In order to combat various endodontic, prosthetic and surgical issues, tooth extraction is the most often used oral maxillofacial surgical procedure. Some treatment plans in orthodontics involve tooth extractions. Although tooth extractions are carried out frequently, patients often believe that it causes a lot of pain. This leads to anxiety and stress, which makes the whole extraction procedure tough for the patient as well as the dentist. The patient being awake during the procedure makes it even more difficult [1].
Pain is defined as an uncomfortable sensory and emotional experience with actual or potential tissue damage [2]. According to McAloon C et al., pain is considered as a subjective feeling, whereas according to Closs SJ et al., pain is a complex experience [3,4].
One of the most essential prerequisites of dentistry is successful control of pain during all dental procedures. In dentistry, the fear of pain has been controlled by using local anaesthetics. They block nerve conduction only temporarily without altering the consciousness of the patients. However intra operative or post-operative pain still occurs in a few patients as the pain threshold varies from patient to patient and also on the efficacy of the local anasthetic used.
In 1943, Lofgren synthesised the first modern Local Anaesthetic (LA) agent Lignocaine [5]. In modern dentistry, Lignocaine is considered as a gold standard for pain management. Anaesthesia can be achieved by local infiltration as well as by nerve block. But local infiltration has its own limitations and cannot be used in all situations like in cases of inflammation. On the other hand, nerve block provides profound deep anaesthesia and can bypass situations like local infection at the extraction site [6].
Infraorbital nerve block anaesthetises incisors, cuspids, bicuspids and mesiobuccal root of maxillary first molar on the side injected. On the other hand, GP nerve block anaesthetises posterior portion of the hard palate upto the first bicuspid area on the side injected [5].
Thus, the use of Greater Palatine (GP) nerve block for palatal anaesthesia along with infrarbital nerve block is a well-known procedure for orthodontic extraction of maxillary first premolar. Since GP nerve block is rather a painful injection, some techniques such as pressure, electronic, cryogenic or topical anaesthesia have been suggested to reduce patient’s discomfort [6,7]. However, these methods are not universally effective and GP nerve block for palatal anaesthesia remains a painful experience specially in case of children [8]. There is sparse literature with regard to the diffusion property of lignocaine HCl and their use as infraorbital nerve block for orthodontic extraction of first premolar without GP nerve block [8-10].
The aim of the present split-mouth prospective study was to evaluate the anaesthetic efficiency of Infraourbital nerve block with and without Greater Palatine anaesthesia during orthodontic extraction of maxillary first premolar.
Materials and Methods
The present prospective, randomised study using a split-mouth design was conducted in the month November 2019 to January 2020 on 60 patients with age group range from 12-18 years; who presented to the Department of Oral and Maxillofacial Surgery, SGT University, Gurugram for bilateral maxillary premolar tooth extraction required for orthodontic purpose. The prior approval of Institution Ethical Committee (SGTU/FDS/24/1522-A dated 25th October, 2019) was taken and informed consent was obtained from all the patients or their parents for minors.
Exclusion Criteria: Patients were excluded if they had pre-existing systemic disease such as hypertension, diabetes or bleeding disorders, allergies to local anaesthetics, pregnancy or suspected pregnancy, and orthodontic patient’s taking pain relief medicines, undergoing fixed prostheses, extensive fillings, and endodontic treatment.
The nerve block were allocated to different sides by generating randomisation list using GraphPadStatMate version 1.01i (GraphPad Software, Inc., Armonk, NY: IBM Corp).
The patients were scheduled for extraction at 2 separate clinical sessions (1 side at a time) 1 week apart. The study was conducted over a period of 3 months.
Surgical Procedure
Before the procedure, all the patients were checked for normal vital signs. A detailed medical history was obtained by conducting clinical examinations. A 1.8 mL of lignocaine HCl (2% Lignocaine HCl with 1:80000 Adrenaline (XICAINE®) for infraorbital nerve block (using intraoral premolar approach) was administered on 1 side (Experimental group) and on the other side (control group) 0.5 mL lignocaine HCl (2% Lignocaine HCl with 1:80000 Adrenaline (XICAINE®) on palatal side (1 cm from the palatal gingival margin towards the midline of the palate between second and third molar) for greater palatine nerve block in addition to 1.8 mL lignocaine HCl for infraorbital nerve block was administered. All injections were given using 25 gauge 3 mL disposable syringe and the rate of anaesthetic delivery was 1 mL every 1 minute.
