The Femoral Artery Pseudoaneurysm (FAP) is an iatrogenic complication occurring at the femoral arterial puncture site during invasive cardiovascular procedures. Various studies have observed their incidence to be 0.1% to 0.2% for diagnostic angiograms and 0.8% to 2.2% for interventional procedures [1,2]. The recent rise in incidence of FAP has been attributed to more frequent use of thrombolytics, anti-platelets, anti-coagulants and large bore cannulas for interventional procedures [1]. Pseudoaneurysms occurs if arterial puncture site does not seal, leading to leakage of arterial blood into the surrounding tissues, gets contained by haematoma and the pressure of surrounding tissues and form a perfused sac (the false lumen) connected to the supplying artery by a “neck” [3]. It can present as localised swelling or pulsatile haematoma, a new thrill or bruit, or marked pain or tenderness. Complications of pseudoaneurysms include rupture leading to catastrophic bleeding, local pain, infection, skin necrosis, distal embolisation, compression neuropathy, and distal limb ischaemia [3].
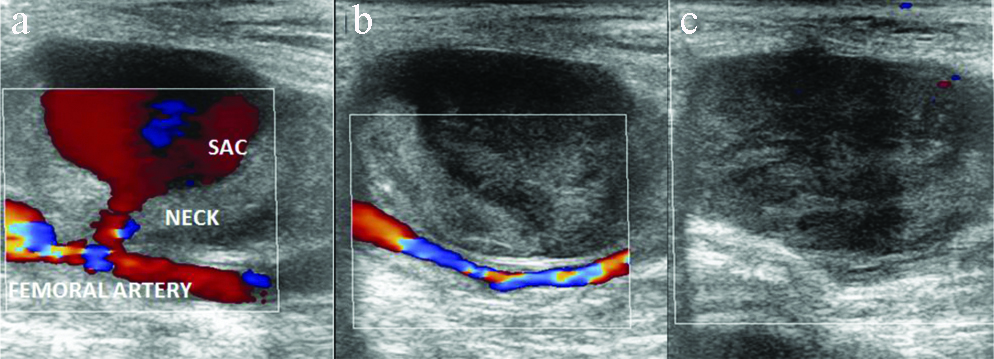
Ultrasound with colour doppler imaging is the modality of choice for diagnosis of pseudoaneurysm. Typical characteristics of pseudoaneurysm include colour flow within a tract leading from the artery to the sac, swirling colour flow within sac and a typical to-and-fro Doppler waveform (“the yin-yang sign”) in the pseudoaneurysm neck [Table/Fig-1,2a]. Morgan R and Belli AM in their study stated that colour Doppler ultrasound is 94% to 97% sensitive in diagnosing peripheral pseudoaneurysm [4].
It is possible for small pseudoaneurysms (less than 2 cms in diameter) to thrombose spontaneously within four weeks [5], but this spontaneous resolution is unpredictable, and the watch-and-wait policy may reduce patient’s activity and delay discharge, prompting an early active management of most pseudoaneurysms. Fellmeth BD et al., first described UGCR [6]. Since then it has been proved to be a safe and cost-effective method for achieving pseudoaneurysm thrombosis, with a failure rate of 10-35% [6-8]. This article is aimed at sharing seven years’ experience of performing UGCR to treat FAP in a research cardiac institute. Various predictive factors for successful versus failed UGCR are also discussed, though remain controversial. An attempt was made to include angle of neck in relation to underlying artery of origin as one of the predicting factors, and to the best of current available knowledge till date none of major studies have addressed it.
Materials and Methods
A retrospective, observational study was conducted at UN Mehta Institute of Cardiology and Research Center, Ahmedabad, Gujarat, India from December 2012 to November 2019 after approval of the ethical committee of the institute (UNMICRC/ALLIED/2019/04.).
Inclusion Criteria: Out of 1,55,000 total femoral punctures performed for various diagnostic and therapeutic procedures by different operators during seven years period from December 2012 to November 2019, ultrasound were performed for evaluation of local site (groin region) in patients having local site swelling or pain or bruit on clinical examination were included. Chronic pseudoaneurysm (>28 days), were also enrolled.
Exclusion Criteria: Patients with pseudoaneurysms above the inguinal ligament, presence of a puncture site infection, or a limb threatened by vascular compromise were excluded. Seven patients fell in exclusion criteria- five due to local site infection, one due to pseudoaneurysm above the inguinal ligament and one due to limb threatened by vascular compromise.
