Sedation is a continuous spectrum ranging from anxiolysis to general anaesthesia. Stress factors in operation room and with surgical procedure may contribute to discomfort, anxiety and restlessness in patients under regional anaesthesia [1].
Sedation requires vigilant monitoring of the patient. Methods of monitoring the depth of sedation are: qualitative method (observer’s assessment of awareness/sedation OAA/S scale) and quantitative method {Bispectral Index (BIS)} [2]. BIS is a non-invasive and continuous electroencephalographic assessment of level of sedation which provides a single number ranging from 0 to 100. OAA/S scale is composed of four parameters- responsiveness, speech, facial expression and eyes [3].
In previous studies, correlation between OAA/S and BIS had been done using propofol and midazolam separately during regional anaesthesia. They had compared BIS score at a fixed OAA/S score with variable correlation between the 2 scoring system [4,5]. However, in the present study, BIS score was compared with OAA/S score at different time intervals to find a correlation between BIS and OAA/S score using Dexmedetomidine, Propofol and Midazolam. It would help us to understand the sedative properties of these drugs and will enable us to monitor the sedation level of patient using clinical and EEG based techniques together to avoid oversedation which is quite common using these techniques separately.
The primary objective was to determine any correlation between depth of sedation monitored simultaneously with BIS monitor and OAA/S score in orthopaedic surgeries under spinal anaesthesia. Secondary objectives were to compare the effects of study drugs midazolam, propofol and dexmedetomidine on haemodynamics.
Materials and Methods
This randomised double-blind study was conducted in a medical university from January 2018 to June 2019 after Institutional Ethical Committee Approval (E.C.NO:13/2018). Informed consent was taken from all recruited adult patients of ASA physical status I and II posted for elective lower limb orthopaedic surgeries of approximately 90 minutes duration. Patients with cardiorespiratory disease, pregnant, with psychiatric illness, hypersensitivity to study drugs or were contraindicated for spinal anaesthesia were excluded from the study.
Sample size of 90 was calculated using alpha error of 0.05, power of study to be 80% and considering a difference of 20% regarding the time for onset of sedation to be significant clinically.
All patients were divided randomly into three groups utilising a computerised random number table. Concealment was done by sealed opaque envelope method. The anxiety grade of the patients was noted pre-operatively based on the Amsterdam pre-operative anxiety and information scale [Table/Fig-1] [6]. Patients with a score of 4 were graded as mild, 5-10 as moderate and 11-20 to be severely anxious.
Amsterdam Pre-operative Anxiety and Information Scale (APAIS) [6].
| No. | APAIS Questions | 1 | 2 | 3 | 4 | 5 |
|---|
| 1 | I am worried about the anaesthetic | | | | | |
| 2 | The anaesthetic is on my mind continually | | | | | |
| 3 | I would like to know as much as possible about the anaesthetic | | | | | |
| 4 | I am worried about the procedure | | | | | |
| 5 | The procedure is on my mind continually | | | | | |
| 6 | I would like to know as much as possible about the procedure | | | | | |
1-Not at all, 2-Somewhat, 3-Moderate, 4-Moderately High, 5-Extremely
The BIS reading of 70-80 was found to correlate to a clinical state in which the patient can react to loud verbal, minimal tactile stimulation and a BIS score of 60-70 corresponds to a state in which the patient is sensitive to loud verbal and more extreme tactile stimulation. In OAA/S score of 3 the patient only reacts after the name is called loudly/or frequently [7]. For this reason the OAA/S score 3 was considered as a sedation state on clinical evaluation in the present study, and a BIS score 70 was taken as sedation state during instrumental monitoring. Therefore, the time was noted to hit BIS score 70 and the time to achieve OAA/S score 3. The OAA/S score assessment was performed using a 5-point scale [Table/Fig-2] [7].
