Complication of Rubber Band Ligation in Second and Third Degree Haemorrhoids
Aditya Ashwani Rajkumar Mehta1, Yashwant Lamture2
1 Junior Resident, Department of Surgery, Jawaharlal Nehru Medical College, Wardha, Maharashtra, India.
2 Professor, Department of Surgery, Jawaharlal Nehru Medical College, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Yashwant Lamture, Jawaharlal Nehru Medical College, Wardha, Maharashtra, India.
E-mail: dryrlamture@yahoo.co.in
Introduction
Haemorrhoids or piles are symptomatic anal cushions. They can be classified as 1st degree (only bleed), 2nd degree (prolapse but reduce automatically), 3rd degree (prolapse and requires manual reduction) and 4th degree (permanent prolapsed). Haemorrhoids can be managed either conservatively by regular sitz bath, dietary modifications and medications etc., or by minimal invasive procedures like Rubber Band Ligation (RBL), excising and whitehead haemorrhoidectomy. RBL is the most common non surgical and outpatient modality performed, as it is a safe, effective and easier to execute, it is being advised as an Outpatient Department (OPD) procedure.
Aim
To study the complications of RBL in 2nd and 3rd degree haemorrhoids.
Materials and Methods
The study was conducted as a prospective interventional study at Department of Surgery. The study population consisted of 50 cases of second and third degree haemorrhoids, who underwent RBL as a outpatient procedure. Post-operative complication were studied. Statistical analysis was done using descriptive and inferential statistics through chi-square test. SPSS software 24.0 version and Graph Pad Prism 7.0 version were used in the analysis. Level of significance was considered as less than 0.05.
Results
Total 84% had 2nd degree haemorrhoids and 16% had 3rd degree haemorrhoids. The study showed an overall higher success rate (94%) of RBL procedure for 2nd and 3rd degree haemorrhoids; recurrence rate after RBL was 6% (3 patients), when followed-up for a period of 6 weeks The most common complication was pain (62%) followed by urinary retention (8%). The post RBL pain was significantly higher in the 2nd degree haemorrhoids.
Conclusion
RBL is an effective, safe outpatient procedure but the complications are more in 3rd degree when compared to 2nd degree haemorrhoids.
Haemorrhoidectomy, Pelvic infection, Post RBL bleeding, Urinary retention
Introduction
Haemorrhoids or piles are symptomatic anal cushions [1]. Degree of haemorrhoids can be classified as 1st degree (only bleed), 2nd degree (prolapse but reduce automatically), 3rd degree (prolapse and requires manual reduction) and 4th degree (permanent prolapsed). The approach in treatment of haemorrhoids has significantly changed in the past few decades [2].
Haemorrhoids can be managed either conservatively by regular sitz bath, dietary modifications and medications etc., or by minimal invasive procedures like RBL, sclerotherapy, cryotherapy, diathermy using bipolar, coagulation by Infrared rays or Laser, dilatation of anal region, ultroid and treatment with diode laser [3].
RBL is the most common non surgical and outpatient modality performed. As it is a safe, effective and easier to execute, it is being advised as an OPD procedure [3]. RBL was first described by Blaisdell in 1954. It was popularised by Barron in 1963 and now considered to be the most popular outpatient treatment for symptomatic internal haemorrhoids. RBL has low complication and is effective when compared to operative procedure. Recurrent internal haemorrhoids are also treated using RBL [4].
RBL is the most commonly used feasible, minimally invasive procedure, representing a balance between efficacy, pain and potential of complications [5] with success rate from 69 percent to 97 percent irrespective of the problems that are associated with surgical procedures [6]. The minor complications of RBL commonly consists of blood loss, pain, vasovagal reflex, slipping of the bands, urinary retention and long standing ulcers (vertical) [7]. Marshman D et al., found that the complication rate of RBL increases when multiple ligations are performed in one session [8]. The life threatening complication of RBL is pelvic sepsis.
At present there are two scenarios in context to RBL; one scenario shows minor complications whereas the other shows life threatening complications. Hence, the present study was conducted to compare both major as well as minor complications of RBL in Indian population having second and third degree haemorrhoids simultaneously.
