Hypoalbuminemia has been shown to be associated with increased mortality and morbidity rates in both hospitalised patients and community dwelling elderly persons. In surgery, an association between hypoalbuminemia and adverse outcome has been recognised for many years [1-4]. It is common and occurs in about 30% of surgical patients with GI diseases and in up to 60% of those in whom hospital stay has been prolonged because of post-operative complications.
Patients with malnutrition have a higher risk of complications and an increased risk of death [5,6]. A dietary history, physical examination (including anthropometric measurements), and relevant laboratory investigations are required to know a patient’s pre-operative nutritional status.
The serum albumin level is the most readily available and clinically useful parameter. A serum albumin level >3 gm/dL suggests adequate protein stores. It predicts perioperative morbidity and mortality [6]. Serum albumin is the most important laboratory test for the diagnosis of protein-calorie undernutrition. Most patients with severe protein depletion have low serum albumin levels that would correspond to poor clinical outcomes [7].
The major risk factors that have been commonly studied in relation to the adverse post-operative outcomes in laparotomy patients are intra-abdominal sepsis, old age, obesity, co-morbidities like Diabetes Mellitus, Coronary Artery Disease, Jaundice and Pulmonary Diseases [8-12].
Serum albumin is a good indicator of presence and degree of malnutrition and thus an indirect indicator of surgical risk. Hypoalbuminemia causes delayed recovery of bowel function and thus is strongly associated with post-operative complications after surgeries for colonic pathologies and other major GI surgery [13-15]. The role of albumin in maintenance of homoeostasis is well known but the mechanism of its deficiency and the harmful effects of the same in critically ill patients especially who have undergone major surgery like laparotomies have not been well understood till now. In hypoalbuminemic patients, wound infection, remote infections (pneumonia, anastomotic leakage), are commonly found [8,11,15,16].
Current indication for nutritional support before elective surgery include a history of weight loss in excess of 10% of body weight or an anticipated prolonged post-operative recovery period during which the patient will not be fed orally [17].
This study tried to determine the relationship between hypoalbuminemia and the development of complications following laparotomy for GI diseases for both emergency and elective surgeries. The rate of mortality related to hypoalbuminemia was also studied.
Materials and Methods
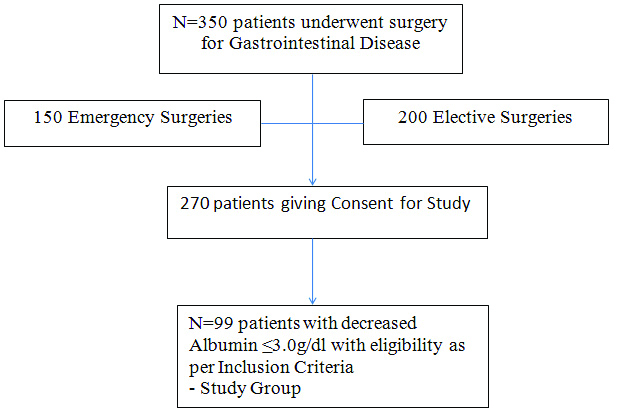
This prospective cross-sectional study was conducted in a Rural Medical College in Central India for the period between November 2013 and October 2015. The institutional ethical committee approved the study (2013/07-3). A written informed consent was taken from all the study participants.
The following assessments were done on the study participants:
Pre-operative Evaluation of Serum Albumin for Gastrointestinal Disease on Emergency Basis and Elective Surgeries.
Nutritional Assessment (Mid Upper Arm Circumference, Skin Fold Thickness) along with BMI.
Post-operative Evaluation of Serum Albumin after 48 hours and 7 day.
Study of the association of hypoalbuminemia with post-operative morbidities were divided into Early Post-operative which included complications within 30 days post-operative and late post-operative complications which were determined at follow-up of the patients. The early post-operative complications included: Systemic Sepsis, Acute Renal Failure, Ventilatory Support, Bleeding/Transfusion, Myocardial Infarction, Pneumonia (LRTI), Urinary Infection, Pulmonary Oedema, Pleural Effusion, SSI, Wound Dehiscence, Prolonged Ileus, Pulmonary Embolism, Biliary Fistula, Fecal Fistula, Deep Vein Thrombosis (DVT) and Thrombophlebitis, Cardiac Arrest, Prolonged Hospital Stay, Burst Abdomen and Adult Respiratory Distress Syndrome (ARDS). Late post-operative complications included Incisional Hernia, Para-stomal hernia and Re-operation along with other above mentioned complications.
