A Rare Co-existence of Pulmonary Nocardiosis with E.coli Infection in Immunocompetent Host
Amithash Marulaiah Prabhudev1, Thomas Antony2, Vyshak Uddur Surendra3, Rahul Magazine4, Febi Ann Roy5
1 Assistant Professor, Department of Respiratory Medicine, Kasturba Medical College, Manipal Academy of Higher Eduation, Manipal, Karnataka, India.
2 Postgraduate Student, Department of Respiratory Medicine, Kasturba Medical College, Manipal Academy of Higher Eduation, Manipal, Karnataka, India.
3 Assistant Professor, Department of Respiratory Medicine, Kasturba Medical College, Manipal Academy of Higher Eduation, Manipal, Karnataka, India.
4 Professor and Head, Department of Respiratory Medicine, Kasturba Medical College, Manipal Academy of Higher Eduation, Manipal, Karnataka, India.
5 Postgraduate Student, Department of Respiratory Medicine, Kasturba Medical College, Manipal Academy of Higher Eduation, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vyshak Uddur Surendra, Assistant Professor, Department of Respiratory Medicine, Kasturba Medical College, Manipal-576104, Karnataka, India.
E-mail: vyshusurendra1303@gmail.com
Community Acquired Pneumonia (CAP) is the second leading cause of death worldwide. Diagnosis becomes difficult when these are associated with legionella or nocardiosis, as these are not easily grown in routine aerobic culture. In a setting of high burden countries for tuberculosis like India, an acid fast bacilli is always taken as Mycobacterium tuberculosis until and unless proved otherwise. This is a case report of 38-year-old female, with no co-morbid illness, with cough, breathlessness, and fever of two weeks duration. On sputum microbiological evaluation was found to have co-existence of Pulmonary Nocardiosis with Escherichia coli (E.coli) infection. This case is important in many levels; to begin with, considering the diagnosis, a sputum positive for acid fast staining confirms the diagnosis of pulmonary tuberculosis. Hence, diagnosis of other rare acid fast bacilli such as Nocardia may be missed. Secondly, aerobic bacteria causing mixed bacterial pneumonia are reported very rarely, and have a high mortality rate. Co-existence of Nocardia with E.coli causing pneumonia is rare. Its occurrence in an immunocompetent host makes it even more difficult for diagnosis. Patient not responding to antibiotic therapy or anti-tubercular therapy, necessitates further evaluation to rule out other co-existing potential pathogen or condition. Patient was started with cefoperazone sulbactum and amikacin along with suplhamethoxazole + trimethoprim for seven days. Suplhamethoxazole + trimethoprim, was continued for six months and she showed clinico-radiological improvement.
Community acquired pneumonia, Filamentous bacteria, Rare acid fast bacilli
Case Report
A 38-year-old female, homemaker, with no co-morbid illness, presented with the history of cough, breathlessness, and fever of two weeks duration, with weight loss and loss of appetite to the Respiratory Medicine Out-Patient Department (OPD). Patient had history of intermittent cough for 20 years. Her family history and marital history were insignificant.
Patient was evaluated and treated elsewhere, where an HRCT thorax was done, which revealed multiple patchy areas of consolidation, with features suggestive of bilateral bronchiectasis. She was referred to the tertiary centre, as there was no clinical improvement in patient condition with a course of amoxicillin clavulanic acid for seven days.
On general physical examination at the time of admission, she was moderately built and nourished, afebrile, with pulse rate of 108 beats per min, and Blood pressure of 118/78 mmHg. There was no significant lymphadenopathy. Respiratory system examination revealed bilateral coarse crackles on auscultation. Rest of the system examination was unremarkable.
