Cytological Diagnosis of Pilomatricoma: A Case Report
Mary Raju1, Kumari Ajitha2, Elizabeth Joseph3, Sany Philip4, Dahlia Joseph5
1 Assistant Professor, Department of Pathology, Believers Church Medical College Hospital, Thiruvalla, Kerala, India.
2 Professor, Department of Pathology, Believers Church Medical College Hospital, Thiruvalla, Kerala, India.
3 Professor, Department of Pathology, Believers Church Medical College Hospital, Thiruvalla, Kerala, India.
4 Tutor, Department of Pathology, Believers Church Medical College Hospital, Thiruvalla, Kerala, India.
5 Assistant Professor, Department of Pathology, Believers Church Medical College Hospital, Thiruvalla, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mary Raju, Department of Pathology, Believers Church Medical College, Thiruvalla-689103, Kerala, India.
E-mail: drmaryraju4@gmail.com
Pilomatricoma is an uncommon benign neoplasm arising from the cells of the outer sheath of the hair follicle. Pilomatricoma is often misdiagnosed clinically and cytologically due to rarity of the lesion as well as difficulty in obtaining all cytological features. The case reported the cytological and histopathological findings of pilomatricoma as post auricular swelling. The present case highlight the importance of considering pilomatricoma as differential diagnosis of dermal or subcutaneous nodules and to keep in mind the variability of the cellular composition of this lesion to avoid misdiagnosis.
Benign tumour, Calcifying epithelioma, Subcutaneous nodule
Case Report
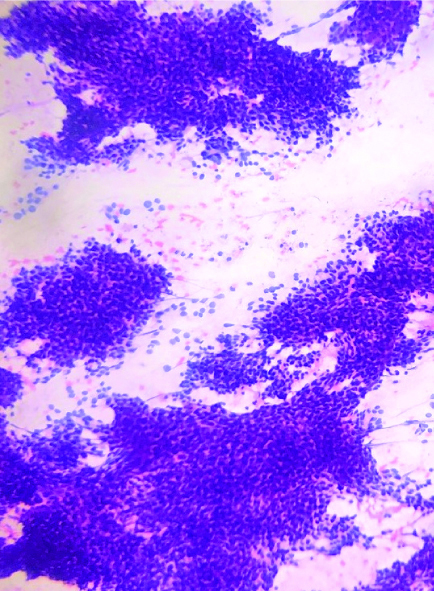
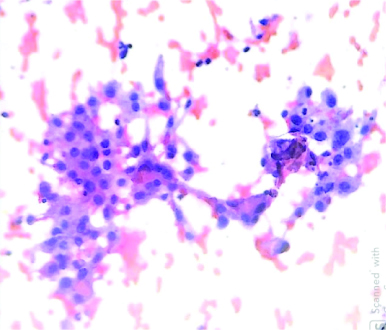
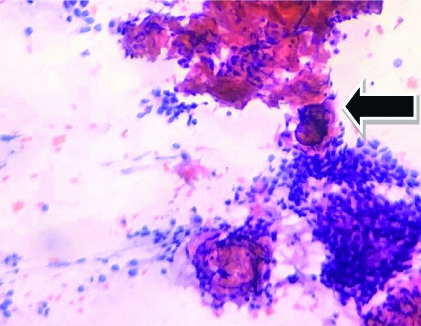
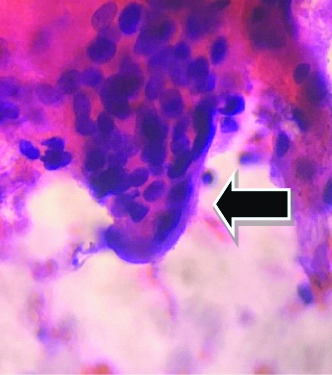
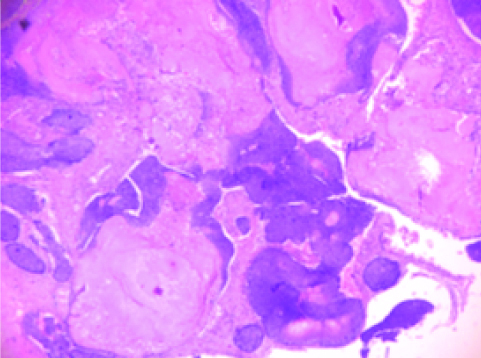
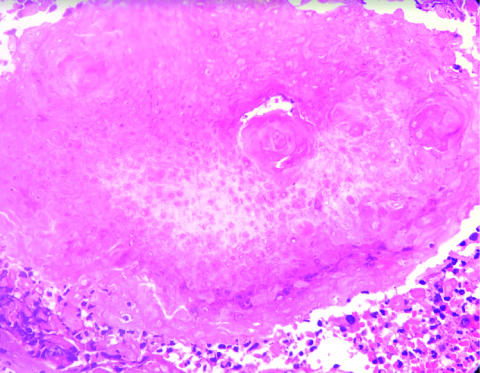
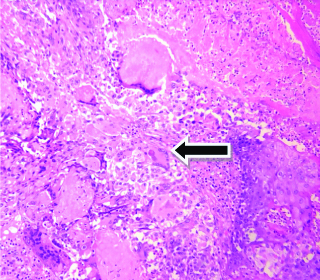
A 49-year-old healthy woman presented with a one month history of slow growing swelling on the right post auricular region. There was no history of trauma, pain, fever, chills, weight loss, fatigue, numbness; tingling sensation over the swelling. There was no significant past medical history. Physical examination revealed a 1×1 cm; non-tender, mobile soft swelling over the post auricular region. The systemic examination of the patient was found normal. Her routine blood investigations were within normal limits. The provisional diagnosis was lymphadenopathy. Fine Needle Aspiration Cytology (FNAC) was done and cytological examination showed