Bilateral Fibrothecoma: A Rare Case in Young Woman
Anupriya Gupta1, Shruti Pathak2
1 Junior Resident, Department of Obstetrics and Gynaecology, Sri Aurobindo Institute of Medical Sciences, Indore, Madhya Pradesh, India.
2 Junior Resident, Department of Obstetrics and Gynaecology, Sri Aurobindo Institute of Medical Sciences, Indore, Madhya Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Anupriya Gupta, 15 Yeats Court, 4 Tynemouth Road, London, England, United Kingdom.
E-mail: anupriya.0016@gmail.com
Fibrothecomas are rare sex cord stromal tumours. They usually occur in postmenopausal women and are mostly unilateral. They are usually associated with good prognosis; however, difficulties are encountered in establishing diagnosis. The treatment includes surgical resection. Here, the authors describe a rare case of a bilateral ovarian fibrothecoma in a 20-year-old female who presented with a large pelvic mass. On examination, there was a regular, immobile solid mass extending 30 weeks pregnancy size per abdomen. Pelvic examination revealed a firm nodular mass with minimal mobility and uterus could not be appreciated separately. On ultrasonography, a large solid mass arising from the pelvis superior and to the right of the uterus extending up to right hypochondrium was seen along with few cystic spaces and peripheral vascularity. Computerised tomography demonstrated two large solid cystic abdominopelvic mass lesion with internal solid enhancing areas and calcification of approximately 18 cm on the right side and 14 cm on the left side. The patient underwent exploratory laparotomy. Intra-operatively, the right ovarian mass was found, which was histopathologically confirmed as bilateral ovarian tumour (Bilateral Fibrothecoma).
Meig’s syndrome, Ovarian tumour, Sex cord, Stromal tumour
Case Report
A 20-year-old married female presented with a two and a half month history of increasing abdominal mass. There were no associated gastrointestinal symptoms or vaginal bleeding. She had a heavy but regular menstrual cycle. On examination, there was a regular, immobile solid mass extending 30 weeks pregnancy size per abdomen. There was no associated tenderness. The bowel sounds were normal to auscultation. Pelvic examination revealed a firm nodular mass with minimal mobility and uterus could not be appreciated separately.
On ultrasonography, a large solid mass arising from the pelvis superior and to the right of uterus extending up to right hypochondrium was seen along with few cystic spaces and peripheral vascularity. This was accompanied by another small mass of similar echotexture noted posterior and to the left of uterus which in results pushing the uterus upwards. Both the ovaries were not visualised separately.
Computerised tomography demonstrated two large solid cystic abdominopelvic mass lesion with internal solid enhancing areas and calcification of approximately 18 cm on right side and 14 cm on left side. Clinical diagnosis was of suspected giant myoma, but ovarian malignancy could not be excluded. Patient was counselled for possibility of hysterectomy, bilateral salpingo-oophorectomy and long term need for hormone replacement therapy.
Complete haemogram and routine blood biochemistry of the patient were within normal limits. The serum CA-125 levels were found to be 21 U/mL. Unfortunately, other tumour markers could not be tested due to unaffordability. Endometrial biopsy demonstrated endometrial hyperplasia without atypia.
The patient underwent exploratory laparotomy. Intrao-peratively, right ovarian mass of 18 cm × 17 cm × 9 cm and left ovarian mass of 14 cm × 8.5 cm × 6 cm were found. She underwent bilateral salpingo-oophorectomy as no normal ovarian tissue was visualised separately from the mass. Histopathology of bilateral ovarian tumour revealed fibrothecoma. There were no malignant changes in the tumour. Uterus and attached fallopian tubes were normal. There was no ascites. The omentum appeared normal. No evidence of peritoneal disease or enlarged para-aortic lymph nodes or pelvic lymph nodes was found. Peritoneal washings and omental biopsy were free of malignant cells. Post-operative ultrasonography of abdomen and pelvis was normal.
Gross Examination revealed Left ovarian mass (weight-440 gm) showing glistening, smooth yellowish white outer surface measuring 14 × 8.5 × 6 cm, with soft to firm consistency [Table/Fig-1]. Cut sections with homogenous yellowish white appearance were present.