Materials and Methods
This prospective interventional study was conducted after the approval of the Ethical Committee (DMIMS (DU)/IEC/2017-18/6646), in the Department of Surgery, Jawaharlal Nehru Medical College, Deemed University, Sawangi (Meghe) from September 2017 to July 2019. Written consents were obtained from all the patients.
Sample Size Calculation [
9]
Where,
P=overall success rate (88.6%);
L=Allowable error (11.5% of p=9.959);
q=100-p (13.4)
The sample size was 50. All patients of 2nd and 3rd degree internal haemorrhoids were included in the study. Patients with 1st and 4th degree haemorrhoids, thrombosed haemorrhoids, inflammatory bowel disease, blood dyscriasis, haemorrhoids with rectal prolapsed and infected haemorrhoids were excluded.
Patients presenting with complaint of bleeding per rectum were thoroughly evaluated by complete physical examination, including per rectal examination and proctoscopy. The possible complications were explained and RBL was performed after taking informed consent. The base of the haemorrhoids was clearly visualised and band applied above the dentate line.
The details of procedure included proctoscopy to which pen torch was attached to provide illumination thereby displaying haemorrhoids. Initially, the instrument was washed and treated with 2% gluteraldehyde solution for 20 minutes before using in each patient [10]. Each haemorrhoid trunk was then caught above the dentate line with a pre-loaded baron band ligator.
After procedure, patient was kept under observation for 6 hours for complaint of pain, bleeding and other complications like vasovagal reflex, urinary retention, slippage of band. Patient was also observed for pelvic infection. Patient was followed-up till 6 weeks for success and recurrence [9]. Pain was measured using Visual Analogue Scale (VAS). The minimum score was 0 and maximum score 6 in the study- 0: denoted no pain corresponding to VAS of 0 mm; 2-4: Mild pain corresponding to VAS of 1-40 mm; 6: Moderate pain corresponding to VAS of 41-60 mm; 8: Severe pain corresponding to VAS of 61-80 mm; and 10: Very severe Pain corresponding to VAS of 81-100 mm. Patients with severe and very severe pain were not taken into the study.
Success in a patient was defined as patient being completely asymptomatic for 6 weeks after the procedure with no evidence of haemorrhoids noted on proctoscopy whereas, recurrence was defined as symptomatic patients with evidence of haemorrhoids on proctoscopy 6 weeks after rubber band application [9].
The event of bleeding was controlled by using appropriate medicines Tranexamic acid 10 mg/kg body weight. Pain was controlled with appropriate medicines like Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) like Paracetamol 500 mg BD.
Statistical Analysis
Statistical analysis was done by using descriptive and inferential statistics through chi-square test. SPSS software 24.0 version and Graph Pad Prism 7.0 version was used in the analysis. Level of significance was considered as less than 0.05.
Results
Maximum number of patients was seen between the age group of 41 to 50 years [Table/Fig-1]. Out of 50 patients 35 were males and 15 were females. Male:Female ratio was 2.3:1. Out of the 50 patients, 84% had 2nd degree haemorrhoids and 16% had 3rd degree haemorrhoids.
Age wise distribution of patients.