cellular smears with two types of epithelial cells: basaloid cells with scant cytoplasm [Table/Fig-1] and polygonal cells with abundant cytoplasm [Table/Fig-2]. The background showed calcified material [Table/Fig-3] and few multinucleate giant cells [Table/Fig-4]. A cytological diagnosis of cutaneous adnexal lesion possibly pilomatricoma was rendered and excision of the lesion was advised. After two weeks, the patient underwent complete excision of the swelling under local anaesthesia and specimen was sent to pathology department for histopathological examination. The specimen was a round firm mass measuring 2×1.5×1 cm. Cut surface showed a well circumscribed nodule with pale white to grey brown areas. The histopathological examination revealed a well circumscribed lesion composed of basaloid cells [Table/Fig-5,6] and shadow cells [Table/Fig-6] with areas of calcification and foreign body giant cells [Table/Fig-7]. The diagnosis of pilomatricoma was confirmed on histopathological examination. The follow-up during six months was uneventful with no recurrence.
Cytology smear showing basaloid cells arranged in sheets (40x) PAP stain.
Cytology smear showing polygonal cells with oval nuclei and abundant cytoplasm (100x) PAP stain.
Cytology smears showing calcified material (bold arrow) and clusters of basaloid cell (100x) PAP stain.
Cytology smears showing multinucleate giant cell (bold arrow) (400x) PAP stain.
Histopathology showing basaloid cells and eosinophilic shadow cells (40x) H&E stain.
Histopathology showing eosinophilic shadow cells (400x) H&E stain.
Histopathology showing foreign body giant cell reaction (400x) H&E stain.
Discussion
Pilomatricoma is a benign tumour of hair matrix differentiation and represents 0.12% of all skin tumours [1,2]. Pilomatricoma was first described by Malherbe and Chenantais in 1880 and coined the term calcifying epithelioma of Malherbe [3]. Although they described it as a benign tumour arising from sebaceous glands, there has been a gradual increase in the understanding of morphological features of this lesion since then. Later in 1961, Forbis and Helwig proved its origin from hair matrix cells [4]. Dubreuilh and Cazenave described its unique histopathologic characteristics-the basaloid cells and shadow cells [5]. However, literature survey shows that preoperative diagnosis of pilomatricoma is a difficult one and is often misdiagnosed clinically and cytologically [Table/Fig-8] [1,5-10].