Study of the association of hypoalbuminemia with post-operative mortality was also studied [Table/Fig-1].
Inclusion Criteria:
Age >18 years.
Patients having pre-operative serum albumin <3 gm/dL.
Patients who underwent Emergency Laparotomy for GI Diseases in Tertiary Care Rural Hospital during November 2013 and October 2015.
Exclusion Criteria:
Patients having normal albumin levels and ≥3.0 gm/dL was taken as normal value for present study.
Patients who had Chronic Liver Disease and Jaundice, Sepsis (WBC>12,000 cells/mm3), Severe Anaemia with Hb <8 gm/dL, Diabetes Mellitus Type II, Chronic Renal Disease, Patients on Steroids or Chemotherapy or any other Hepatotoxic Drugs and Clinically significant signs and symptoms of hypoalbuminemia.
BMI <12 and >40 were excluded from the study.
Patients with prolonged addiction to alcohol and tobacco were excluded.
Significant medical and family history pertaining to medical disease including Cirrhosis of Liver, Protein Losing Enteropathy, Nephrotic Syndrome, Congenital Analbuminemia, Ulcerative Colitis, Cystic Fibrosis, Hepatitis, Heart Failure, Renal Failure, Amyloidosis and Auto-Immune Diseases ruled out.
Non GI Surgical Patients including Abdominal Trauma patients were excluded.
Patients who were lost in follow-up.
Method of Collection of Data
Details of cases were recorded including history, clinical examination, laboratory values and nutritional status given in proforma.
Independent Variables
Pre-operative serum albumin closest to the day of surgery was used in the analysis. Only those measurements that occurred within 30 days prior to the surgery were considered valid. The predictive ability of serum albumin levels were evaluated against the following: age, sex, tobacco use, alcohol use, substance abuse, weight loss, emergency operation, presence or absence of co-morbidities covering all major organ systems along with other laboratory values including serum albumin level after 48 hours, 7 days and follow-up.
Dependent Variables
Operative mortality was defined as death due to any cause occurring within 30 days of the operation. Operative morbidity were complications recorded in the 30 days after the surgeries including Length of Hospital Stay (LOS) that were grouped under early complications and follow-up late complications including re-operation. The summary measure used in this analysis was the presence or absence of one or more of the complications. For the diagnosis of these complications, certain laboratory investigations and imaging studies were done and expert opinion were taken for confirmation and management of these complications.
Follow-up of the patients and examination along with full assessment in view of late post-operative complications.
Statistical Analysis
Taking into consideration the population and other variables, statistically relevant sample size was taken using the following formula:
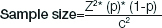
Where:
Z=Z value (e.g., 1.96 for 95% confidence level), p=percentage picking a choice, expressed as decimal (.5 used for sample size needed), c=confidence interval, expressed as decimal (e.g., .04=±4)
Statistical analysis was done by using descriptive and inferential statistics using Chi-square test. Software used in the analysis was SPSS17.0 version and Graph Pad Prism 5.0.
Continuous variables were presented as Mean±Standard Deviation (SD) and compared using t-test. Categorical variables were presented as proportions and compared using chi-square test. Multivariate analysis were used to determine risk factors associated with serum albumin and various clinical and biochemical parameters. The p-value <0.05 was regarded as being statistically significant.
Results
The study was conducted on 99 patients, aged between 19-70 years, who underwent major GI surgeries. Maximum number of patients was in the age group 40-59 years [Table/Fig-2]. Seventy three patients (73.74%) were male; the Male to Female ratio (M:F) was 2.8:1.
Age wise distribution of patients.
| Age group (years) | Frequency | Percentage |
|---|
| <20 | 1 | 1.01 |
| 20-39 | 25 | 25.25 |
| 40-59 | 43 | 43.43 |
| 60-70 | 30 | 30.30 |
| Total | 99 | 100.0 |
| Mean±SD | 48.25±15.16 y (19-70 y) |
Serum Albumin Level
Most of the patients (56.57%) had albumin in the range of 2.1-2.7 gm/dL [Table/Fig-3].