Observer’s Assessment of Awareness and Sedation (OAA/S) scale [7].
| Responsiveness | Speech | Facial expression | Eyes | Score |
|---|
| Responds normally to name spoken in normal tone | Normal | Normal | Clear, no ptosis | 5 |
| Lethargic response to name spoken in normal tone | Mild slowing | Mild relaxation | Glazed or mild ptosis | 4 |
| Responds to name being called out loudly | Slurring | Marked relaxation | Glazed and marked ptosis | 3 |
| Responds after mild prodding | Few recognisable words | Marked relaxation | Glazed and marked ptosis | 2 |
| Does not respond after mild prodding | Few recognisable words | Marked relaxation | Glazed and marked ptosis | 1 |
(OAA/S Score is the lowest score in any of the four categories)
All patients were made to fast for 6 hours before the surgery. No patient received any premedication. The monitors (non-invasive blood pressure, electrocardiogram, pulse oximeter) were attached and monitoring started. With proper backup for GA, preloading was done with warm Ringer’s lactate solution 15 mL/kg over 30 minutes. Baseline values of Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), Mean Arterial Pressure (MAP), Heart Rate (HR), Oxygen Saturation (SpO2), were recorded. A thorough skin preparation of forehead was done to remove any skin oils. The sensors of the BIS monitor (BIS LoC 2 channel, ©2011 Covidien, made in Singapore) were placed diagonally on the forehead as follows: one at the centre of forehead approximately 2 inches above the bridge of nose, second directly above the forehead and the third on the temple between the corner of eye and hairline. BIS model was connected to the BIS module and the patient cable. Sensor impedance check was initiated, impedance value was measured and electrode statuses were displayed above each electrode. Baseline values of BIS score and OAA/S score were recorded.
The patients and anaesthesiologist who recorded the data were blinded to the group allocation and study drugs. Study drug preparation and infusion was done by another anaesthetist. Inj midazolam undiluted (concentration of 1 mg/mL) was taken in 20 mL syringe. Inj propofol undiluted (concentration of 10 mg/mL) was taken in 20 mL syringe. Inj dexmedetomidine (2 mL, 200 mcg) diluted with 48 mL of normal saline to get 50 mL of dexmedetomidine in concentration of 4 mcg/mL, 20 mL of this solution was taken. Syringe containing the study drug was attached to a manually controlled infusion pump connected to the IV cannula via infusion line. The syringe and infusion line was wrapped in silver foil to maintain blinding.
The patient received study drug as follows:
Group M (n=30) Inj Midazolam IV loading dose of 0.05 mg/kg over 10 minutes followed by maintenance dose starting at 0.06 mg/kg/hour.
Group P (n=30) Inj Propofol IV loading dose of 1 mg/kg over 10 minutes followed by maintenance dose starting at 1 mg/kg/hour.
Group D (n=30) Inj Dexmedetomidine IV loading dose of 0.5 mcg/kg over 10 minutes followed by maintenance dose starting at 0.5 mcg/kg/hour.
The maintenance dose was titrated after achieving sedation level by increasing or decreasing the infusion at the rate of 0.5 mL/hour (midazolam=0.5 mg/hour, propofol=5 mg/hour, dexmedetomidine=2 mcg/hour) to maintain the BIS score between 65 and 70. Infusion was stopped approximately 5 minutes before the end of surgery.
The patient was positioned in sitting position and under all aseptic precautions, spinal anaesthesia was given with 2.5 mL-3.0 mL 0.5% injection Bupivacaine heavy using 25G Quincke’s spinal needle in L2-L3 or L3-L4 intervertebral space after free and clear flow of cerebrospinal fluid. After positioning the patient supine, monitoring of BIS values was started. Level of block was checked by pin prick method using 23 Gauge hypodermic needle. When sensory block reached T10 level, surgery and study drug was started simultaneously. The time to reach BIS score 70 and OAA/S score 3 from the start of study drug were recorded. The HR, NIBP, SpO2, BIS score and OAA/S score were recorded continuously every 2 minutes from the start of study drug till required level of sedation is achieved and then every 10 minutes till 105 minutes or end of surgery (whichever was earlier), then post-operatively at 15 minutes and 30 minutes.
