deletions and duplication are also very much prevalent in congenital anomalies cases [39].
Congenital malformations occur across the globe and are responsible for about 15% of the perinatal mortality in India [39]. Out of 147 cases of congenital anomalies included in the study, 13 (8.84%) had numerical or structural cytogenetic abnormalities [Table/Fig-1,2]. A number of parents having babies with congenital anomalies were married consangiounsly [40]. Chromosomal abnormalities and autosomal recessive traits were mostly involved in congenital anomalies in child [38]. In the present study, autosomal trisomies of chromosomes 13 and 18 were observed in congenital abnormal neonatal babies. Structural chromosomal anomalies of inversion and translocation types had been observed in 9 cases of congenital abnormalities. An incidence of 14.64 per 1000 births with congenital anomalies is reported in a survey of over 4000 births with various types of structural and numerical chromosomal aberrations [37].
Psychiatric Disorders
Psychiatric disorder affects 2.5-3.0% of the total population in our society [41]. Possibly, chromosomal abnormalities or genetic mutations are one of the important causative factors for mental retardation [42]. Cytogenetic investigations of 30 referred mentally challenged patients were done and suspected child cases such as Down syndrome, delayed milestones, mental retardation were not included. Chromosome analysis confirmed that only 2 (6.66%) female cases with unusual and interesting karyotypes, one with 47,XX,+small marker (dot like) chromosome and another one with 45,XX,t(13;14) [Table/Fig-2]. The role of this translocation with psychiatric disorder is difficult to justify.
Indian studies have shown variations in the frequencies of chromosomal abnormalities in clinically suspected cases and variations in the percentages of chromosomal abnormalities may be due to different types of referred patients and number included in the studies [Table/Fig-7] [3,7,11,13,19,25,36,42].
Indian studies showing frequencies chromosomal abnormalities in clinically suspected cases [3,7,11,13,19,25,36,42].
| Authors | % of Chromosome abnormalities | Types of suspected cases included in the study |
|---|
| Moghe M et al., 1981 [42] | 24.5% (74/306) | Mentally retarded children |
| Rajasekhar M et al., 2010 [19] | 24.5% (343/1400) | Primary amenorrhea, Down syndrome, Recurrent pregnancy loss, Infertility, etc. |
| Datta UR et al., 2013 [11] | 20.7% (132/637) | Primary amenorrhea |
| Sheth F et al., 2015 [36] | 7.2% (125/1728) | Prenatal genetic diagnosis |
| Sudhir N et al., 2016 [25] | 3.41% (15/440) | Recurrent pregnancy loss |
| Polipalli SK et al., 2016 [13] | 43.1% (371/859) | Down syndrome, Turner syndrome, Sex development disorder, Intellectual disabilities. |
| Kalotra V et al., 2017 [3] | 3.1% (15/243) | Recurrent pregnancy loss |
| Pal AK et al., 2018 [7] | 9.88% (17/172) | Primary amenorrhea |
| Present study | 12.3% (271/2215) | Down Syndrome, Primary amenorrhea, Recurrent pregnancy loss, male infertility, Ambiguous, congenital abnormalities, psychiatric disorders |
Limitation(s)
Cytogenetic analysis cannot identify the changes at molecular level or mutations which can be done only by molecular genetic analysis. Therefore, this is beyond the scope and it is limitation of the present study.
Conclusion(s)
Cytogenetic analysis is essential for diagnosis of genetic diseases and also for estimation the risk of recurrence of the genetic disorders. Chromosomal analysis helps in genetic counseling to decide about the clinical management and future pregnancies. The cytogenetic data is useful to clinicians and other health care providers for purposes of counseling. The genetic counseling can help families to cope with emotional, psychological and medical consequences of genetic diseases. Consanguineous marriage is an important risk factor for congenital anomalies and the frequency of which may be reduced by creating awareness regarding its avoidance. The facilities for catering the genetic diagnostic services are less in developing countries. The efficient registries, databases on genetic basis of diseases and continued investment in genetic research are key to successful public health interventions.
*F: Female; #M: Male
Grand total (Numerical + Structural) 204+67=271