The word meaning of Pseudomyopia is false shortsighthedness. The other words that are also synonymus to pseudomyopia are accommodative spasm or accommodative excess and spurious myopia.
The only way of finding this is a properly done ocular examination. Over-correction can produce asthenopia i.e., eyestrain, pain in and around the eyes, headaches, migraines. Cycloplegics such as homatropine, cyclopentolate and tropicamide are used to detect pseudomyopia. However, pseudomyopia can also be detected without the use of cycloplegic drugs, by methods such as fogging done by high powered convex lenses. Hypermetropia is defined as a type of refractive error in which parallel rays of light coming from infinity is focused in front of retina, with accommodation at rest [1]. The amount of hypermetropia is measured in terms of the diopteric power of the convex lens which is required to be placed at the vertex distance to shift the focused rays towards the retinal plane, the diopteric value is reported in terms of convex sphere or a sphero-cylinder as in cases of a co-existing astigmatism.
Clinically, hyperopia may be divided into three categories, namely the simple hyperopia, pathological hyperopia and functional hypermetropia. The commonest among them being simple hyperopia which may be further classified as axial hypermetropia, curvatural hypermetropia and index hypermetropia. Functional hypermetropia is due to paralysis of accommodation, as seen with cycloplegic drugs or due to third nerve palsy. Pathological hyperopia is a condition seen in cases of abnormal ocular developments such as microphthalmos, nanophthalmos and trauma [2].
Depending on the magnitude of hyperopia the disease is classified as mild, moderate and severe hypermetropia. Mild hypermetropia ranges in a convex spherical power of less than +2.00 diopters. Moderate hypermetropia ranges from +2.25 to +5 diopters of convex spherical refractive error. High hypermetropia is anything more than +5.00 diopters of convex spherical refractive error. This hyperopia classification scheme relates to the role of accommodation [3].
Accomodation reflex is known to transiently relieve manifest hypermetropia and to some extent even facultative hypermetropia. However, prolonged hours of near work can exhaust this accommodation range and magnitude leads to development of symptoms like vision blur, asthenopia, brow ache, strabismus and loss of binocular single vision. This phenomenon is more likely to develop in moderate to higher degree of hypermetropes and in adult population who have a higher visual need.
In a study, it was shown that accommodation affects hyperopia more than myopia. The findings in the study suggested that cycloplegia brought about a greater shift in the diopters of spherical equivalent in hypermetropes compared to myopes and astigmatics. This also suggests that cycloplegia is an essential step in evaluation of all refractive errors [4].
Pseudomyopia is due to spasm of accommodation. In this condition there is a temporary shift towards myopia. The accommodation reflex causes a contraction of the ciliary body leading to its forward and inward movement. This movement relaxes the zonular fibres attached to the equator of the lens, leading to a spherical shape of the lens, making it a more powerful convex lens and hence capable of focusing near objects more easily [5,6]. Hence, during a state of spasm of accommodation there is a shift towards myopia.
The cause may be organic or functional due to eye strain. Functional is seen in young adults who have active accommodation, and occurs after a change in visual demands, such as students preparing for an exam, or a change in occupation. The diagnosis mandates a cycloplegic refraction always.
Organic causes of pseudomyopia include head trauma, encephalitis, intracranial masses, and cerebrovascular diseases. These cerebral conditions are more likely to affect the supranuclear controls of the third nerve nucleus and the Edinger Westphal nucleus [7]. Since, there are not many treatment modalities for these neurologic conditions, the treatment lies in managing the spasm of the ciliary muscle [8].
Treatment is dependent on the underlying aetiology. Organic causes include systemic or ocular medications. Functional pseudomyopia can be corrected by altering the working distance for the induced hyperopia. The change in existing refractive correction can be tried for managing the disease condition, such as reducing the power of the concave lens if there is pre-existing myopia. Ocular exercises can be also be tried using convergence exercises and prisms [9].