All extractions (total 120 maxillary first premolar teeth, 60 in each group) were performed by single surgeon under standard extraction protocol which includes checking for subjective symptoms and objective symptoms after 10 minutes of nerve block at the site of extraction using periodontal probe. The post-operative medication i.e., 400 mg of oral ibuprofen three times a day for three days and instructions were carefully explained to the patients. They were informed that they should contact the surgeon if any complications such as severe pain or bleeding occurred. None of the extractions required bone removal, flap raising or suture placement. It was planned to exclude patients who required additional injection from the present study but none of the patients actually required.
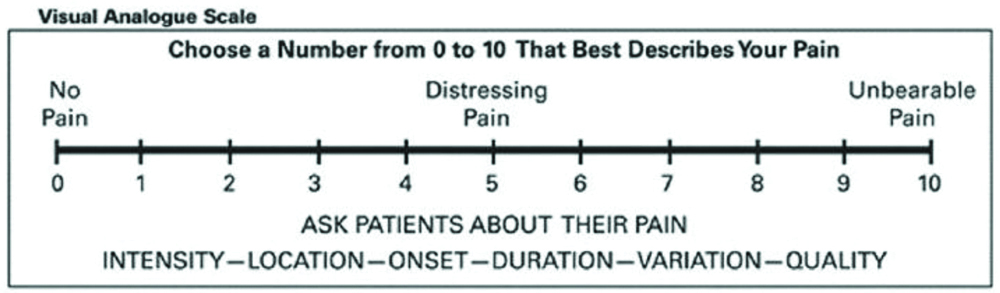
The patients were explained about the scoring system on Visual Analog Scale (VAS) [Table/Fig-1] [11]. VAS was recorded 10 minutes after injection of local anaesthesia. The degree of pain was assessed using a 100 mm VAS ranging from 0 to 10. For the degree of pain, 0 indicated no pain and maximum pain was given score 10. VAS score was recorded by the investigator other than the operating surgeon to reduce bias in the study. Cronbach’s alpha value 0.938 showed good degree of intra-examiner reliability. Post-operative analgesic i.e., 400 mg of oral ibuprofen was used as a rescue medication. All the patients completed the study before taking any medication.
Statistical Analysis
The data were entered in the Microsoft excel spreadsheet 2013. Student’s unpaired t-test analysis was performed using IBM SPSS Version 24.0 (Armonk, NY: IBM Corp.).
The VAS scores by unpaired t-test was calculated. p-value <0.05 was considered as statistically significant.
Results
According to VAS scores of all 60 patients (28 male and 32 female, mean age of 15 years) [Table/Fig-2], the pain elicited during orthodontic extraction of maxillary first premolars with palatal injection and without palatal injection were compared by unpaired t-test. The VAS scores by unpaired t-test was statistically non-significant with p-value 0.868.
Demographic and surgical variables.
| Variable | Patients (n) |
|---|
| Gender |
| Male | 28 |
| Female | 32 |
| Mean age | (12-18 years) 15 years |
| Extracted maxillary first premolar | 120 |
| Experimental group | 60 |
| Control group | 60 |
Thus, the difference in the pain perceived by the patients in experimental and control group was not found to be statistically significant [Table/Fig-3].
Comparison of VAS Pain Score between the infraorbital nerve block with and without palatal injection (Unpaired t-test).
| Group | Total number of patients | Mean | Standard deviation | t-value | p-value |
|---|
| VAS score on a scale of 0-100 mm | Experimental group | 60 | 29.00 | 10.688 | 0.167 | 0.868 |
| Control group | 60 | 29.33 | 11.179 |
p>0.05- Non Significant (NS); p≤0.05- Significant (*); p≤0.01- Highly significant (**) p≤0.001- Very highly significant (***); VAS: Visual analog scale
Discussion
Pain free dentistry is the need of the hour, and when our dental procedure involves treatment specially in children, then it is of prime concern. Pain can be controlled by effective anaesthetics and anaesthesia techniques. However, inspite of using effective anaesthetics, patients still fear getting dental procedures done owing to the possibility of experiencing pain. A few patients constantly defer their treatment due to the same, at the cost of bearing more pain from the dental problems itself [3,6].
Although dental extraction is not so common in teenage patients but, in cases of different types of malocclusion which requires some kind of active orthodontic intervention, it is commonly performed procedure.