Distribution of patients according to serum albumin level.
| Pre-operative serum albumin (gm/dL) | Frequency | Percentage |
|---|
| <2.1 | 3 | 3.03% |
| 2.1-2.7 | 56 | 56.57% |
| 2.8-3 | 40 | 40.40% |
| Total | 99 | 100% |
Distribution of Subjects According to BMI
Forty nine patients had BMI less than 18.5 kg/m2 (49.49%) [Table/Fig-4].
Distribution of study subjects according to BMI.
| BMI (kg/m2) | Frequency | Percentage |
|---|
| <18.5 | 49 | (49.49%) |
| 18.5-24.9 | 45 | (45.45%) |
| >25 | 5 | (5.05%) |
| Total | 99 | (100%) |
Complication Rates and Type of Surgery
Fifty nine patients (59.60%) developed post-operative complications. Thirty one (31.31%) patients had elective surgery and 68 (68.69%) patients underwent emergency surgeries.
Relation Between Age and Complications
It was observed that out of the total patients, maximum number of complications was present in the age groups 40-70 years. There was a significant co-relation between age and complications (p=0.0001) [Table/Fig-5].
Relation between age and complications.
| Age (years) | Complications | Total |
|---|
| Present | Absent |
|---|
| <20 | 0 (0%) | 1 (1.01%) | 1 (1.01%) |
| 20-39 | 7 (7.07%) | 18 (18.18%) | 25 (25.25%) |
| 40-59 | 26 (26.26%) | 17 (17.17%) | 43 (43.43%) |
| 60-70 | 26 (26.26%) | 4 (4.04%) | 30 (30.30%) |
| Total | 59 (59.60%) | 40 (40.40%) | 99 (100%) |
| χ2-value | 20.98, p-value=0.0001 |
Relation Between Sex and Complications
It was observed that the complication in males was 42.42% and in females, it was 17.17%. It was also found that when complication rate was taken among only males, the complication rate was 57.5% and among females, the rate was 65.3% [Table/Fig-6].
Relation between sex and complications.
| Sex | Complications | Total |
|---|
| Present | Absent |
|---|
| Male | 42 (42.42%) | 31 (31.31%) | 73 (73.74%) |
| Female | 17 (17.17%) | 9 (9.09%) | 26 (26.26%) |
| Total | 59 (59.60%) | 40 (40.40%) | 99 (100%) |
| χ2-value | 0.49, p-value=0.48 |
Early Post-operative Complications
Early post-operative complications included complications, which occurred during the first 30 days post-operative. Among the total study subjects, 59 (59.6%) patients had complications and SSI was seen in 32 (32.32%) patients, which was the most common early post-operative complication in present study [Table/Fig-7].
Early post-operative complications.
| Complications | Code | Frequency | Percentage (%) |
|---|
| Systemic sepsis | SS | 2 | 2.02 |
| Acute renal failure | ARF | 3 | 3.03 |
| Myocardial infarction | MI | 4 | 4.04 |
| Pneumonia | LRTI | 17 | 17.17 |
| Urinary infection | UTI | 16 | 16.16 |
| Pulmonary oedema | PEd | 1 | 1.01 |
| Pleural effusion | PEf | 5 | 5.05 |
| Surgical site infection | SSI | 32 | 32.32 |
| Wound dehiscence | WD | 5 | 5.05 |
| Pulmonary embolism | PE | 1 | 1.01 |
| Deep vein thrombosis and thromboplebitis | DVT | 1 | 1.01 |
| Cardiac arrest | CA | 1 | 1.01 |
| Burst abdomen | BA | 2 | 2.02 |
| Biliary fistula | BF | 1 | 1.01 |
| Fecal fistula | FF | 6 | 6.06 |
| Adult respiratory distress syndrome | ARDS | 5 | 5.05 |
| Ventilatory support | VS | 7 | 7.07 |
| Intra-operative bleeding/Transfusion | BT | 12 | 12.12 |
It was also found that there was prolonged in-patient stay in the 34.34% of study patients and delayed bowel movement in 40.40% of the patients.
Late Post-operative Complications (>30 days)
Complications that were found in post-operative follow-up visits were taken into consideration. It was found that Wound Dehiscence was present in 9 (9.09%) patients and was the most common followed by LRTI in 4 (4.04%) patients and Pleural Effusion in 4 (4.04%) patients. Re-operation was done in 3 (3.03%) patients during the late post-operative period up-to 2 years post-operative. The other complications are shown in [Table/Fig-8].