This study was conducted to understand the shift in the refractive errors documented in patients who presented with low diopters of myopia in order to detect the proportion of pseudomyopia amongst them. Tabulation of the amount of the diopteric shift in refractive error for spherical equivalent and astigmatism was also done.
Materials and Methods
The present study was a cross-sectional study in which 62 patients were evaluated. Patients attending the Ophthalmology OPD of Sri Siddhartha Medical College, Tumkur, Bangalore, Karnataka, India presenting, with low diopters of myopia (0 diopters to minus 5 Diopters of myopia), were studied.
The sample size was calculated using the formula Z2×P×(1-P)÷d2, wherein Z is the value (2.05 for a level of confidence 96%), p standard for prevalence which was taken as 0.108 and d stands for precision of 4%. The formula was used for purposive sampling.
The study was conducted from November 2018 to November 2019. The patients between 5 to 35 years of age were included in the study. Informed consent was taken from the patients and/or the guardians; the Tenents of Helsinki was followed. Ethical approval was obtained, letter reference number SSMC/PG-19/IES-5/OCT-2018.
All patients were subjected to visual acuity testing on Snellen’s Chart followed by Autorefractometry performed on UNIQUERK 100. Anterior segment examination was done on Slit lamp Biomicroscope. Following this, all patients were subjected to mydriasis and cycloplegia using homatropine (2%) eyedrops which was instilled 3 times at an interval of 10 minutes. Patients were than evaluated after 45 minutes, for a repeat autorefractometry and three consecutive reading were considered. Patients with myopia more than 5 diopters and visual acuity at presentation less than 6/12 on Snellens were excluded. Also, patient with any other Corneal ectasia, lenticular malpositions, or any other anterior and posterior segment anomalies were excluded from the study.
Statistical Analysis
The pre- and post dilatation refractometry readings were compiled and tabulated. The tables were analysed with paired t-test with SPSS-software Version 20 and conclusions were drawn.
Results
In the study, there was a female preponderance with manifestation of pseudomyopia [Table/Fig-1].
Comparing the gender presenting with low diopters of myopia.
| Gender | No of patients (n=62) | Percentage |
|---|
| Male | 29 | 46.8 |
| Female | 33 | 53.2 |
| Total | 62 | 100.0 |
The most common age group of manifestation was 21 to 25 years of age, with approximately 16 patients (25.8%) in that age group [Table/Fig-2].
Comparison of the age group which manifest with pseudomyopia.
| Age in years | Frequency | Percent |
|---|
| 0-5 | 1 | 1.6 |
| 6-10 | 2 | 3.2 |
| 11-15 | 9 | 14.5 |
| 16-20 | 13 | 21.0 |
| 21-25 | 16 | 25.8 |
| 26-30 | 13 | 21.0 |
| 31-35 | 8 | 12.9 |
| Total | 62 | 100.0 |
The study found that, the precycloplegic spherical refraction was found to range from 0.00 diopters to (-) 0.75 diopters in 30 (48.83%) of patients. Study showed maximum patients having a myopia between 0 to -0.75 diopters [Table/Fig-3], 57 (91.93%) patients had a myopia within a range of -2.00 diopters. Most of the patients were having a visual acuity from 6/6 to 6/12 range on Snellen’s Visual acuity chart.
Comparison of spherical refractive error shift before and after cycloplegia in the right eye.