| Age group (Year) | No of patients | Percentage |
|---|
| ≤20 | 5 | 10 |
| 21-30 | 6 | 12 |
| 31-40 | 9 | 18 |
| 41-50 | 12 | 24 |
| 51-60 | 8 | 16 |
| 61-70 | 6 | 12 |
| 71-80 | 3 | 6 |
| >80 | 1 | 2 |
| Total | 50 | 100 |
| Mean±SD | 45.50±17.71(16-86 years) |
SD: Standard deviation
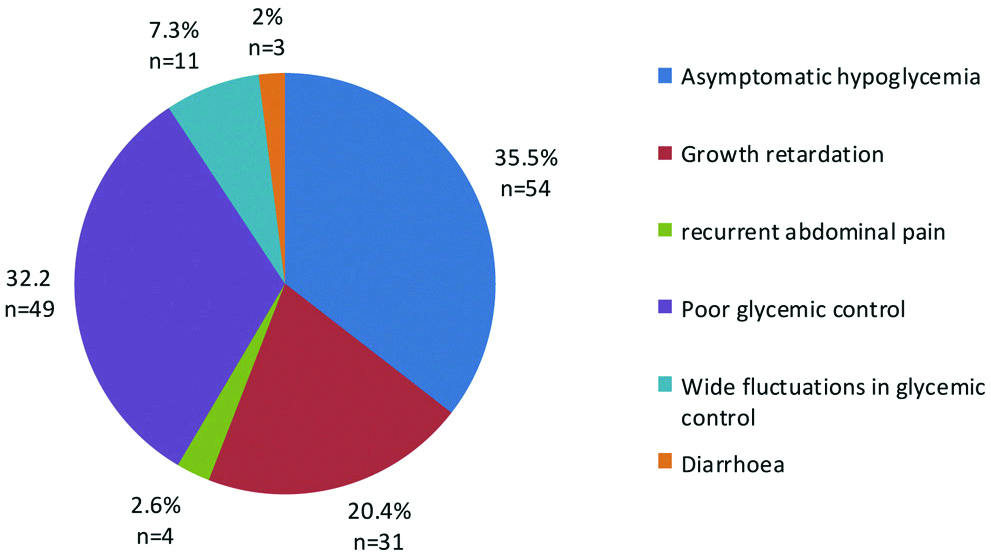
Complications in Patients after RBL
a. Post RBL Bleeding
Out of 50 patients, bleeding was present in three patients at 6 weeks post-procedure. Out of the three patients, one (2%) patient had 2nd degree haemorrhoids and two (4%) patients had 3rd degree haemorrhoids (χ2=6.09 and p-value=0.01).
b. Pain after RBL
Pain after RBL was assessed by Visual Analogue Scale at 6 weeks post-procedure and given an appropriate scoring. The minimum score was 0 and maximum score 6 [Table/Fig-2]. Post RBL the patients experience either no pain, mild pain or moderate pain.
Pain score according to degree of haemorrhoids.
| Pain score | Degree of haemorrhoids | χ2-value | p-value |
|---|
| 2nd degree | 3rd degree |
|---|
| 0 | 18 (36%) | 1 (2%) | 10.52 | 0.014 |
| 2 | 1 (2%) | 1 (2%) |
| 4 | 16 (32%) | 1 (2%) |
| 6 | 7 (14%) | 5 (10%) |
| Total | 42 (84%) | 8 (16%) |
Other Complications after RBL
The most common complication seen was urinary retention and the incidence was same in patients with both 2nd and 3rd degree haemorrhoids. Out of 50 patients, none of the patients suffered from any pelvic infection [Table/Fig-3].
Other complications according to degree of haemorrhoids.
| Other complications | | Degree of haemorrhoids | χ2-value | p-value |
|---|
| 2nd degree | 3rd degree |
|---|
| Urinary retention | Present | 2 (4%) | 2 (4%) | 3.73 | 0.053 |
| Absent | 40 (80%) | 6 (12%) |
| Slippage of band | Present | 0 (0%) | 1 (2%) | - | - |
| Absent | 42 (84%) | 7 (14%) |
| Vasovagal reflex | Present | 0 (0%) | 0 (0%) | - | - |
| Absent | 42 (84%) | 8 (16%) |
NS: Non-significant
Treatment Modalities to Manage Complications
Most of the complications post RBL were managed conservatively, either by NSAID’s like Paracetamol 500 mg BD, Tranexamic acid 10 mg/kg body weight given twice daily for 3 days and then SOS or by temporary Foley’s catheterisation. Re-Banding was required only in 2% of the patients [Table/Fig-4].
Treatment modalities to manage complications.
| Treatment modalities | | Number of patients |
|---|
| Medical Management for bleeding (Tranexamic acid 10 mg/kg body weight given twice daily for 3 days and then SOS) | Required | 3 (6%) |
| Not required | 47 (94%) |
| Pain killer (NSAIDS: Paracetamol 500 mg BD) | Present | 11 (22%) |
| Absent | 39(78%) |
| Catheterisation for urinary retention | Present | 4 (8%) |
| Absent | 46 (92%) |
| Re-banding | Present | 1 (2%) |
| Absent | 49 (98%) |
Outcome
Urinary retention is the inability to completely or partially empty the bladder and was recorded in 1st week after procedure. Vasovagal reflex is defined as sudden drop in the heart rate and blood pressure leading to fainting and was observed during the procedure. Slippage of band was assessed at 6 weeks post-procedure. Out of 50 patients, success rate of RBL was 94% (47 patients) and recurrence rate after RBL was 6% (3 patients), when followed-up for a period of 6 weeks.