Adverse events like hypotension (more than 20% decrease in blood pressure from baseline), bradycardia (more than 20% decrease in heart rate from baseline), desaturation (oxygen saturation <94%) were also noted. Bradycardia was treated with injection Atropine 0.6 mg IV. Hypotension was treated with fluid bolus or injection Mephentermine 6 mg IV. Desaturation was treated with oxygen supplementation via facemask at 6 L/minute. The satisfaction of the patient was assessed using a 7 Point Likert verbal rating scale [Table/Fig-3] [8], 12 hours after the surgery by asking the patients to answer the question ‘how you would rate your experience during surgery’? Scores between 5-7 was considered as acceptable.
Patient satisfaction scale [8].
| 1 Extremely dissatisfied |
| 2 Dissatisfied |
| 3 Somewhat dissatisfied |
| 4 Undecided |
| 5 Somewhat satisfied |
| 6 Satisfied |
| 7 Extremely satisfied |
Statistical Analysis
Data were entered in Microsoft Excel and the results presented in frequencies, percentages, Mean±SD. The Chi-square test was used to compare the categorical variables. The One-way analysis of variance (ANOVA) followed by Tukey’s Post-hoc test was used to compare continuous variables among the groups. The p-value less than 0.05 were considered significant. All the analysis was carried out on SPSS 16.0 version (Chicago, Inc., USA).
Results
The groups were comparable in terms of age, gender, anthropometric parameters, duration of surgery, ASA grade and pre-operative anxiety grade of the patients [Table/Fig-4].
Demographic parameters, anxiety grade, ASA grade and duration of surgery: Data expressed as Frequency and Mean±SD.
| Variables | Group-P (n=30) | Group-M (n=30) | Group-D (n=30) | p-value |
|---|
| Age (years) | 36.23±14.89 | 38.50±14.53 | 35.13±12.73 | 0.64 |
| BMI | 21.34±0.98 | 21.72±1.36 | 21.42±1.03 | 0.39 |
| Males (%) | 25 (83.3%) | 21 (70.0%) | 18 (60.0%) | 0.13 |
| Females (%) | 5 (16.7%) | 9 (30.0%) | 12 (40.0%) | 0.13 |
| Anxiety grade mild (%) | 24 (80.0%) | 15 (50.0%) | 25 (83.3%) | 0.06 |