The figure shows the frequency of the patients with myopia in the pre dilated state is reduced with most of them showing a hyperopic shift to within 0 to 0.75 Diopters
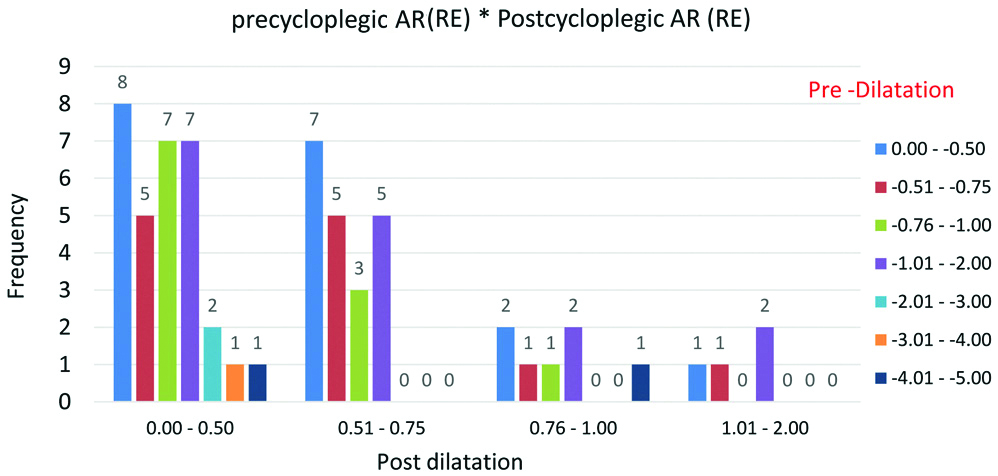
On postcycloplegic evaluation it was found that 51 patients (82.25%) had a spherical refraction in the range of 0.00 to (+) 0.75 diopter, hence it was concluded that the myopic refraction almost from 0.00 to -2.00 diopters shifted to hyperopic refraction of 0 to (+) 0.75 diopters. Hence those numbers of patients could be categorised into pseudomyopia of refractive origin. Even the myopia range of upto 5 diopters were shown to shift into hyperopia within (+) 2.00 diopters in the study.
On evaluating the left eye it was found that 39 (62.9%) patients had a myopic refractive error in the range of 0.00 to -0.75 which was the maximum among the study group. Again similar to the right eye, we had almost 57 patients within a range of -2.00 diopters in the study group [Table/Fig-4].
Comparison of spherical refractive error shift before and after cycloplegia in the left eye.
The figure shows the frequency of the patients with myopia in the pre dilated state is reduced with most of them showing a hyperopic shift to within 0 to 0.75 Diopters
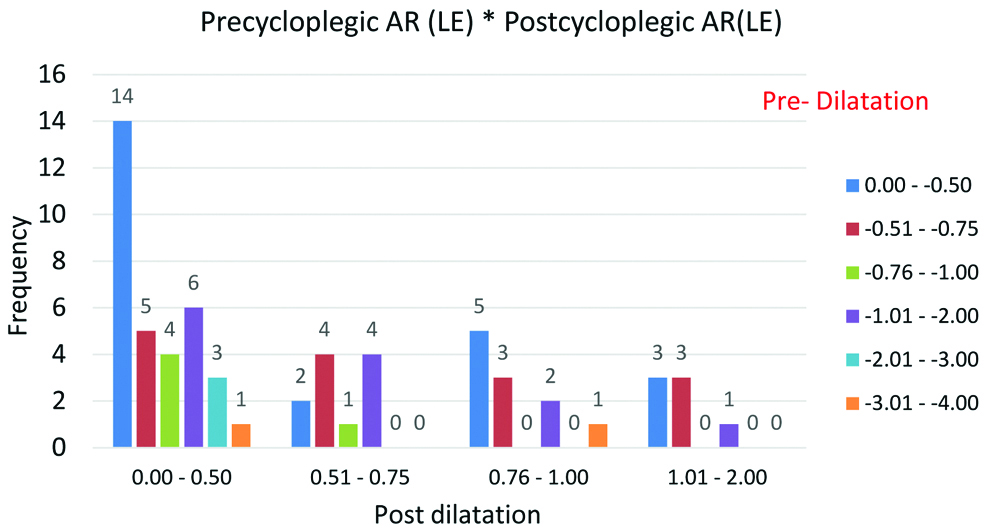
On postdilatation evaluation, 44 (70.96%) patients had a refractive error within the range of 0 to (+) 0.75 diopters, all of these can be categorised to pseudomyopia of refractive origin. It was also found that most of the patients shifted to a hypermetropia within (+) 2.00 diopters.