Late post-operative complications.
| Late post-operative complications | Code | Frequency | Percentage (%) |
|---|
| Pneumonia | LRTI | 4 | 4.04 |
| Pleural effusion | PEf | 4 | 4.04 |
| Surgical site infection | SSI | 3 | 3.03 |
| Wound dehiscence | WD | 9 | 9.09 |
| Burst abdomen | BA | 1 | 1.01 |
| Biliary fistula | BF | 1 | 1.01 |
| Incisional hernia | IH | 2 | 2.02 |
| Para-stomal hernia | PH | 2 | 2.02 |
| Re-operation | RO | 3 | 3.03 |
Relation Between Pre-operative Serum Albumin and Early Post-operative Complications
It was observed that out of the total patients, the rate of early post-operative complication was high (59.60%) most of which was present in serum albumin level 2.1-2.7 gm/dL (43.43%), followed by 13.13% in serum albumin 2.8-3 gm/dL and 3.03% below 2.1 gm/dL.
The relation between pre-operative serum albumin and early post-operative complications was found to be statistically significant (p-value 0.0001) [Table/Fig-9].
Relation between pre-operative serum albumin and early post-operative complications.
| Pre-operative serum albumin (gm/dL) | Early post-operative complications | Total |
|---|
| Present | Absent |
|---|
| <2.1 | 3 (3.03%) | 0 (0%) | 3 (3.03%) |
| 2.1-2.7 | 43 (43.43%) | 13 (13.13%) | 56 (56.57%) |
| 2.8-3 | 13 (13.13%) | 27 (27.27%) | 40 (40.40%) |
| Total | 59 (59.60%) | 40 (40.40%) | 99 (100%) |
| χ2-value | 21.10, p=0.0001 |
Relation Between Pre-operative Serum Albumin and Late Post-operative Complications
It was observed that out of the total patients, late post-operative complication (>30 days post-op) was found in 29 patients (29.29%) most of which was present in serum albumin level 2.1-2.7 gm/dL (21.21%).
The relation between pre-operative serum albumin and late post-operative complications was found to be statistically significant (p-value 0.02) [Table/Fig-10].
Relation between pre-operative serum albumin and late pos-toperative complications.
| Pre-operative serum albumin (gm/dL) | Late post-operative complications (>30 days) | Total |
|---|
| Present | Absent |
|---|
| <2.1 | 2 (2.02%) | 1 (1.01%) | 3 (3.03%) |
| 2.1-2.7 | 21 (21.21%) | 35 (35.35%) | 56 (56.57%) |
| 2.8-3 | 6 (6.06%) | 34 (34.34%) | 40 (40.40%) |
| Total | 29 (29.29%) | 70 (70.71%) | 99 (100%) |
| χ2-value | 7.79, p=0.020, S, p<0.05 |
p-value <0.05; S: Statically significant
Relation Between Pre-operative Serum Albumin and Post-operative Mortality
Out of the total, 4 (4.04%) patients had mortality, which was most common in serum albumin level 2.1-2.7 gm/dL. The relation between pre-operative serum albumin and mortality was found to be statistically significant (p-value 0.014) [Table/Fig-11].
Relation between pre-operative serum albumin and pos-toperative mortality.
| Pre-operative serum albumin (gm/dL) | Post-operative mortality | Total |
|---|
| Present | Absent |
|---|
| <2.1 | 1 (1.01%) | 2 (2.02%) | 3 (3.03%) |
| 2.1-2.7 | 3 (3.03%) | 53 (53.54%) | 56 (56.57%) |
| 2.8-3 | 0 (0%) | 40 (40.40%) | 40 (40.40%) |
| Total | 4 (4.04%) | 95 (95.96%) | 99 (100%) |
| χ2-value | 8.57, p=0.014, S, p<0.05 |
p-value <0.05; S: Statically significant
Relation Between Body Mass Index (BMI) and Complications
Out of 99 patients, majority of the patients had BMI in the range of <18.5 kg/m2 (44.44%) in which complication was present.
Considering patients with BMI <18.5 kg/m2, the rate of complications was 89% and between 18.5-24.9 kg/m2 rate of complication was 26% and 60% between 25-30 kg/m2. Relation with BMI was found to be statistically significant (p-value 0.0001) [Table/Fig-12].