Discussion
Various post RBL complication encountered by the patients in 2nd degree and 3rd degree haemorrhoids were studied. The most common complication experienced by the study population was pain (62%) which is consistent with many other studies as mentioned in [Table/Fig-5] [5,14-18]. Urinary retention (8%) is the second most common co complication experienced by the study population as shown in [Table/Fig-5] [9,18]. There were no cases showing life threatening complications like vasovagal reflex [3,19] and pelvic infections [3] in the study as well as some other studies mentioned in [Table/Fig-5] [2,3,5,9,11-20].
Complications of Rubber Band Ligation seen in various studies [2,3,5,9,11-20].
| Total patients | Post RBL bleed | Post RBL pain | Urinary retention | Slippage of band | Vasovagal reflex | Pelvic infection |
|---|
| Present study | 50 | 6% | 62% | 8% | 2% | 0% | 0% |
| El Nakeeb AM et al., [11] | 750 | 4.13% | - | - | - | - | - |
| Aram FO [3] | 890 | - | - | - | - | 0.6% | 0.1% |
| Forlini A et al., [12] | 206 | 2.4% | - | - | - | - | - |
| Hadi A et al., [13] | 105 | 3.8% | - | - | - | - | - |
| Nikam V et al., [9] | 60 | 16.6% | - | 6.7% | - | - | - |
| Azizi R et al., [14] | 60 | - | 62% | - | - | - | - |
| Watson NFS et al., [15] | 183 | - | 90% | - | - | - | - |
| Hardwick RH and Durdey P, [16] | 52 | - | 81% | - | - | - | - |
| Kotzampassi K [5] | 87 | - | 31.2% | - | - | - | - |
| Kumar N et al., [17] | 98 | - | 24.5% | - | - | - | - |
| Khaliq T et al., [18] | 56 | - | 13% | - | - | - | - |
| Chandra B et al., [19] | 100 | - | - | 5% | - | 0% | - |
| Ratan R and Rao PP, [2] | 100 | - | - | - | 0% | - | - |
| Bat L et al., [20] | 512 | - | - | - | 1% | - | - |
Like many other studies [2,20], the present study also showed a higher success rate (94%) of RBL procedure for 2nd and 3rd degree haemorrhoids [Table/Fig-2] and lower recurrence (6%) of complications of RBL procedure for 2nd and 3rd degree haemorrhoids [Table/Fig-6] [2,20].
Comparison of success rate of Rubber band ligation and recurrence of complications of Rubber band ligation [2,20].
Limitation(s)
The follow-up period in this study was 6 weeks. The study was a single centre study and the sample size was less, hence might have an impact on the outcome of study.
Conclusion(s)
Post RBL bleeding was more in third degree haemorrhoids. The success rate in this study was 94% at six weeks. To conclude, RBL is safe, outpatient procedure in second and third degree haemorrhoids with low rate of recurrence.