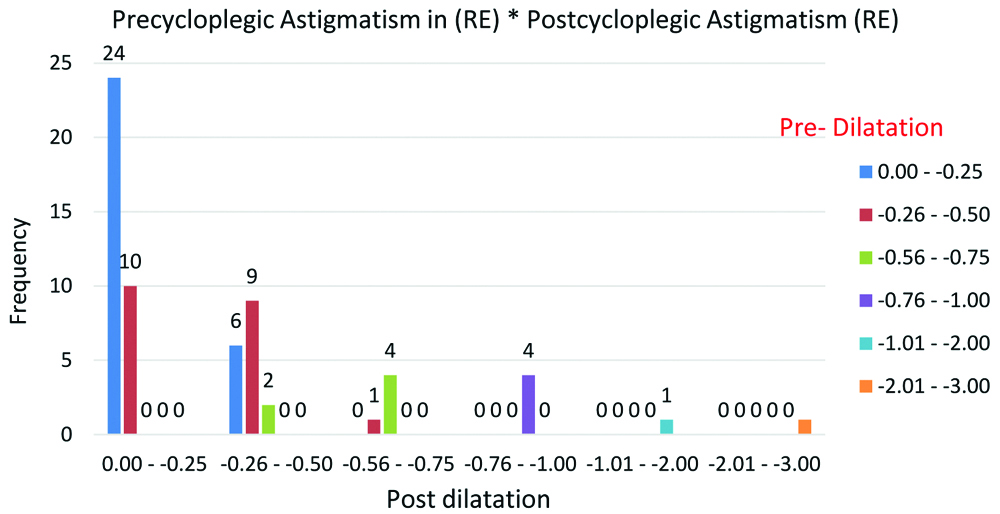
On comparing the shift in astigmatism, no change was found in the study as the astigmatism continued to stay in the range of 0.00 to (-) 3.00 diopters of cylindrical error. Also, 50 patients (80%) had a cylindrical error ranging from 0.00 to (-) 0.5 diopters pre cyloplegia. Postcycloplegia we found a refractive error to be in the range of 0.00 to (-) 0.5 diopters in almost 82.2% of the patients. Hence no significant change was found in the astigmatic refractive error in the patients [Table/Fig-5].
Graph showing the effect of cycloplegia on astigmatism in right eye.
The graph shows that most patients showed not much change in astigmatism after Cycloplegia. Most patients had astigmatism between 0.00 to -0.75 Diopters and continued to remain so Postcycloplegia
Similarly on comparing the astigmatism in the left eye, we found maximum 53 (85.48%) patients in 0.00 to -0.5 diopters, who continued in a similar diopteric value postcycloplegia. It was found that 53 (85.48%) patients continued to be to be in the 0.00 to (-) 0.50 diopters even in the postcycloplegic state [Table/Fig-6].
Graph showing the effect of cycloplegia on astigmatism in left eye.
The graph shows that most patients showed not much change in astigmatism After Cycloplegia. Most patients had astigmatism between 0.00 to -0.75 Diopters and continued to remain so Postcycloplegia.