| Anxiety grade moderate (%) | 6 (20.0%) | 10 (33.3%) | 5 (16.7%) | 0.06 |
| Anxiety grade severe (%) | 0 (0.0) | 5 (16.7%) | 0 (0.0) | 0.06 |
| ASA grade I (%) | 21 (70.0%) | 20 (66.7%) | 19 (63.3%) | 0.86 |
| ASA grade II (%) | 9 (30.0%) | 10 (33.3%) | 11 (36.7%) | 0.86 |
| PSS | 6.80±0.40 | 6.73±0.45 | 7.00 | 0.96 |
BMI: Body mass index; ASA: American society of anaesthesiologists; PSS: Patient satisfaction score
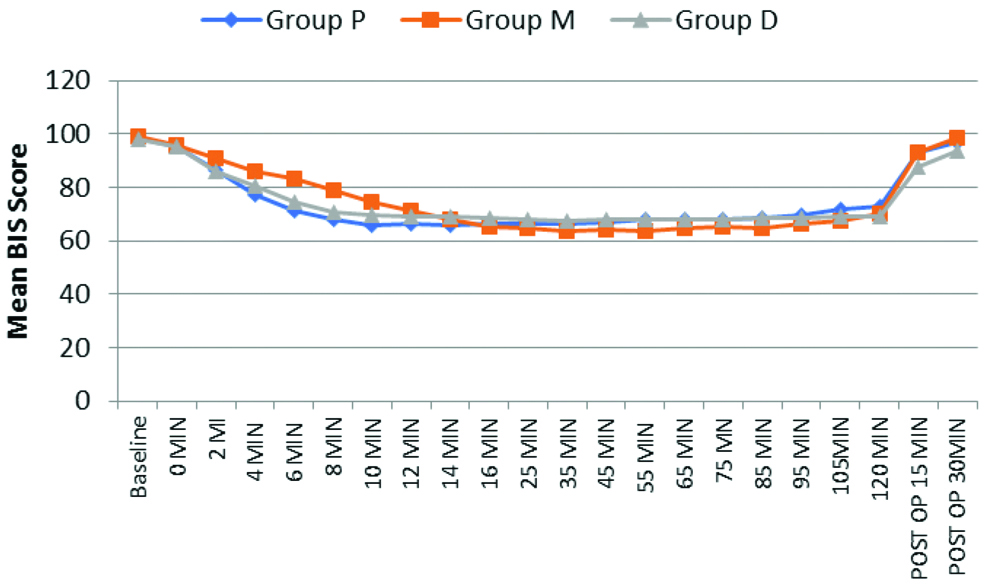
The time to reach BIS score 70 was significantly less in Group P as compared to Group D and Group M (6.00±1.87 minutes v/s 7.97±1.62 minutes and 12.23±1.92 minutes) [Table/Fig-5,6 and 7]. The time to reach OAA/S score 3 was significantly less in Group P as compared to Group M and Group D (6.27±1.92 minutes v/s 12.77±3.19 minutes and 15.20±2.69 minutes). Therefore, the onset of sedation occurred earlier with propofol sedation as compared to midazolam and dexmedetomidine.
Characteristics at onset of sedation.
| Variables | Group P (n=30) | Group M (n=30) | Group D (n=30) | p-value |
|---|
| Time to reach BIS score 70 (mins) | 6.00±1.87 | 12.23±1.92 | 7.97±1.62 | <0.001* |
| Time to reach OAA/S score 3 (mins) | 6.27±1.92 | 12.77±3.19 | 15.20±2.69 | <0.001* |
| OAA/S score at BIS score 70 | 3.33±0.47 | 3.57±0.62 | 4.07±0.36 | <0.001* |
| Correlation coefficient | 0.925 | 0.211 | 0.512 | --- |
| P value of correlation coefficient | 0.022* | 0.133 | 0.163 | |
*significant
Comparison of BIS score among the groups across the time periods.
Comparison of OAA/S score among the groups across the time periods.
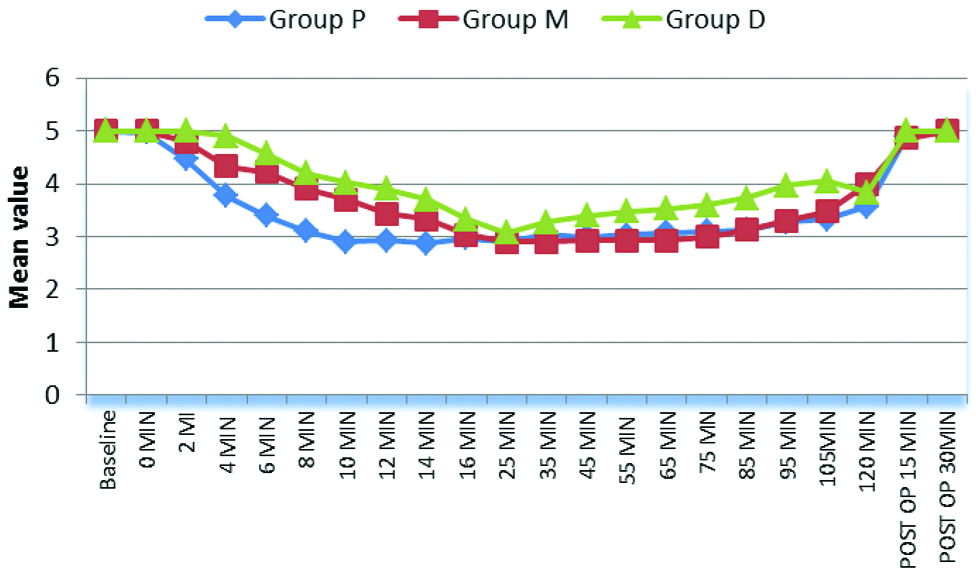
The Spearman’s correlation between time to reach BIS score 70 and OAA/S score 3 in Group P, Group M, Group D were 0.925, 0.211 and 0.512, respectively, which was statistically significant in propofol group but not significant in midazolam and dexmedetomidine group [Table/Fig-5]. This shows correlation between BIS index and OAA/S scale during onset of sedation in Group P but divergence between BIS index and OAA/S scale during onset of sedation in Group M and Group D.