Gross specimen of bilateral salpingo-oophorectomy.

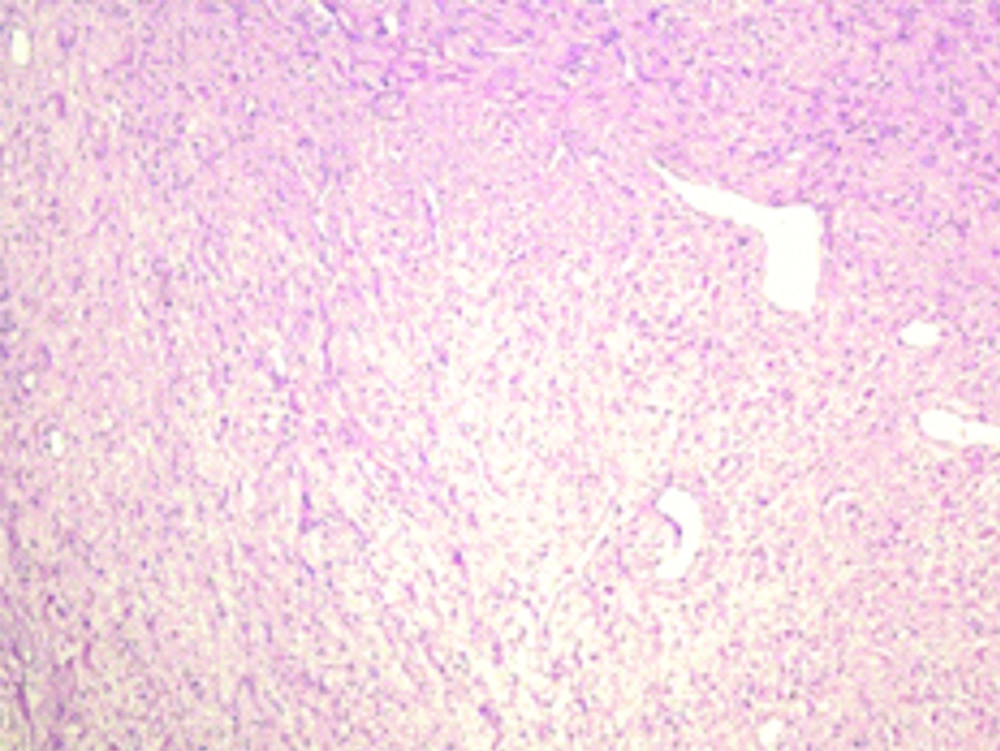
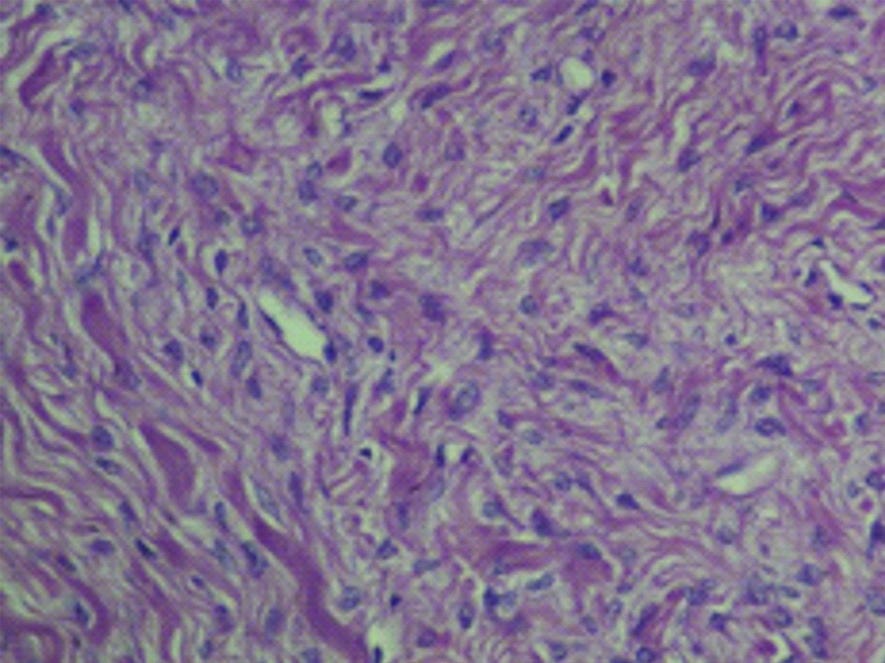
Right ovarian mass (weight-2.4 kg) measured 18 cm× 17 cm × 9 cm, with smooth glistening surface with congested vessels, yellow-white in colour and soft to firm consistency. The cut-section was homogenous, yellow white with few small cystic areas filled with yellowish mucoid fluid. Right and left fallopian tubes measure 65 mm × 5 mm, 66 mm × 5 mm and were unremarkable. Post-operative histology with Haematoxylin and Eosin stain demonstrated sections from both the ovarian masses composed of intermixed fibro collagenous tissue and loose areolar tissue with wavy fibres and clear to myxomatous background. Rim of normal ovarian stroma was present at periphery along with focal areas of necrosis and degeneration. The cellular features also showing round and spindle shaped nuclei without atypia. No mitotic figures were observed. Both tubes were noted to be normal [Table/Fig-2,3]. Tumour was classified as Stage 1B.
Microphotograph showing intermixed fibro collagenous stroma, (×100, Haematoxylin and Eosin stain).
Microphotograph showing cellular features having round and spindle shaped nuclei without atypia (X400, Haematoxylin and Eosin stain).
Post-operatively, patient was disease free on 1 year follow-up and has been advised further close follow-up.
Discussion
Fibrothecoms are rare ovarian tumours which sometimes occur in extra ovarian tissue assumed to arise in ectopic ovarian tissue. Although histologically both are indistinguishable [1,2]. They constitute 1.0-4.0% of all ovarian tumours [3]. They are primarily benign tumours arising almost always from ovarian medulla. They are solid in consistency and have mixed constituents of both fibroma and the coma [4]. Chen H et al., described occurrence of Fibrothecoms after menopause in 63.93% of the lesions, of which 65.57% in women aged 51 to 70 years. Most common presentation was palpable pelvic masses, whereas 64% of these patients were asymptomatic. Microscopically, appearance