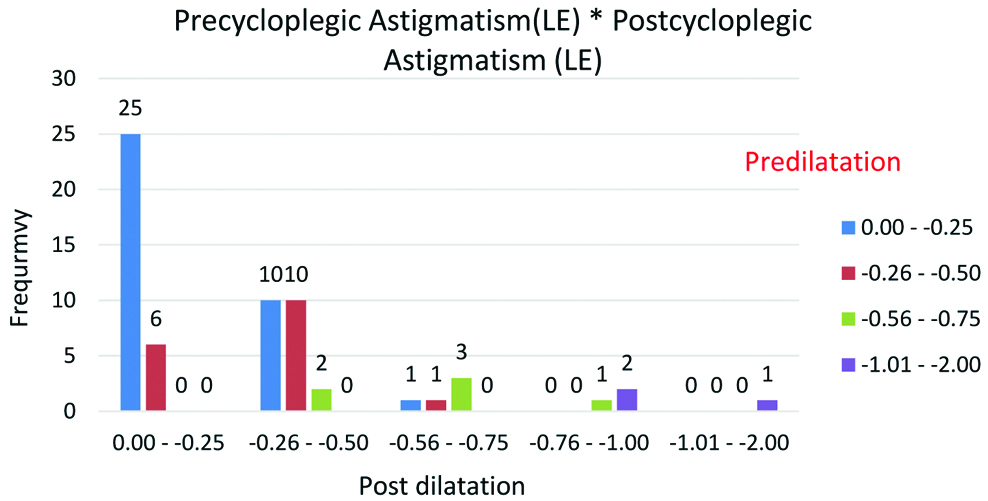
Hence in the study, in both the eyes there was no shift in the Astigmatic refractive error following Cycloplegia.
On Applying the paired t-test value to the precycloplegic and postcycloplegic spherical refraction value in the right eye the following inferences were drawn, the mean value was found to be -1.0968 in the precycloplegic phase which shifted to +0.6653 in postcycloplegia. Hence, the myopic refractive error was shifted to hypermetropia. The study showed the t-value to be -15.798, the higher value of T, suggested that there was a significant difference in the precycloplegic to postcycloplegic spherical refractive error. The p-value of <0.001 between the two groups was found to be significant [Table/Fig-7].
Table showing change in spherical error postcycloplegia.
| Pairs | Cycloplegia state | Mean | N | Std deviation | Mean difference | t-value | D.F | p-value |
|---|
| Pair 1 | Pre-cycloplegsia AR (RE) | -1.0968 | 62 | 0.83268 | -1.762 | -15.798 | 61 | <0.001 |
| Postcycloplegia (RE) | +0.6653 | 62 | 0.30683 |
| Pair 2 | Pre cycloplegic AR (LE) | -1.0000 | 62 | 0.78927 | -1.690 | -15.649 | 61 | <0.001 |
| Postcycloplegia (LE) | +0.6895 | 62 | 0.39641 |
D.f: Degrees of freedom; Std Deviation: Standard deviation; p-value- Significant value, t-value- Significance value; Paired t-test
Thus, it was found that these patients were myopic at presentation shifting to a hyperopia in the range +0.6653., with the t-value and p-value being in a significant range.
Similarly, comparing the pair 2 which represented the precycloplegic and postcycloplegic spherical refraction value in the left eye, it was found that the mean precycloplegic value of -1.000 got shifted to a value of +0.6895 in the postcycloplegic phase. The mean difference was found to be -1.690, between the precycloplegic spherical refraction and the postcycloplegic spherical refraction. The t-value was found to be -15.649, this high value suggests that there was a significant difference in the precycloplegia to Postcycloplegia spherical refractive error. The p-value was <0.001, which was significant.
Hence, the study found a significant hyperopic shift in the spherical component of refractive error in both the eyes, proving that the primary manifestation of both of them was pseudomyopia at the time of presentation.
On applying the paired t-test to the astigmatic refractive error in pair 3 which showed right eye astigmatism shift, it was found that the precycloplegic astigmatic refractive error mean shifted from -0.4194 to -0.3750, the mean difference between pre and postcycloplegic Astigmatism was found to be -0.044. The t-value being -1.898, which is not very high, indicates the shift in the astigmatic refractive error is not very significant, similarly, the p-value was 0.062, which was also not significant for the astigmatic refractive error. Hence we found that cycloplegia did not influence the astigmatic refractive error [Table/Fig-8].