Total 310 pseudoaneurysms were detected out of 1,55,000 total femoral punctures (0.2% incidence). All the patients who were diagnosed on same day of the procedure were given tight compression bandage and re-evaluated after 24 hours to look for presence or absence of spontaneous thrombosis. Out of 310 pseudoaneurysms, 53 of them were of small size and thrombosed spontaneously on 24 hours follow-up and tight compression bandage.
A high frequency of 10 MHz linear probe of colour ultrasound (Philips HD 15, USA) was used to confirm the diagnosis of a pseudoaneurysm. Local anaesthetic agent was used as and when required. Intravenous analgesics were not needed in any of patients. Manual compression was given with a 10 MHz linear probe to obliterate flow in the pseudoaneurysm neck while still allowing flow through the underlying femoral artery for 10 minutes intervals [Table/Fig-2b,c,3]. After some time the pseudoaneurysm was rechecked for occlusion and peripheral pulses were reassessed. If flow was still present, the procedure may be repeated at most three times (30 minutes’ compression) in one cycle. A successful repair was considered when complete thrombosis of the sac was achieved [Table/Fig-4,5]. If complete thrombosis was not achieved, same cycle was repeated next day. Maximum four cycles were attempted before labelling patient as failure. A study by Huang TL et al., have attempted total three cycles of 45 minutes duration (45×3=135 minutes) [9]. In present study it was modified to 30 minutes per cycle to total four cycles (30×4=120 minutes). In those patients where complete thrombosis was achieved, patients were confined to bed rest in the hospital for 24 hours with a compression bandage. Rechecking of the arterial flow was considered on the following day before discharge and after one month to detect any recurrence. No procedure related complications were encountered.
Doppler ultrasound image showing: a) Femoral artery of origin with patent neck and pseudoaneurysm sac; b) During compression no flow within sac while flow present within underlying femoral artery; c) Post successful compression completely thrombosed sac with no flow within.
Doppler ultrasound image showing: a) Femoral artery of origin with patent neck and pseudoaneurysm sac; b) Post successful compression completely thrombosed sac with no flow within.

Doppler ultrasound image showing: a) Femoral artery of origin with patent neck and pseudoaneurysm sac; b) Post successful compression completely thrombosed sac with no flow within.

Age, gender, procedure performed, artery of origin, duration of the pseudoaneurysm, the size and area of the pseudoaneurysm sac, the width and length (from the pseudoaneurysm to the origin from femoral artery) and angle of neck of the pseudoaneurysm and time required for complete thrombosis were evaluated.
Statistical Analysis
All statistical tests were carried out using IBM SPSS program version 20. Mean±SD values were used to express Quantitative variable and percentages were used to express Qualitative variable. Association between angle and neck width, duration of aneurysm and mean time of successful compressions was done using chi-square test.
Results
The mean largest dimension of the pseudoaneurysms sac was 3.5±1.83 cm (range 1-8 cm) and mean sac area was 9±7.31 cm2 (range 1-36 cm2) [Table/Fig-6].
Parameters of 250 patients who underwent UGCR.
| Variables | | N=250 (%) or Mean±SD |
|---|
| Gender | Male | 135 (54) |
| Female | 115 (46) |
| Location | CFA | 241 (96.4) |
| SFA | 8 (3.2) |
| DFA | 1 (0.4) |
| Side | Right | 210 (84) |
| Left | 40 (18) |
| Success | Successful | 235 (94) |
| Failure | 15 (6) |
| Age | | 60±7.84 years (Range: 41-70) |
| Sac size | | 3.5±1.83 cm (Range: 1-8 cm) |
| Sac area | | 9±7.31 cm2 (Range: 1-36 cm2) |
| Neck width | | 2.3±1.15 mm (Range: 0.5-6 mm) |
| Neck length | | 11±6.07 mm (Range: 1-26 mm) |
| Duration of aneurysm | | 2±3.9 days (Range: 1-46 days) |
| Mean time required | | 26±25.27 min (Range: 6-110 min) |
| Procedure | Diagnostic coronary angiography | 75 (30) |
| Therapeutic coronary angiography with stent placement | 140 (56) |
| Therapeutic peripheral angiography | 32 (12.8) |
| Intra-Arterial Balloon Pump (IABP) | 3 (1.2) |
CFA: Common femoral artery; SFA: Superficial femoral artery; DFA: Deep femoral artery
Successful thrombosis of the pseudoaneurysm was achieved in <60° angle (97.1%) compare to >60° angle (27.3%). The difference between two groups was statistically significant (p<0.0001). Neck width, duration of aneurysm and mean time of successful compressions was also associated with <60° angle (p<0.0001) [Table/Fig-7].