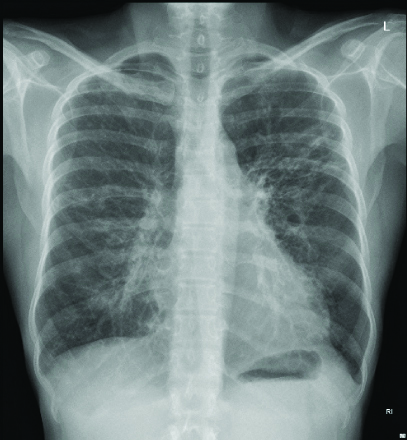
Laboratory investigation showed Haemoglobin of 11 g/dL, Total Leukocyte Count of 21000 cell/micro litre with Neutrophilia (93.4%). Chest Roentgenograph showed bilateral non-homogenous opacities with consolidation [Table/Fig-1]. Serum procalcitonin was elevated (3.040). Blood sugars were within normal limits and serological test for Human immunodeficiency virus was non-reactive. Paired blood culture was reported as sterile after five days of incubation. Sputum acid fast bacilli staining was negative for Mycobacterium tuberculosis and aerobic culture of sputum showed growth of E.coli. However, in view of bilateral non-homogenous opacities, atypical infection was suspected and modified acid fast staining and actinomyces on sputum requested. Modified acid fast staining was suspicious of Nocardia species. Repeat aerobic culture of sputum confirmed the presence of Nocardia species.
Patient was started on Cefoperazone sulbactum and Amikacin along with Sulphamethoxazole + Trimethoprim as per sensitivity pattern for a total duration of seven days. She showed clinical improvement and repeat chest Roentgenography showed improvement [Table/Fig-2]. Hence patient was discharged with oral therapy. She was continued on Sulphamethoxazole+Trimethoprim for a period of six months.
Bilateral non-homogenous patchy opacity in all zones except in left lower zone, associated with left lung cystic shadow.

Improvement in the consolidation was noted.

Bronchoscopy was done after a period of six months as patient was not able to produce sputum. Bronchial washing aerobic culture did not reveal any growth of Nocardia or Mycobacterium tuberculosis. Patient showed clinical and radiological improvement [Table/Fig-3] and is under regular follow-up.
Clearing of bilateral non-homogenous patchy opacity noted with left lung cystic shadows and fibrotic strands.
Discussion
The Community Acquired Pneumonia (CAP) is the second leading cause of death worldwide [1]. Nocardia species are infrequently encountered in clinical practice but these are challenging to clinicians. Nocardia can infect both normal and immunocompromised patients; however more commonly infects immunocompromised patients and those patients having chronic respiratory diseases [2]. They are aerobic, branching, gram-positive, filamentous bacteria, commonly isolated from soil. More commonly involved species in human infections are N. asteroides, N. brasiliensis, N. farcinica and N. nova [3].
Nocardia acts by neutralising the microbicidal activity of the host. The increased virulence of N. asteroides is attributed to its ability to inhibit phagosome-lysosome fusion and thus modifying phagocyte function [4]. In recent years, the number of cases diagnosed with Nocardial infection has been increasing, and this can be attributed to the improvements in diagnostic capabilities and the higher clinical index of suspicion accompanying the increased prevalence of immunosuppressed patients [2]. Screening for nocardiosis can be done by modified Kinyoun staining in all patients who are not responding to usual antibiotic therapy [5]. The Kinyoun method substitutes 1% sulfuric acid for acid alcohol as a decoloriser, which will allow the less tenaciously acid-fast Nocardia to retain fuchsin. Presence of Nocardia can be confirmed by sputum bacterial aerobic culture.
Mixed aerobic bacterial infections are rare. Mixed bacterial infections increase the mortality. Mortality is even higher if one of the organisms is from Ligeonella, Mycobacterium and Nocardia species. These species are not routinely grown in culture and the diagnosis may be missed which may delay in effective treatment [6]. Mixed bacterial infections require higher antibiotics for longer durations. Mixed infection with Nocardia species requires longer duration (6-12 months) of treatment with sensitive antibiotics.