Table showing change in astigmatic refractive error pre and postcycloplegia.
| Pair | Cycloplegic state | Mean | N | Std deviation | Mean difference | t-value | d.f | p-value |
|---|
| Pair 3 | Precycloplegic astigmatism in (RE) | -.4194 | 62 | .43366 | -0.044 | -1.898 | 61 | 0.062 |
| Postcycloplegic astigmatism (RE) | -.3750 | 62 | .44756 |
| Pair 4 | Precycloplegic astigmatism (LE) | -.3629 | 62 | .33778 | -0.048 | -1.689 | 61 | 0.096 |
| Postcycloplegic astigmatism (LE) | -.3145 | 62 | .36758 |
D.f: Degrees of freedom; Std Deviation: Standard deviation; p-value- Significant value, t-value- Significance value; Paired t-test
Similarly on evaluating the Pair 4, which showed precycloplegic to postcycloplegic astigmatic shift in the left eye, we found that the mean precycloplegic astigmatism shifted from -0.3629 to -0.3145, the mean difference in the precycloplegia to postcycloplegia value was -0.048. The t-value was -1.689 which is not very high hence it indicates the shift in the astigmatic refractive error is not very significant, Similarly the p-value was 0.096, which is also not significant for the astigmatism. Hence, it was found that cycloplegia did not influence the astigmatic refractive error.
Discussion
It was found that women (53.2%) were more commonly associated with pseudomyopia. In studies evaluating presbyopia and its onset, the reading distance and the depth of focus were found to be the primary factors that influence the onset of presbyopia. There is evidence that adult women have a shorter measured habitual reading distance than adult men [10,11]. Since this is habitual, it showed that women always have a shorter measured reading distance compared to the males.
This closer working distance can also act as a stimulus for more presentation of pseudomyopia in females compared to the males. This preferential near range reading can be a stimulus for over accommodation, leading to more manifestation of pseudomyopia in female gender.
Maximum patients were in the working age group of 20 to 21 years. Moreover, almost 37 (59.6%) of the cases were between 21 to 35 years. Though accommodation is known to be more powerful in the younger age than little more than half of the study population in the older age group. Hence, it was found that accommodation can be equally well functional in the older age groups as well. This over active accommodation could be the cause of pseudomyopia in the working age group, depending on their working distance and reading requirements.
Fincham E has proposed that accommodation is predominantly controlled by the lens in the eye. Hence the lenticular changes with ageing reduce the accommodative power of the eye [12]. However, the theory also suggested that the magnitude of ciliary muscle contraction required for a particular amount of accommodation also increases with age proving that both lens and ciliary muscle may show changes with ageing affecting the accommodation reflex in elderly population.
Contradicting the above study, a study by Domínguez-Vicent A et al., proposed that presbyopic ciliary muscle has the same contractile capabilities as the young presbyopic ciliary muscle [13]. Other studies have also shown that not much of change in the contractility of ciliary muscle occurs following ageing [14-16].
This theory can support the findings in the study, of more number of pseudomyopes in the age group of 21 to 25 years, which is the working age group or studying age group, though the accommodation may be more powerful in terms of range of accommodation in younger age group. Nonetheless, even the older age group has a good contractility of ciliary muscle to have a manifestation of pseudomyopia. If we consider an age range of 16 to 30, we had almost 60% of cases manifesting with pseudmyopia in that age group. Hence, we conclude that the risk of pseudomyopia will not reduce with age and the manifestation depends on the amount of near work performed by the patient. The common age of manifestation is the age group studying and actively working.
It was found that 57 (92%) patients had a myopia within a range of -2.00 diopters at presentation. Postcycloplegia the myopic refraction of the range from 0.00 to -2.00 diopters shifted to a hyperopic refraction of range from 0 to (+) 0.75 diopters in 51 patients (82.25%) [Table/Fig-3,4].
The existing basal tone of the ciliary body is known to decide the amount of adaptive accommodation that an eye can go into depending on the required near work. The basal tone of the ciliary body is known to vary according to age and refractive error amongst people [17]. Most of the studies show that the basal tone is higher in a pre-existing hyperope, and hence they are more likely to go into a tonic adaptive contraction leading to pseudomyopia [18-21].