Neck width, duration of aneurysm and mean time of successful compressions and their association with angle (p<0.0001).
| Angle <60° N=239 | Angle >60° N=11 | p-value* |
|---|
| Successful | 232 (97.1) | 3 (27.3) | <0.0001 |
| Failure | 7 (2.9) | 8 (72.7) | |
| Sac size | 3.5±1.85 cm | 3.5±1.32 cm | 1 |
| Sac area | 8.88±7.17 cm2 | 11.55±10.06 cm2 | 0.24 |
| Neck width | 2.24±1.1 mm | 3.58±1.41 mm | <0.0001 |
| Neck length | 11.14±6.06 mm | 7.91±5.67 mm | 0.08 |
| Duration of aneurysm | 1.72±2.07 days | 8.18±15.22 days | <0.0001 |
| Mean time of successful compression | 23.43±19.97 min | 81.91±53.04 min | <0.0001 |
*Calculated by using chi-square test
The mean compression time of the successful compressions was 26±25.27 minutes (range 6-110 minutes). Successful thrombosis of the pseudoaneurysm was achieved in 235 (94%) patients. Of the 15 patients who underwent surgical treatment, 10 patients had failed UGCR, three failed due to development of local infection, one patient refused treatment after one UGCR cycle, one patient required ventilation due to worsening of his primary cardiac condition. Parameters of 15 UGCR failure group are summarised in [Table/Fig-8].
Parameters of UGCR failure group.
| No. | Artery of origin | Compression time | Outcome | Largest sac dimension Mean-4.2 cm | Neck width Mean-4.4 mm | Neck length Mean-9 mm | Neck angle |
|---|
| 1 | CFA | 120 min | Failure | 4.5 cm | 5.5 mm | 1 mm | >60° |
| 2 | CFA | 120 min | Failure | 3 cm | 4 mm | 8 mm | >60° |
| 3 | CFA | 120 min | Failure | 6 cm | 3.8 mm | 10 mm | >60° |
| 4 | DFA | 120 min | Failure | 4 cm | 4.3 mm | 23 mm | <60° |
| 5 | CFA | 120 min | Failure | 2.5 cm | 4.5 mm | 2 mm | >60° |
| 6 | CFA | 120 min | Failure | 3.8 cm | 5 mm | 4 mm | >60° |
| 7 | SFA | 120 min | Failure | 4.3 cm | 4.1 mm | 5 mm | >60° |
| 8 | CFA | 120 min | Failure | 4.5 cm | 3.9 mm | 5 mm | >60° |
| 9 | CFA | 120 min | Failure | 3.8 cm | 4.5 mm | 15 mm | <60° |
| 10 | CFA | 120 min | Failure | 5.5 cm | 4.4 mm | 18 mm | <60° |
| 11 | CFA | Only 1 cycle attempted | Development of local site infection | 2.8 cm | 5.5 mm | 9.5 mm | <60° |
| 12 | CFA | Only 1 cycle attempted | Development of local site infection | 3 cm | 5 mm | 8.6 mm | <60° |
| 13 | CFA | Only 1 cycle attempted | Development of local site infection | 4.3 cm | 4.4 mm | 7.2 mm | <60° |
| 14 | CFA | Only 1 cycle attempted | Patient refused | 5 cm | 4 mm | 8.3 mm | <60° |
| 15 | CFA | Only 1 cycle attempted | Required ventilation due to worsening of his primary cardiac condition | 6 cm | 4.1 mm | 10.4 mm | >60° |
CFA: Common femoral artery; SFA: Superficial femoral artery; DFA: Deep femoral artery
All 235 patients who had successful UGCR further had 24-hour and one month follow-up colour ultrasound and all of them were found to be asymptomatic with no evidence of recurrence.
Discussion
UGCR of the pseudoaneurysm neck with simultaneous thrombin injection is currently the method of choice in many centres because of its ease, rapidity, and minimal discomfort, with success rate ranging between 86% and 100% [10].
In this study mean largest dimension of sac in success group was 3.5 cm and in failure group was 4.2 cm. According to Coley BD et al technical success was 87% for pseudoaneurysms whose dimension was 4 cm or less and it was only 62% for lesions more than 4 cm [11]. Similar findings was observed by Eisenberg et al., [3]. It is hypothesised that flow through a large sac tends to be greater than flow through a small sac and therefore difficult to obliterate completely. However, largest mean sac dimension with successful UGCR in this study was 8 cm and few <4 cm size sac had failed UGCR. No correlation between the pseudoaneurysm size and the therapeutic success were found in studies by Huang TL et al., [9] and in Schaub’s series [12]. Mean neck length in success group was 11 mm and in failure group was 9 mm. Schaub F et al., in his series noted that short length of the neck (<10 mm) is a factor which is likely to result in unsuccessful compression and in present study also same was observed [13]. The mean width of pseudoaneurysm neck in success group was 2.3 mm and in failure group was 4.4 mm. Various previous studies have concluded that wide pseudoaneurysm neck (>4 mm) is also a factor which is likely to result in unsuccessful compression [9,13].