Published cases of pilomatricoma misdiagnosed clinically and cytologically [1,5-10].
| Year | Author reference | Age and sex | Location | Clinical diagnosis | Cytological diagnosis |
|---|
| 2012 | Ieni A et al., [1] | 28/M | Left foot swelling | Dermoid cyst | Round cell tumour |
| 2010 | Pant I et al., [5] | 10/F | Right upper back | Epidermal cyst | Dermoid cyst |
| 9/F | Ear lobe mass | Dermoid cyst | Dermoid cyst |
| 2011 | Bansal C et al., [6] | 35/F | Submental swelling | Calcified lymph node | Epidermal cyst |
| 22/F | Lumbar swelling | Sebaceous cyst | Epidermal cyst |
| 26/M | Neck | Lipoma | Epidermal cyst |
| 61/M | Eye brow | Epidermal cyst | Epidermal cyst |
| 2010 | Agrawal L et al., [7] | 16/M | Cervical region swelling | Lymphadenopathy | Round cell tumour |
| 2018 | Bax D et al., [8] | 21/F | Scalp swelling | Cutaneous carcinoma | Cutaneous carcinoma |
| 2020 | Shelgaonker G, et al., [9] | 65/M | Right inguinal region | Cutaneous metastasis | Metastatic carcinoma |
| 2012 | Gupta V et al., [10] | 9/F | Neck swelling | Lymphadenopathy | Squamous cell carcinoma |
The most common sites involved by this tumour are the head and neck region. This tumour usually occurs in first two decades of life with a female predisposition [1]. Pilomatricoma can be associated with myotonic dystrophy, Gardner syndrome, Steinert’s disease, Turner syndrome and Sarcoidosis [3]. The tumour most commonly presents as a firm subcutaneous mass clinically. However, the preoperative clinical diagnosis rate of pilomatricoma is very low because of the wide range of other tumours which can have the same clinical presentation such as dermoid cyst, inflammatory lesion, lipoma, fibroxanthoma, osteoma and haematoma [5]. Salivary gland tumours may be considered if the lesions are located in the region of the salivary gland as in present case.
Cytological examination of pilomatricoma reveals basaloid cells, polygonal squamous cells, shadow cells, foreign-body giant cells and calcification. All these features are rare to be found in a single case, and therefore an accurate diagnosis of pilomatricoma is difficult cytoloically [5]. The cytological differential diagnosis depends upon the predominant cell that is obtained during aspiration.
When aspirates contain predominantly squamous cells, it often leads to a misdiagnosis of epidermal inclusion cyst [6]. If the aspirate shows predominantly basaloid cells, it leads to a misdiagnosis of basal cell carcinoma. The absence of peripheral palisading in cell clusters and nucleoli favours pilomatricoma [1]. Smears that show mainly basaloid cells can be easily misinterpreted as small round cell tumour because of their high nucleus: cytoplasmic ratio and slight nuclear hyperchromasia [7]. Extreme calcification in pilomatrixoma may yield only calcified material and proper diagnosis may not be possible [5]. Metastatic squamos cell carcinoma can come as the differential if the aspirate shows predominantly polygonal cells [8]. The absence of malignant features such as nuclear pleomorphism, coarse clumping of chromatin and atypical mitosis and a proper history will allow us to exclude this [9,10].
Imaging modalities is of little value in making an accurate diagnosis of pilomatricoma [5]. The accurate diagnosis is usually rendered by histopathological examination which reveals two types of epithelial cells-basaloid cells and eosinophilic shadow cells arranged in lobules. The tumour in the early stages shows a predominance of basaloid cells. As the tumour matures, the basaloid cells acquire more cytoplasm and lose their nuclei and become the so called shadow cells. The shadow cells usually undergoes calcification over a period of time imparting a bony hard consistency to the lesion [4,5]. Histopatholoically, pilomatricoma should be differentiated from basal-cell carcinoma with matrical differentiation, and matrical carcinoma. The presence of atypical features, such as large areas of tumour necrosis, infiltrative growth, lymphovascular or perineural invasion, or large tumour size, should raise the possibility of pilomatrical carcinoma [11]. Basal cell carcinoma with matrical differentiation also show population of shadow cells with basaloid cells in the periphery similar to pilomatricoma. But the presence of peripheral palisading with stromal retraction artefact favours a diagnosis of basal cell carcinoma [12].
The treatment for pilomatricoma is complete surgical resection with clear margins [13]. Incomplete resection of the lesion can cause recurrence, described in up to 3% of cases [3]. Malignant transformation is uncommon and should be suspected in cases with repeated local recurrences [14].