In a study by Gwiazda J et al., hyperopic children (7-16 years of age) showed a smaller adaptive shift in their accommodation response of about 0.24 diopters after a prolonged fixation on a stimulus compared to emmetropic children who showed 0.68 diopters [19]. They also showed an inability to further accommodate among hyperopes, or attainment of a maximal tonic response in hyperopes, or a longer period of sustained accommodation required in hyperopes in order to focus. Any of these situation may hold good in an hyperope, substantiating the tonic shift in hyperopes during near work leading to pseudomyopia.
Another phenomenon known with accommodation is that the human eye employs a retinal blur to stimulate accommodation. In absence of an adequate visual stimulus, the accomodation is known to rest in a myopic posture wherein the power varies individually between the ranges of -0.5 D to -4.5 diopters. This is known as tonic accommodation. This also supports present study finding that the tone of ciliary body itself can induce pseudomyopia from -0.5 upto -4.5 diopters [22-25].
The maximum patients in the study had myopia in the range of 0.00 to -0.75 diopters. The same group postdilatation shifted to hyperopia within 0 to +0.75 diopters. There were 44 (70.96%) patients in this range, who could be categorised as pseudomyopia of refractive origin. The maximum hyperopic shift amongst the patients was found to be +2.00 diopters [Table/Fig-3,4].
Further, it was found that even a myopia upto -5 diopters was shifted to a hyperopia maximally upto +2.00 diopters. This adds to the fact that myopia upto -5 dioters can also be a manifestation of pseudomyopia [Table/Fig-3]. Maximum patients had pseudomyopia in the range of 0.00 to +0.75 diopters. Postcycloplegia 57 (91.93%) patients had a diopteric shift to a hypermetropia within +2.00 diopters [Table/Fig-3,4].
Since accommodation is a binocular phenomenon, both eyes are showing similar findings in the study. The drug used in the study was Homatropine 2% as a cycloplegic and in the both the eyes there was a hyperopia of 0 to +0.75 diopters postcycloplegia. The mean difference pre to postcycloplegia was 1.762 diopters and 1.690 diopters in right eye and left eye, respectively [Table/Fig-3].
In a study by Asharlous A et al., they found that cycloplegia induced by a single drop of cyclopentolate 1% caused a hyperopic shift in the spherical refraction by mean value of 1.17 diopters. The cycloplegic used in this study was Cyclopentolate 1%. Cycloplegia of cyclopentolate is known to be stronger than homatropine [26].
In a study by Khurana AK et al., they found that residual accommodation following cyclopentolate was 1.48±0.33 as compared to homatropine which had 2.32±0.37 as residual accommodation [27].
The shift in astigmatism following cycloplegia in right eye was evaluated; however no change in the astigmatic refractive error was seen following cycloplegia. The study showed almost 50 patients (80%) were having a cylindrical error ranging from 0.00 to (-) 0.5 diopters precycloplegia. In the postcycloplegic state the refractive error was found to be in the range of 0.00 to (-) 0.5 diopters in almost 82.2% of the cases. Hence there was no change in astigmatism following cycloplegia [Table/Fig-5].
The change in astigmatism in left eye following cycloplegia was evaluated and it was found that maximum 53 (85.48%) patients were showing an astigmatism in the range of 0.00 to -0.5 diopters pre cycloplegia, which continued in a similar diopteric value postcycloplegia as well [Table/Fig-6].
In the study out of 62 patients, only 49 patients were found to have recorded an astigmatism in right eye. Amongst them 36 patients showed bi-oblique astigmatism, 8 showed with the rule astigmatism while 5 showed against the rule astigmatism. Hence, in both the eyes no shift in the astigmatic refractive error was seen following cycloplegia.
In a study by Ashourlas A et al., they found that the astigmatism changed especially in the vertical and the horizontal meridian following cycloplegia. However, the oblique astigmatisms remained same in their study as well [26].