This study explored the angle of neck in relation to underlying artery of origin as one of the predicting factors, and to the best of knowledge till date none of studies have addressed it. Cut-off value of <60° was associated with high success rate. In success group 232 patients had angle <60° and only 3 patients had angle >60°. In failure group, only seven patients had angle <60° and while eight patients had angle >60°.
None of the patients was asked to stop anticoagulants in this study and did not keep data of the International Normalised Ratio (INR) as almost all of patients had cardiac pathology requiring strict continuation of anticoagulants and many previous studies have failed to consider it to be significant factor in success of UGCR. Schaub F et al., reported a 54% success rate in patients who used anticoagulants (INR, 2.5-6.0) versus 93% in patients who did not use anticoagulants [12]. They showed no significant correlation between INR at the time of UGCR and the therapeutic success rate, with a p-value of 0.014 (in their series, p<0.01 was defined as significant).
The chronicity of a pseudoaneurysm will decrease the thrombogenicity of the track due to the development of endothelium. So previously pseudoaneurysm> 28-day-old has been regarded as untreatable by UGCR. However, many studies have shown that pseudoaneurysm age should not be considered as a predictive factor of technical success [3,10]. In this study, the mean duration of presentation in success group was two days while nine days in failure group. It was concluded that chronicity is not a predictive factor but chronic pseudoaneurysm require longer compression time. The mean time required for successful compression was 26 minutes in this study. While for those pseudoaneurysms >28 days, mean time was 60 minutes in this study. Factors like the presence of a large surrounding haematoma, associated arteriovenous fistula, the size of arterial sheath used and the presence of underlying femoral artery disease do not affect outcome [11,14]. Comparison of this study with two major studies’ results are summarised in [Table/Fig-9].
Comparison of results with various studies [9,14].
| Parameter assessed | Cox GS et al., [14] | Huang TL et al., [9] | Present study |
|---|
| Mean largest dimension | Mean: 2.2 cmRange: 0.5 to 5.2 cm | Mean: 3.6 cmRange: 1 to 9 cm | Mean: 3.5 cmRange: 1 to 8 cm |
| Sac area | Not studied | Mean: 7.3 cm2Range: 0.5 to 31.5 cm2 | Mean: 9 cm2Range: 1 to 36 cm2 |
| Duration of aneurysm | Mean: 7.6 daysRange: 1 to 80 days | Not studied | Mean: 2 daysRange: 1 to 46 days |
| Mean time required | Mean: 33 minRange: 10 to 120 min | Mean: 21.2 minRange: 8 to 45 min | Mean: 26 minRange: 6 to 110 min |
| Neck length | Not studied | Mean: 3.3 mmRange: 1.1 to 20.2 mm | Mean: 11 mmRange: 1 to 26 mm |
| Neck width | Not studied | Mean: 2.1 mmRange: 1 to 5 mm | Mean: 2.3 mmRange: 0.5-6 mm |
| Neck angle | Not studied | Not studied | <60°: 222>60°: 13 |
| Success rate | 94% | 90.5% | 94% |
Though UGCR is overall a safe procedure, Eisenberg L et al., had reported a 3.6% complication rate [3]. Common complications include acute enlargement of the pseudoaneurysm, rupture, vasovagal response, deep vein thrombosis, acute hypertension, and angina. Femoral artery thrombosis after simultaneous temporary occlusion of the underlying artery had also been reported previously [6]. No procedure-related complications were encountered in this study. However, due to large number of participants this study offer conclusive results and a study of new parameter- angle of neck of pseudoaneurysm adds new knowledge in current concept.
Limitation(s)
This study may have few limitations: 1) Patients coagulation status was not corrected; 2) All the UGCR was not carried out by single radiologist; 3) It is possible that many of small lesions may have gone undiagnosed or closed spontaneously so true incidence cannot be estimated reliably; 4) Comparative assessment of simple UGCR with UGCR of the neck and simultaneous thrombin injection was not done.
Conclusion(s)
In present study width and angle of pseudoaneurysm neck was found to be the most reliable predictive factor for technical success and UGCR procedure is considered as safe, cheap and reliable technique to treat post procedure FAP.
CFA: Common femoral artery; SFA: Superficial femoral artery; DFA: Deep femoral artery
*Calculated by using chi-square test
CFA: Common femoral artery; SFA: Superficial femoral artery; DFA: Deep femoral artery