Relation between BMI and complications.
| BMI (kg/m2) | Complications | Total |
|---|
| Present | Absent |
|---|
| <18.5 | 44 (44.44%) | 5 (5.05%) | 49 (49.49%) |
| 18.5-24.9 | 12 (12.12%) | 33 (33.33%) | 45 (45.45%) |
| 25-30 | 3 (3.03%) | 2 (2.02%) | 5 (5.05%) |
| Total | 59 (59.60%) | 40 (40.40%) | 99 (100%) |
| χ2-value | 38.82, p=0.0001 |
Relation Between Type of Surgery and Complications
For emergency surgeries, the rate of complication was 61% and for Elective surgeries, it was 54%. This relationship was not found to be statistically significant (p-value 0.51) [Table/Fig-13].
Relation between type of surgery and complications.
| Type of operation | Complications | Total |
|---|
| Present | Absent |
|---|
| Elective | 17 (17.17%) | 14 (14.14%) | 31 (31.31%) |
| Emergency | 42 (42.42%) | 26 (26.26%) | 68 (68.69%) |
| Total | 59 (59.60%) | 40 (40.40%) | 99 (100%) |
| χ2-value | 0.42, p=0.51 |
Discussion
In the present study, maximum rate of complications was noted in the patients of age 60-70 years which was 86.6% followed by 60.4% in 40-59 years of age and 28% in 20-39 years of age. There was a significant co-relation between age and complications (p=0.0001). Similar results were observed by other authors too, showing a significant relation between age and complications most commonly in the age group >60 years [13,15,18].
The present study showed that patients with pre-operative serum albumin <3 gm/dL had statistically significant early and late post-operative complications. The rate of complication was 100% in patients with serum albumin <2.1 gm/dL. In the regression models, albumin level was the strongest predictor of morbidity for surgery particularly for some types of morbidity such as sepsis and major infections and also a good prognostic indicator.
In a study done by Davenport DL et al., on 183,069 patients subjected to general and vascular surgeries, it was found that a serum albumin <3.5 g/dL and weight loss >10% was associated with cardiac complication with a significant p-value (0.0001) [19]. Lohsiriwat V et al., suggested that pre-operative hypoalbuminemia (<3.5 gm/dL) is an independent risk factor for post-operative complications following rectal cancer surgery [14].
Vincent JL et al., showed that hypoalbuminemia was a potent dose dependent, independent predictor of poor outcome [20]. A serum albumin level of <2 gm/dL in critically ill patients has been shown to be associated with a mortality of nearly 100%. The association between hypoalbuminemia and poor outcome appeared to be independent of both nutritional status and inflammation. In a study of 244 surgical patients it was found that hypoalbuminemia was the significant risk factor for post-operative complications and delayed time to first bowel movement [14].
Different studies have taken different levels of serum albumin for predicting post-operative morbidity, significant relation between low serum albumin level and complications have been observed in these studies (<2.5 g/dL-, 3.5 g/dL) [14,15,21-24].
Gibbs J et al., reported that Pneumonia (10.6%) and SSI (10.3%) were the two most common complications in the patients who had hypoalbuminemia [15]. Similar results were observed by Hennessey DB et al., where a total of 105 patients developed SSI (20%) [13]. In the present study, SSI (32.32%) and Pneumonia (LRTI, 17.17%) were the most common complications in the early post-operative period. Increased incidence of pneumonia, wound infection, septicaemia post-operatively was reported by Brown RO et al., in their study in patients with serum albumin levels <3 g/dL. Albumin <3 gm/dL was associated with an increased rate of deep versus superficial SSI (p-value=0.002) [25]. The duration of inpatient stay negatively correlated with pre-operative albumin (p-value < 0.001). Similarly, a negative co-relation was found by Badia-Tahull MB et al., between albumin levels and hospital stay regardless of the type of surgery [26].
In the late post-operative period (>30 days post-op), the present study showed that wound dehiscence (9.09%) was the most common complication. Re-operation was required in 3.03% patients, which was done for burst abdomen, incisional and para-stomal hernias. It was also observed that whenever there was development of surgical complications, there was prolonged hospital stay (34.34%) which had profound impact on financial issues and hospital borne diseases. Delayed start of post-operative bowel function was present in 40.40% of the patients who developed complications. Similar results were also reported in two other studies [14,22] who both proposed that low pre-operative serum albumin concentrations were associated with longer hospital stays compared to those where concentrations were higher. Anderson CF et al., observed that low albumin had a sensitivity of 22% and a specificity of 91% in predicting hospitalisation lasting more than 10 days and a sensitivity of 10% and specificity of 86% for complications [27].