is of spindle cell proliferation [5]. Magnetic Resonance Imaging (MRI) is the imaging modality of choice in determining the adnexal mass which is indistinguishable on palpation and sonography [6]. The aetiology of development of fibrothecomais not clearly understood. They mostly present as a growing mass pressing on other organs but can present with endocrine effects mostly due to oestrogen like endometrial hyperplasia coming from the coma component but occasionally causes androgenic stimulation [1,2,7]. An 8% of the tumours may undergo torsion [7]. Ovarian fibrothecomas have been incidentally linked with Meigs’ syndrome, typically described as the triad of ascites, unilateral hydrothorax, and benign ovarian tumour imitating ovarian cancer. Symptoms resolve with the removal of the ovarian mass [8]. In our case, the patient had no such signs. Serum CA-125 levels are in normal range in fibrothecomas [2]. Albeit sonography has been scrutinised as the imaging modality for handpicking of ovarian masses, the sonographic features of ovarian fibrothecoma are inconclusive.
Mak CW et al., reported that these tumours may appear as a homogeneous hypoechoic mass with posterior acoustic shadowing, although majority of the cases sonographic appearance is nonspecific. On CT scans, these tumours have delayed accrue of contrast medium. Although intratumoural haemorrhage, infarction, myxoid or cystic degeneration, calcification may impinge the appearance of the fibrothecoma [9]. On MRI signal characteristics are homogeneous low signal intensity on T1 and T2 and scattered high signal areas from degeneration on T2 [10]. Leiomyomas and solid ovarian masses such as Brenner tumours, Granulosa cell tumours and Dysgerminomas are the other differential diagnosis for fibrothecoma [10,11]. However, the preferred treatment for sex cord-stromal tumours is surgical resection and is associated with a good prognosis [12]. The main purpose of this study was to discuss this rare syndrome, undertake a literature search and highlight challenges in diagnosis of ovarian fibroma.