Several factors can be responsible for astigmatism change with cycloplegia. The proposed causes include accommodative astigmatism, subject’s head positioning, and higher order aberration. Increment in dilated pupil and different astigmatism vectors in different centrifugal rings in the visual axis during dilatation have been also reported to cause astigmatism shift [26].
Paired t-test was applied to pre and postcycloplegic spherical refraction values in [Table/Fig-7]. The t-value and the p-value were found to be significant for both the eyes. This shows that significant hyperopic shift in the spherical component of refractive error occurs in both the eyes proving that the primary manifestation of both of them was pseudomyopia at the time of presentation.
These findings also suggest that low diopters of myopia shift to hypermetropia following cycloplegia. These findings support the fact that hyperopia of low diopters can manifest with myopia or pseudomyopia which can only be detected with cycloplegia.
On applying paired t-test to pre and postcycloplegic astigmatic refractive error it was found to be non-significant, showing that astigmatism was unaffected by cycloplegia.
A study by Ashlarous A et al., showed that cycloplegia causes statistically significant change in vertical and horizontal astigmatism. However, they found that the oblique and the bi-oblique astigmatism were unaffected by cycloplegia [26]. Similar findings were also seen by Jorge J et al., [28].
On evaluating the astigmatic refractive error in this study group, it was found that 49 out of 62 patients showed astigmatism in the right eye, amongst whom 36 (73.46%) patients had a bi-oblique astigmatic axis, 8 (16.3%) had with the rule astigmatism (vertical) and 5 (10.2%) had against the rule astigmatism (horizontal).
Similiarly, out of 48 patients who had an astigmatism in the left eye showed 34 (70.83%) had Bi-oblique astigmatism, 8 (16.66%) had with the rule astigmatism (vertical), and 6 (12.5%) had against the rule astigmatism (horizontal).
It has also been proposed that with the rule astigmatism (WTR) changes due to lens tilt around the horizontal axis following cycloplegia. This is further substantiated by changes due to sectorial contractions in ciliary muscle, lens and zonules, extraocular muscles and lens tilt. Since these changes are a part of the accommodation reflex in the eye, the absence of the reflex by cycloplegic drugs may affect the magnitude or the dioptoric value of astigmatism with respect to the pre-cycloplegic value of astigmatism [29].
Carkeet A et al., showed higher order aberrations are known to cause a change in refractive astigmatism which is more evident in with the rule astigmatism and oblique astigmatism, and are known to depend on the variable dilatated state of the pupils [30].
In a study by Marcos S et al., they showed that higher order aberrations worsen the focus in astigmatic eyes especially in with the rule and against the rule astigmatisms. This varies with the dilatation of the pupil [31].
Hence most of the studies in literature show that cyloplegia predominantly affects, with the rule and against the rule astigmatism compared to oblique and bi-oblique astigmatism. This was in accordance to present study findings of no change in astigmatism as maximum of our patients had Oblique and Bi-oblique astigmatism.
Limitation(s)
The study population was small, and only included the patients presenting with pseudomyopia to the hospital. Detailed evaluation of astigmatism was not done in the study, this if pursued might further enhance our knowledge regarding cycloplegia effects.
Conclusion(s)
The study showed that low diopters of hyperopia predominantly manifest as myopia which can be termed as pseudomyopia of refractive origin. The presenting myopia was found to range upto -0.75 diopters of spherical error commonly. The presenting vision ranges between 6/6 to 6/12 on Snellen’s chart, which is near normal, and the commonest age was between 21 to 25 years. Hence, we propose that this range of myopia and vision should be suspected to have pseudomyopia which mandates a cycloplegic refraction irrespective of the age of presentation.
We also found that cycloplegia did not affect the astigmatism as much as it does the spherical refractive error.
D.f: Degrees of freedom; Std Deviation: Standard deviation; p-value- Significant value, t-value- Significance value; Paired t-test
D.f: Degrees of freedom; Std Deviation: Standard deviation; p-value- Significant value, t-value- Significance value; Paired t-test