So, in patients undergoing extraction due to orthodontic treatment, plays a major role of creating space in cases of excess tooth material. Out of all surgical goals of orthodontic extraction, the most important is to make the procedure as less traumatic as possible by inducing least trauma to the surrounding structures e.g., Soft tissue, bone, adjacent teeth etc. [12].
To achieve these goals, retraction of both buccal and palatal flaps is not advised to maintain height of the crestal bone (to preserve blood supply to crestal bone from gingival tissue). Even, avoiding a single prick of needle in teenage patient plays a very major role in raising morale of the patient while undergoing any minor surgical procedure. This can be achieved by modifying the treatment like, avoiding palatal injection in patients undergoing maxillary orthodontic extractions [13,14].
The palatal injection is mild to moderately painful and has reported relatively poor tolerance by patients who have experienced this procedure. Various techniques have been advocated in the literature to reduce the pain of intraoral injections out of which, application of topical anaesthetic being a frequently used option. However, it is effective only upto a tissue depth of 2-3 mm and the deeper tissues are poorly anaesthetised. This pain appears to be caused due to displacement of the firmly adhered palatal tissues to the underlying bone [15,16].
Since, the study does not involve working in the palatal gingiva of maxillary premolar tooth beyond gingival sulcus, hence it is not required to give GP nerve block in orthodontic maxillary premolar extraction cases [16]. The biological plausibility of the infraorbital nerve block injection depends on the penetration of the anaesthetic solution into the palatal tissues and its diffusion through pores in the cortical bone of the posterior maxilla and various nutrient canals. The anaesthetic efficiency could be influenced by the variations of the presence of nutrient canals, as well as the density, porosity and thickness of the cortical plates [17].
Maxilla has low bone density than mandible and because of its high porosity buccal maxilla facilitates the diffusion of lignocaine HCl. Thus, Maxillary tooth removal can be performed without palatal injection. Also lignocaine HCl is lipid soluble, thus, it diffuses through soft tissues [16,18]. Second, it has been claimed that sufficient palatal tissue anaesthesia can be provided using lignocaine as a maxillary buccal infiltration, since it diffuses readily through soft and hard tissues than other local anaesthetics [19,20,21]. Third, the anaesthetic requirement for maxillary premolar tooth extraction is not as high as that required for other extractions [22].
Sekhar GR et al., found no significance statistically in control and study groups and concluded that maxillary tooth extraction is possible by depositing 2 mL of lignocaine to the buccal vestibule of the tooth without the need for palatal anaesthesia [6]. Uckan S et al., conducted a similar study on 53 patients, and concluded that success rates were not statistically significant when permanent maxillary tooth removal was performed with and without palatal injection [20]. Sharma M et al., based on the results of VAS and Facial Pain Scale (FPS) in their study, observed similar results as seen in the present study, which states that permanent maxillary premolar teeth can be extracted by giving only buccal anaesthesia using 2% lidocaine, without palatal anaesthesia [9].
Fan S et al., have observed that deposition of 1.7 mL of 4% articaine HCl with 1:100,000 epinephrine into the buccal vestibule provides similar clinical anaesthetic efficacy as compared to the routine type of anaesthesia with palatal injection for maxillary tooth removal [8]. Badcock ME and McCullough MJ has stated that the length of time taken while performing extraction had a significant impact on the level of pain experienced by the patients [23]. In this study, administration of infraorbital nerve block injection of lignocaine HCl with and without GP nerve block for orthodontic extraction of maxillary first premolar showed similar statistical results, which are same as that of the previous study conducted by other authors [6,8,9].
Limitation(s)
Primarily, sample size in this study was less, and VAS scores of injecting anaesthetic solution and post-extraction both should have been considered and tabulated for better understanding of anaesthetic efficacy in experimental group. Post-extraction VAS score was not recorded hourly. Along with this, satisfaction and wound healing scores were not recorded after extraction.
Conclusion(s)
In this study, there was no statistically significant difference in the pain perceived during extraction procedure when infraorbital nerve block was given with or without palatal injection. This study was done to avoid an additional needle prick of GP nerve block along with infraorbital nerve block while performing maxillary orthodontic first premolar extraction.
This is only a preliminary study, more studies with larger sample size must be conducted in future. In future, this alternative method of avoiding greater palatine nerve block can be used in young patients to avoid their fear of multiple injections.
p>0.05- Non Significant (NS); p≤0.05- Significant (*); p≤0.01- Highly significant (**) p≤0.001- Very highly significant (***); VAS: Visual analog scale