SD: Standard deviation
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 17, 2019
Manual Googling: Apr 02, 2020
iThenticate Software: Apr 15, 2020 (8%)
[1]. Williams NS, Connell PR, McCaskie AW, Bailey and Love’s Short Practice of Surgery 2018 27th EditionTaylor and Francis Group:1355 [Google Scholar]
[2]. Ratan R, Rao PP, Rubber band ligation in early stage hemorrhoids: Outcome & efficacy in today’s eraInternational J of Healthcare and Biomedical Research 2018 6(2):66-72. [Google Scholar]
[3]. Aram FO, Rubber band ligation for hemorrhoids: An office experienceIndian J Surg 2016 78(4):271-74.10.1007/s12262-015-1353-127574343 [Google Scholar] [CrossRef] [PubMed]
[4]. Lee HH, Spencer RJ, Beart RWJr, Multiple hemorrhoidal bandings in a single sessionDis Colon Rectum 1994 37(1):37-41.10.1007/BF020472128287745 [Google Scholar] [CrossRef] [PubMed]
[5]. Kotzampassi K, Rubber band ligation of haemorrhoids- An Office ProcedureAnnals of Gastroenterology 2003 16(2):159-61. [Google Scholar]
[6]. Iyer VS, Shrier I, Gordon PH, Long-Term outcome of rubber band ligation for symptomatic primary and recurrent internal haemorrhoidsDis Colon Rectum 2004 47(8):1364-70.10.1007/s10350-004-0591-215484351 [Google Scholar] [CrossRef] [PubMed]
[7]. Albuquerque A, Rubber band ligation of hemorrhoids: A guide for complicationsWorld J Gastrointest Surg 2016 8(9):614-20.10.4240/wjgs.v8.i9.61427721924 [Google Scholar] [CrossRef] [PubMed]
[8]. Marshman D, Huber PJ Jr, Timmerman W, Simonton CT, Odom FC, Kaplan ER, Hemorrhoidal ligation. A review of efficacyDis Colon Rectum 1989 32(5):369-71.10.1007/BF025636832714125 [Google Scholar] [CrossRef] [PubMed]
[9]. Nikam V, Deshpande A, Chandorkar I, Sahoo S, A prospective study of efficacy and safety of rubber band ligation in the treatment of Grade II and III haemorrhoids- A western Indian experienceJ Coloproctol (RIO J) 2018 38(3):189-93.10.1016/j.jcol.2018.03.006 [Google Scholar] [CrossRef]
[10]. Cowan RE, Cleaning and disinfection of equipment for gastrointestinal endoscopy. Report of a working party of the British Society of Gastroenterology Endoscopy CommitteeGut 1998 42(4):585-93.10.1136/gut.42.4.585 [Google Scholar] [CrossRef]
[11]. El Nakeeb AM, Fikry AA, Omar WH, Fouda EM, Metwally TAE, Ghazy HE, Rubber band ligation for 750 cases of symptomatic hemorrhoids out of 2200 casesWorld J Gastroenterol 2008 14(42):6525-30.10.3748/wjg.14.652519030206 [Google Scholar] [CrossRef] [PubMed]
[12]. Forlini A, Manzelli A, Quaresima S, Forlini M, Long-term result after rubber band ligation for haemorrhoidsInt J Colorectal Dis 2009 24(9):1007-10.10.1007/s00384-009-0698-y19387663 [Google Scholar] [CrossRef] [PubMed]
[13]. Hadi A, Aman Z, Anwar F, khan M, Iqbal Z, Experience of rubber band ligation for haemorrhoidal diseasePak J Med Res 2011 50(3):104-07. [Google Scholar]
[14]. Azizi R, Rabani-Karizi B, Taghipour MA, Comparision between Ultroid and rubber band ligation in treatment of internal haemorrhoidsActa Med Iran 2010 48(6):389-93. [Google Scholar]
[15]. Watson NFS, Loptrott S, Maxwell-Armstrong CA, A prospective audit of early pain and patient satisfaction following out-patient band ligation of haemorrhoidsAnn R Coll Surg Engl 2006 88(3):275-79.10.1308/003588406X9864916719998 [Google Scholar] [CrossRef] [PubMed]
[16]. Hardwick RH, Durdey P, Should rubber band ligation of haemorrhoids be performed at the initial outpatient visit?Ann R Coll Surg Engl 1994 76(3):185-87. [Google Scholar]
[17]. Kumar N, Paulvannan S, Billings PJ, Rubber band ligation of haemorrhoids in the out-patient clinicAnn R Coll Surg Engl 2002 84(3):172-74. [Google Scholar]
[18]. Khaliq T, Shah SA, Mehboob A, Outcome of rubber band ligation of haemorrhoids using suction ligatorJ Ayub Med Coll Abbottabad 2004 16(4):34-37. [Google Scholar]
[19]. Chandra B, Karthik KS, Kumari S, Suman RK, An evaluation of the effectiveness of barron band ligation as a modality of treatment of hemorrhoidsIOSR-JDMS 2014 13(10):39-46.10.9790/0853-131013946 [Google Scholar] [CrossRef]
[20]. Bat L, Melzer E, Koler M, Dreznick Z, Shemesh E, Complications of rubber band ligation of symptomatic internal hemorrhoidsDis Colon Rectum 1993 36(3):287-90.0.1007/BF020535128449135 [Google Scholar] [CrossRef] [PubMed]