Conclusion(s)
Pilomatricoma is a benign tumour of the skin arising from the hair follicle. Although the lesion is rare, it should be kept in the differential diagnosis of subcutaneous swelling especially in the head and neck region both by the clinician and the cytologist.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 16, 2019
Manual Googling: Mar 31, 2020
iThenticate Software: Apr 09, 2020 (17%)
[1]. Ieni A, Todaro P, Bonanno A, Catalano F, Catalano A, Tuccari Limits of fine needle aspiration in the diagnosing pilomatrixoma. A series of 25 cases with clinico pathologic correlationIndian J Dermatol 2012 57:152-55.10.4103/0019-5154.9429522615520 [Google Scholar] [CrossRef] [PubMed]
[2]. Garg LN, Arora S, Gupta S, Singh P, Pilomatricoma: Forget me notIndian Dermatol Online J 2011 2(2):75-77.10.4103/2229-5178.8599523130229 [Google Scholar] [CrossRef] [PubMed]
[3]. Amin J, Farooq S, Wani AL, Bilal S, Imtiyaz H, Pilomatrixoma: A clinico-pathological studyInt J Curr Res 2019 6(2):B01-03.10.21276/ijcmr.2019.6.2.5 [Google Scholar] [CrossRef]
[4]. Borse H, Sorate Y, Chandak S, Pilomatrixoma of the thigh-A case reportMVP Journal of Medical Sciences 2018 5(1):121-24.10.18311/mvpjms/2018/v5i1/735 [Google Scholar] [CrossRef]
[5]. Pant I, Josi SC, Kaur G, Pilomatricoma as a dignostic pitfall in clinical practice. Report of cases and review of literatureIndian J Deramatol 2010 55:390-92.10.4103/0019-5154.7456621430899 [Google Scholar] [CrossRef] [PubMed]
[6]. Bansal C, Handa U, Mohan H, Fine needle aspiration cytology of pilomatricomJ Cytol 2011 28(1):01-06.10.4103/0970-9371.7694021552399 [Google Scholar] [CrossRef] [PubMed]
[7]. Agrawal L, Kaur P, Singh J, Singh N, Pilomatrixoma misdiagnosed as round cell tumour on fine-needle aspiration cytologyInd J Cancer 2010 47:483-85.10.4103/0019-509X.7356521131775 [Google Scholar] [CrossRef] [PubMed]
[8]. Bax D, Bax M, Pokharel S, Bogner PN, Pilomatricoma of the scalp mimicking poorly differentiated cutaneous carcinoma on positron emission tomography/computed tomography (PET/CT) scan and fine-needle aspiration (FNA) cytologyJAAD Case Reports 2018 4:446-48.10.1016/j.jdcr.2017.12.00629984278 [Google Scholar] [CrossRef] [PubMed]
[9]. Shelgaonkar G, Arya A, Bansal B, Kumar D, Das P, Pilomatricoma simulating metastatic pancreatic carcinoma: A diagnostic pitfallJ Cytol 2020 37:62-63.10.4103/JOC.JOC_104_1931942101 [Google Scholar] [CrossRef] [PubMed]
[10]. Gupta V, Marwah N, Jain P, Diagnostic pitfalls of pilomatricoma on fine needle aspiration cytologyIranian J Dermat 2012 15:59-61. [Google Scholar]
[11]. Kraft S, Granter RS, Molecular pathology of skin neoplasms of the head and neckArch Pathol Lab Med 2014 138:759-87.10.5858/arpa.2013-0157-RA24878016 [Google Scholar] [CrossRef] [PubMed]
[12]. Kyrpychova L, Carr RA, Martinek P, Vanecek T, Perret R, Chottová-Dvořáková M, Basal cell carcinoma with matrical differentiation: Clinicopathologic, immunohistochemical, and molecular biological study of 22 casesAm J Surg Pathol 2017 41(6):738-49.10.1097/PAS.000000000000084128368926 [Google Scholar] [CrossRef] [PubMed]
[13]. Kwon D, Grekov K, Krishnan M, Dyleski R, Characteristics of pilomatrixoma in children: A review of 137 patientsInt J Pediatr Otorhinolaryngol 2014 78(8):1337-41.10.1016/j.ijporl.2014.05.02324954158 [Google Scholar] [CrossRef] [PubMed]
[14]. Phukan JP, Sinha A, Biswas S, Cytodiagnosis of pilomatrixoma from an uncommon site with unusual presentationInt J Trichology 2012 4(4):280-82.10.4103/0974-7753.11120523766616 [Google Scholar] [CrossRef] [PubMed]