Prior infection with an organism may increase susceptibility to another. Co-existence of Nocardia with E.coli causing pneumonia is rare [7]. Studies have shown that prior infection with E.coli causes increased susceptibility to Nocardia asteroides. It may be due to endothelial damage caused by bacterial endotoxin [8].
In the patient, with the above clinical scenario, Pulmonary Tuberculosis was initially suspected. However, acid fast bacilli staining was negative for Mycobacterium tuberculosis. As the patient was not showing any clinico-radiological improvement and with underlying bronchiectasis, modified acid fast staining was asked for, which was suggestive of Nocardia species. The same was confirmed by sputum aerobic culture. Though the patient was not immunocompromised, the co-existent infection with E.coli and the underlying chronic respiratory disease may have made her more susceptible to Nocardia infection.
Conclusion(s)
This case highlights the need for a broad minded approach to look for mixed aerobic bacterial infections in patients with underlying chronic respiratory condition or in those who are not responding to the conventional treatment modalities. Early diagnosis and management of respiratory bacterial infections can prevent complicated superadded infections, in this case which was Nocardia, thus reducing the morbidity, mortality, and curtailed in-patient hospital stay. Finally, in a country like India, with high burden of tuberculosis, and where even an empirical treatment with anti-tubercular treatment is justified in case of clinical suspicion, it is imperative that the other causes of acid fastness beyond the limit of tuberculosis should also be considered particularly when the patient is not responding to the usual anti-tuberculosis regimen. This not only reduces the potential adverse events following the therapy, but also the development of dreaded drug resistant tuberculosis.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jan 16, 2020
Manual Googling: Mar 13, 2020
iThenticate Software: Apr 09, 2020 (4%)
[1]. Prina E, Ranzani OT, Torres A, Community-acquired pneumoniaThe Lancet 2015 386(9998):1097-108.10.1016/S0140-6736(15)60733-4 [Google Scholar] [CrossRef]
[2]. Corti ME, Fioti ME, Nocardiosis: A reviewInternational Journal of Infectious Diseases 2003 7(4):243-50.10.1016/S1201-9712(03)90102-0 [Google Scholar] [CrossRef]
[3]. Chedid MB, Chedid MF, Porto NS, Severo CB, Severo LC, Nocardial infections: Report of 22 casesRevista do Instituto de Medicina Tropical de Sao Paulo 2007 49(4):239-46.10.1590/S0036-4665200700040000917823754 [Google Scholar] [CrossRef] [PubMed]
[4]. Beaman BL, Beaman L, Nocardia species: Host-parasite relationshipsClinical Microbiology Reviews 1994 7(2):213-64.10.1128/CMR.7.2.2138055469 [Google Scholar] [CrossRef] [PubMed]
[5]. Wadhwa T, Baveja U, Kumar N, Govil D, Sengupta S, Clinical manifestations of nocardiosis: Study of risk factors and outcomes in a tertiary care hospitalJournal of Laboratory Physicians 2017 9(4):28810.4103/JLP.JLP_111_1628966493 [Google Scholar] [CrossRef] [PubMed]
[6]. Brown RB, Sands M, Ryczak M, Community-acquired pneumonia caused by mixed aerobic bacteriaChest 1986 90(6):810-14.10.1378/chest.90.6.8103096644 [Google Scholar] [CrossRef] [PubMed]
[7]. Yang M, Xu M, Wei W, Gao H, Zhang X, Zhao H, Clinical findings of 40 patients with nocardiosis: A retrospective analysis in a tertiary hospitalExperimental and Therapeutic Medicine 2014 8(1):25-30.10.3892/etm.2014.171524944592 [Google Scholar] [CrossRef] [PubMed]
[8]. Kobayashi H, Effect of Escherichia coli and its endotoxin on the intravenous infection of mice with Nocardia asteroidesJapanese Journal of Microbiology 1970 14(6):479-86. [Google Scholar]