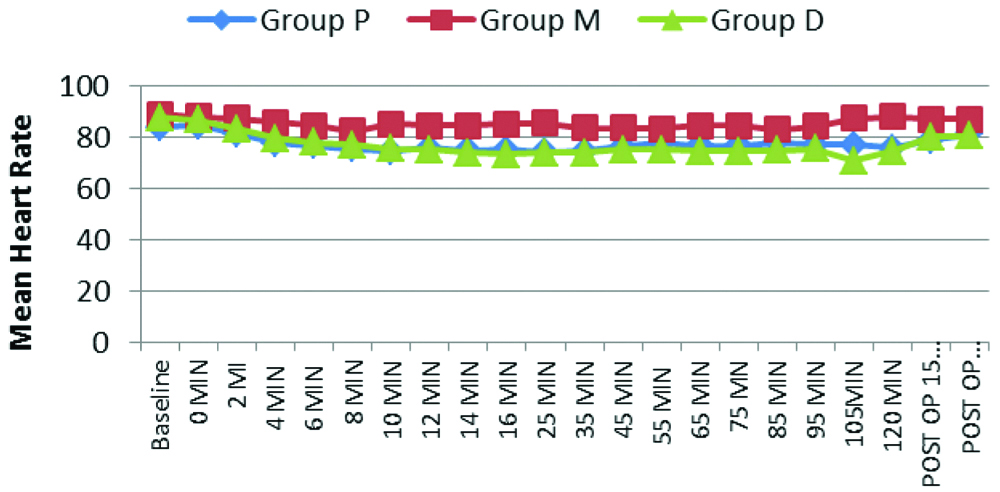
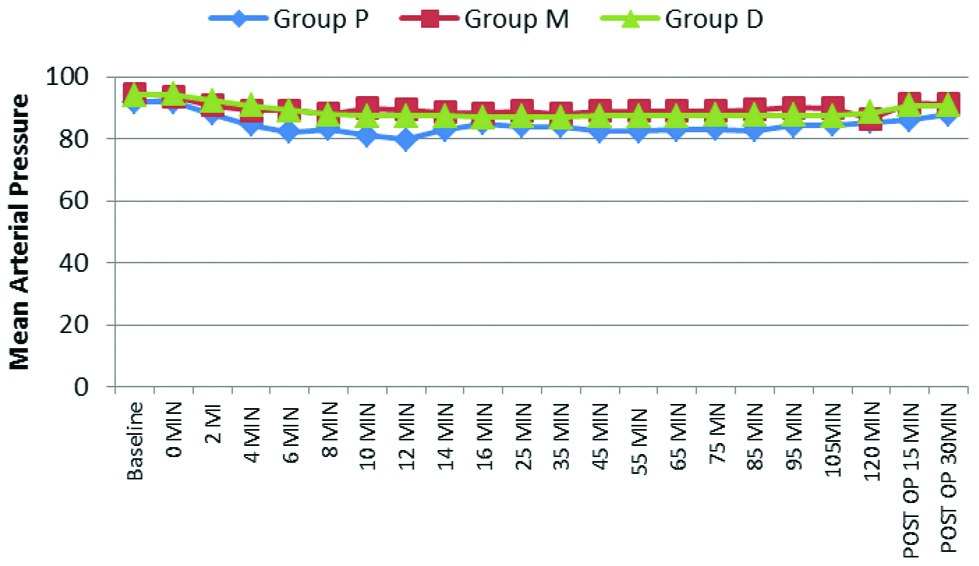
The intra-operative parameters like HR, MAP and SpO2 were recorded and compared at various time intervals. HR decreased in all three groups from baseline value after start of the study drug and it did not return to baseline value at any time period [Table/Fig-8]. MAP began to fall in all groups after start of study drug. After the loading dose was given i.e., after 10 minutes, MAP in Group P, Group M and Group D were 81.23±5.116 mmHg, 90.00±7.15 mmHg and 87.53±5.90 mmHg, respectively, which shows significant decrease in all three groups (p≤0.001,0.008, ≤0.001) [Table/Fig-9]. The oxygen saturation was comparable in all groups.
Comparison of HR (bpm) among the groups.
Comparison of MAP (mmHg) among the groups across the time periods.
The incidence of complications as shown in [Table/Fig-10], Hypotension occurred in 10 patients in Group P (33.3%) and 4 patients in Group M (13.3%). Bradycardia occurred in 7 patients in Group D (23.3%) and 2 patients in Group P (6.7%). Hypotension was significantly more in Group P (p=0.001) and bradycardia was significantly more common in Group M (p=0.001). Mean PSS after surgery in Group P, Group M and Group D were 6.80±0.40, 6.73±0.45 and 7.00. PSS was acceptable in all the groups but maximum satisfaction was noted in Group D [Table/Fig-4].
Comparison of complications among the groups.
| Complications | Group P (n=30) | Group M (n=30) | Group D (n=30) | p-value1 |
|---|
| No. | % | No. | % | No. | % |
|---|
| Hypotension | 10 | 33.3 | 4 | 13.3 | 0 | 0.0 | 0.001* |
| Bradycardia | 2 | 6.7 | 0 | 0.0 | 7 | 23.3 |