Considering BMI, it was found in the present study that low BMI status resulted in increased post-operative complications. The rate of complications was most common in patients with BMI <18.5 kg/m2 which was found to be 89%. Relation between low BMI and complications was found to be statistically significant (p-value 0.0001). Similar reports were presented by Mullen MG et al., and Beghetto DT et al., [28,29]. Engelman S et al., also found that serum albumin levels <2.5 g/dL was associated with increased risk and BMI <20 kg/m2 and > 30 kg/m2 was also associated with increased rates of post-operative complications [30]. Mullen JJ et al., found that low BMI <18.5 kg/m2 has a five fold increased risk in resulting to post-operative complications, whereas high BMI >30 kg/m2 was associated with only SSI [28]. Brooks-Brunn JA also identified several independent risk factor in the development of post-operative pulmonary complications following abdominal surgery among which were age >60 years (p=0.0006) and BMI >27 kg/m2 (p=0.0035) and ASA Class (p=0.0276) [18].
Palma S et al., published a prospective study of increased cholesterol and decreased serum albumin as a risk factor for death in patients undergoing general surgery [31]. Total cholesterol and its fraction were similar in patients with a serum albumin levels below 3.4 gm/dL and in those with a higher level. The results indicate that low levels of serum albumin, total cholesterol and HDL-C are associated with risk of death up to two years after general surgery.
The 30 day mortality had a strong association (p<0.001) with decreased serum albumin levels and a sustained increase in mortality rates as albumin values declined [15]. Lin MY et al., concluded that an albumin level below the discriminatory threshold of 3.2 g/dL was a significant predictor of overall post-operative infectious and non-infectious complications, and mortality (p<0.001) [23]. In the present study, It was found that pre-operative serum albumin was a strong indicator for post-operative mortality (4.04%, p=0.014) which was highest in patients with serum albumin <2.1 gm/dL (33%). Similarly, Beghetto MG et al., found in a univariate analysis that serum albumin <3.5 gm/dL was the strongest predictive parameter for post-operative mortality (p<0.01) [29]. However, in another study there was no mortality even though their patients had low BMI and low serum albumin levels [14]. Leite HP et al., proposed that pre-operative concentrations lower than 3.0 g/dL were also associated with increased post-surgical mortality (p-value=0.0138) [22]. Golub R et al., and Liop JM et al., also reported that upon admission albumin levels of <3 g/dL and <3.5 g/dL, respectively, causes complications and higher mortality among surgical patients [32,33].
Foley EF et al., also observed similar increase in post-operative increase in mortality in patients with serum albumin level <2.5 gm/dL (p<0.001) [21].
Truong A et al., mentioned that hypoalbuminemia significantly influences the length of hospital stay and complication rates, specifically SSI, enterocutaneous fistula, and DVT formation [34]. It has also been found that early post-operative decrease of serum albumin correlated with the extent of surgery, its metabolic response, with adverse outcomes and length of stay [35].
Limitation(s)
The present study was a single institutional study. The study was done over a short duration of time with a limited time for follow-up of operated patients. The purpose of the study was to study the patients not only in the immediate post-operative period but over a longer duration of time and this was not possible in the present study due to short span of follow-up and certain patients came from different states and were lost to follow-up.
Conclusion(s)
It is obvious in the study that wherever serum albumin and BMI were both below the normal levels, the complication rate increased. Pre-operative improvement of nutritional status must be done before undertaking any surgery. Low BMI and hypoalbuminemia are potential predictors of post-operative complications and may lead to prolonged hospital stay and additional cost burden for the patients and the hospital both. Pre-operative hypoalbuminemia <3.0 gm/dL is a strong and independent risk factor for post-operative morbidity and mortality in GI surgeries and BMI is a strong indicator for post-operative complications.
Author Contribution
Dr. BL and Dr. V- Compilation and analysis of the data along with patient data collection, Dr. DG- Thesis guide, Dr. SL- Principle investigator.