Conclusion(s)
Fibrothecomas are rarely aggressive, precise diagnosis can avert invasive measures and less invasive techniques like laparoscopic surgery could be considered as possible alternatives.
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 05, 2020
Manual Googling: Mar 25, 2020
iThenticate Software: Apr 11, 2020 (13%)
[1]. Chen VW, Ruiz B, Killeen JL, Timothy RC, Wu XC, Catherine NC, Pathology and classification of ovarian tumoursCancer 2003 97:2631-42.10.1002/cncr.1134512733128 [Google Scholar] [CrossRef] [PubMed]
[2]. Numanoglu C, Kuru O, Sakinci M, Akbayir O, Ulker V, Ovarian fibroma/fibrothecoma: Retrospective cohort study shows limited value of risk of malignancy index scoreAust N Z J Obstet Gynaecol 2013 53(3):287-92.10.1111/ajo.1209023611791 [Google Scholar] [CrossRef] [PubMed]
[3]. Zhang Z, Wu Y, Gao J, CT diagnosis in the thecoma-fibroma group of the ovarian stromal tumoursCell Biochem Biophys 2015 71:93710.1007/s12013-014-0288-725315640 [Google Scholar] [CrossRef] [PubMed]
[4]. Nocito AL, Sarancone S, Bacchi C, Tellez T, Ovarian thecoma: Clinicopathological analysis of 50 casesAnn Diagn Pathol 2008 12:12-16.10.1016/j.anndiagpath.2007.01.01118164409 [Google Scholar] [CrossRef] [PubMed]
[5]. Chen H, Liu Y, Shen LF, Jiang MJ, Yang ZF, Fang GP, Ovarian thecoma-fibroma groups: clinical and sonographic features with pathological comparisonJ Ovarian Res 2016 9:8110.1186/s13048-016-0291-227876070 [Google Scholar] [CrossRef] [PubMed]
[6]. Shinagare AB, Meylaerts LJ, Laury AR, Mortele KJ, MRI features of ovarian fibroma and fibrothecoma with histopathologic correlationAm J Roentgenol 2012 198:W296-303.10.2214/AJR.11.722122358029 [Google Scholar] [CrossRef] [PubMed]
[7]. Angeles RM, Salem FL, Sirota RL, A right ovarian mass in a 71-year-old woman with ascites and elevated CA 125 level. Fibrothecoma of the right ovaryArch Pathol Lab Med 2005 129(5):701-02. [Google Scholar]
[8]. Abad A, Cazorla E, Ruiz F, Aznar I, Asins E, Llixiona J, Meigs’ syndrome with elevated CA125: case report and review of the literatureEuropean Journal of Obstetrics Gynecology and Reproductive Biology 1999 82(1):97-99.10.1016/S0301-2115(98)00174-2 [Google Scholar] [CrossRef]
[9]. Mak CW, Tzeng WS, Chen CY, Computed tomography appearance of ovarian fibrothecomas with and without torsionActa Radiologica 2009 50(5):570-75.10.1080/0284185090289616319455450 [Google Scholar] [CrossRef] [PubMed]
[10]. Troiano RN, Lazzarini KM, Scoutt LM, Lange RC, Flynn SD, McCarthy S, Fibroma and fibrothecoma of the ovary: MR imaging findingsRadiology 1997 204(3):795-98.10.1148/radiology.204.3.92802629280262 [Google Scholar] [CrossRef] [PubMed]
[11]. Imaoka I, Wada A, Kaji Y, Hayashi T, Hayashi M, Matsuo M, Developing an MR imaging strategy for diagnosis of ovarian massesRadiographics 2006 26:1431-48.10.1148/rg.26504520616973774 [Google Scholar] [CrossRef] [PubMed]
[12]. Jung SE, Rha SE, Lee JM, Park SY, Oh SN, Cho KS, CT and MRI findings of sex cord-stromal tumour of the ovaryAJR 2005 185:207-15.10.2214/ajr.185.1.0185020715972425 [Google Scholar] [CrossRef] [PubMed]