| None | 18 | 60.0 | 26 | 86.7 | 23 | 76.7 |
1Chi-square test, *Significant
Discussion
Time of onset of sedation was compared for propofol, midazolam and dexmedetomidine using both BIS index and OAA/S scale. With propofol sedation, time to reach BIS score 70 and OAA/S score 3 were similar. Correlation coefficient also showed a strong correlation in group P. Thus, instrumental monitoring and clinical observation during the onset of sedation using propofol is comparable (r=0.925, p-value 0.022). This was not the case with dexmedetomidine and midazolam This study demonstrated divergence between time to reach BIS score 70 and time to achieve OAA/S score 3 during onset of sedation with dexmedetomidine (r=0.512, p-value=0.163) and midazolam (r=0.21, p-value=0.133). Thus, instrumental monitoring and clinical observation were not comparable during the onset of sedation with midazolam and dexmedetomidine in this study.
Similar results were found between BIS and OAA/S scale for propofol in the previous studies [9-12]. There are possibilities that propofol being a hypnotic, suppressed cerebral activity faster and more predictively [13,14]. A longer time to suppress the cerebral activity might cause a delayed decrease in BIS scores in patients sedated with midazolam and dexmedetomidine despite the patient being clinically asleep which resulted in a great divergence between the time to reach BIS score 70 and time to achieve OAA/S score 3 in these patients, although much explanation remains to be sought for. From these findings, it is manifest that BIS score during the onset of sedation using midazolam and dexmedetomidine may not correlate with OAA/S scores.
Onset of sedation was faster using propofol as compared to dexmedetomidine and midazolam. Similar results were obtained by Khurana P et al., who found that mean time for propofol and midazolam was 6.2±0.2 minutes and 11.0±0.5 minutes, Bagchi D et al., found 4.8±3.3 minutes v/s 14.9±9.9 minutes, Bhosale J et al., who got 9.80±2.78 minutes v/s 19.30±3.16 minutes and Shah PJ et al., found that propofol had faster onset time as compared to dexmedetomidine (15.57±1.89 minutes vs. 27.06±2.26 minutes) [5,12,15,16]. These values are higher than the values obtained in present study as they used subanaesthetic doses of sedatives. Yaddanapudi S et al., found faster onset with propofol than with midazolam (13.0±4.2 minutes v/s 18.8±4.2 minutes, p<0.0001) [2]. The onset of sedation was longer as compared to the present study as they performed the study in geriatric age group patients in whom lower dose of sedative agents are required.
The haemodynamic parameters were found to be more stable in midazolam group. HR was significantly lower with dexmedetomidine which could be due to its sympatholytic properties. MAP was lower using propofol which could be attributed to direct inhibitory effect on sympathetic outflow causing vasodilatation. Similarly, Khurana P et al., found that MAP was lower than baseline value throughout the study for propofol (from 83.1±8.5 mmHg to 68.25±2.98 mmHg) and midazolam (from 81.7±6.8 mmHg to 76.8±6.9 mmHg) [5]. Shah PJ et al., compared propofol and dexmedetomidine, MAP was lower with propofol sedation (62.43±7.04 mmHg v/s 76.65±7.13 mmHg, p=0.002) and mean HR was significantly lower in dexmedetomidine (68.34±5.64 bpm v/s 82.83±7.55 bpm, p=0.002) [16]. Lim TW et al., concluded that BIS values differed at the same level of sedation between different sedative agents, therefore it should not be used alone for the assessment of sedation levels during spinal anaesthesia [17].
In present study, Bradycardia was more common in dexmedetomidine group (33.3%) and hypotension was more in propofol group (33.3%) and midazolam group (13.3%). Jo YY et al., found more hypotension with midazolam (n=38, 66%) and bradycardia more with dexmedetomidine (n=29, 50%) [11]. Yaddanapudi S et al., also found significantly more hypotension with propofol than midazolam {16 (50%) v/s 4 (14.3%), p=0.003} [2]. Patient satisfaction was more with dexmedetomidine in this study. Lim YP et al., Shah PJ et al., and Nirmala BC et al., found that the satisfaction level was significantly higher with dexmedetomidine sedation [11,16,18]. The patients were more cooperative and arousable with dexmedetomidine.
Limitation(s)
Due to narrow time intervals taken in the study, OAA/S score had to be accessed frequently which causes frequent patient stimulation leading to alteration in the actual level of sedation. Placebo controlled study design was not followed in this study. More detailed study is needed to guide the effectiveness of BIS monitoring in continuous sedation during spinal anaesthesia using different sedative agents at variable levels of sedation.
Conclusion(s)
Significant correlation was found between BIS index and OAA/S scale during onset of sedation using propofol but not with dexmedetomidine and midazolam. All three drugs were found to be good sedative agents. Time to reach sedation was less with propofol than midazolam and dexmedetomidine. Propofol had the fastest onset of sedation and clear headedness. Dexmedetomidine and propofol decreased heart rate and blood pressure. Patients sedated with dexmedetomidine were more calm, cooperative and arousable. Patient satisfaction was maximum using dexmedetomidine.
1-Not at all, 2-Somewhat, 3-Moderate, 4-Moderately High, 5-Extremely
(OAA/S Score is the lowest score in any of the four categories)
BMI: Body mass index; ASA: American society of anaesthesiologists; PSS: Patient satisfaction score
*significant
1Chi-square test, *Significant