General anaesthesia, consisting of four states i.e., unconsciousness, amnesia, analgesia, immobility is a drug induced reversible condition. It also consists of stability of the physiological systems, including the autonomic, cardiovascular, respiratory and thermoregulatory systems [1]. Induction is a very crucial phase of general anaesthesia [2]. As endotracheal intubation is a strong adrenergic stimulus, hypnotics are commonly administered to make wakeful patients unresponsive [3].
Haemodynamic response to laryngoscopy and intubation was first described by Reid and Brace in 1940 [4]. The magnitude of response is said to be directly proportional to the force and duration of laryngoscopy [5]. There is transient and unpredictable increase in heart rate and blood pressure which can have serious consequences especially in high risk patients like those of heart disease and hypertension. So attenuation of these responses is recommended as a precaution against perioperative morbidity and mortality [6].
Many non-pharmacological and pharmacological methods have been tried to attenuate these haemodynamic responses to intubation. Some of them are gentle handling and shorter laryngoscopy, use of LMA as an alternate and blocking of superior laryngeal and glossopharyngeal nerves. Inhalational and topical anaesthetics, calcium channel blockers, ACE inhibitors, Beta blockers and vasodilators are the various pharmacological options [4].
All these approaches or agents have failed to prove themselves as ideal. Hence, we are still searching for an ideal agent to attenuate this haemodynamic response.
Dexmedetomidine (Dextro isomer of medetomidine) which was first introduced in 1999 acts on the alpha-2 receptors in the post synaptic terminals in CNS and causes increased vagal activity leading to attenuation of haemodynamic responses. It also causes sedation, analgesia and anxiolysis [7]. Fentanyl citrate which is a narcotic analgesic acts mainly on opoid mu receptors leading to analgesia and sedation [8].
Dexmedetomidine and Fentanyl have stood the test of time in attenuating the haemodynamic responses during laryngoscopy and intubation without having much undesirable effects [7,9]. So, the present study was aimed to compare the extent of attenuation of the haemodynamic response to laryngoscopy and intubation in adult patients posted for elective surgeries under general anaesthesia using either single I.V. bolus of dexmedetomidine or fentanyl given over 10 minutes before induction of anaesthesia.
The primary aim was to study the effects of dexmedetomidine and fentanyl on haemodynamic response to laryngoscopy and endotracheal intubation. The secondary aim was to study the effect of dexmedetomidine and fentanyl:
Materials and Methods
The present open randomised controlled trial was conducted in March to May 2019, after approval from the college ethical committee of GMC Patiala. Patient consent was taken before conduct of anaesthesia in each case.
Sample Size Calculation
Assuming a 5% two-tailed significance level (a=0.05) and power of 80% (b=0.20), to detect 7.05% absolute difference in the incidence of heart rate, a sample size of 96 patients were required for the study. So, 100 patients of either sex were included in this study. The patients were divided randomly into 2 groups Group D (Dexmedetomidine) and Group F (Fentanyl), consisting of 50 patients each, allotted by simple randomisation which was done using chit method.
Inclusion Criteria:
Age 20-60 years,
ASA grade I and II
Elective surgical procedure under general anaesthesia,
Mallampati grade 1 and 2,
Patient willing to participate in this study.
Exclusion Criteria:
Patient refusal,
History of bradycardia (Heart Rate <50 bpm),
History of renal or liver dysfunction,
History of previous cerebrovascular accident,
History of coronary artery disease,
Pregnant and lactating patients.
A thorough pre-anaesthetic check-up and routine blood investigations were done before surgery in all the patients. Each patient was kept Nil per oral for at least six hours pre-operative and received tablet clonazepam 0.5 mg at 6 am on the day of surgery.
The routine check-up of anaesthesia machine, circuit and resuscitation equipments was done before shifting the fasting patients into the operation theatre. Patients were monitored by a multichannel monitor. Two IV lines using 18G cannula were secured & 500 mL ringer lactate over 30 minutes was given to all patients. After settling in OT for 5minutes, Basal Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), Mean Arterial Pressure (MAP), Heart Rate (HR), and SpO2 were recorded (T0). The vital parameters and ECG were continuously monitored and recorded.
Pre induction included intravenous Inj. Glycopyrrolate 0.2 mg, inj. Ondansetron 4 mg and inj. Ranitidine 50 mg. Also, 100% oxygen was given to all patients.
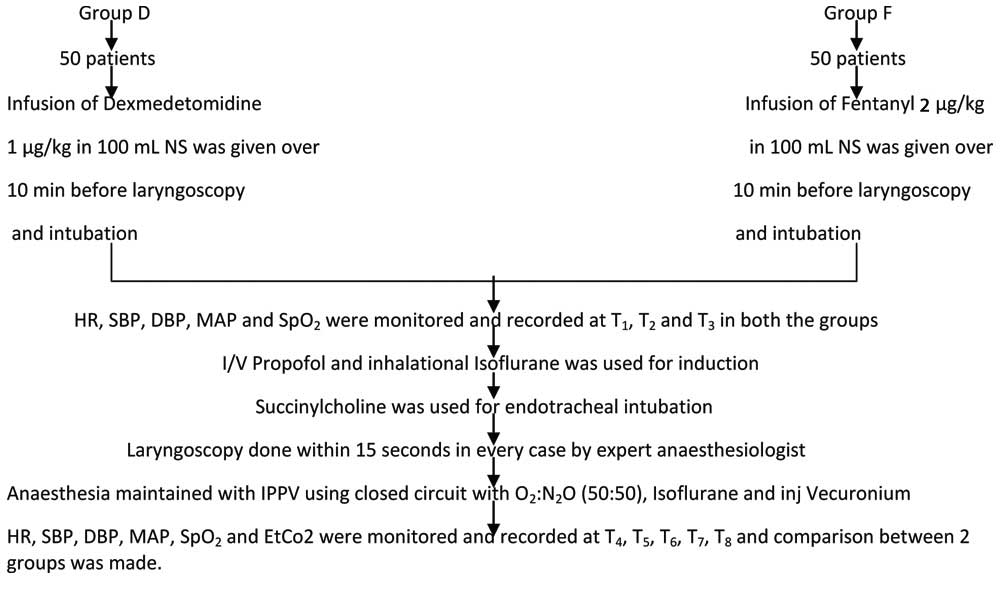
Group D patients were given inj. Dexmedetomidine 1 μg/kg in 100 mL N.S. intravenous infusion over 10 minutes prior to laryngoscopy and endotracheal intubation. Group F received fentanyl 2 μg/kg in 100 mL N.S. intravenous infusion over 10 minutes before laryngoscopy. HR, SBP, DBP, MAP, SpO2 were monitored continuously from the entry of the patient in the operation theatre till shifting to the ward and later on but documented at T1 (the start of infusion), at T2 (5 minutes of start of infusion) and at T3 (10 minutes of start of infusion i.e., completion of infusion) in both the groups.
Intravenous Propofol and inhalational isoflurane were used for induction. Loss of eyelash and corneal reflex determined the propofol dose. Succinylcholine was the muscle relaxant used for endotracheal intubation. Disposable, oral cuffed endotracheal tube of adequate size was used. Laryngoscopy was done within 15 seconds in every case by an expert anaesthesiologist.
Anaesthesia was maintained with IPPV using O2, N2O, and inhalational anaesthetic like Isoflurane. Muscle relaxant Inj. Vecuronium bromide 0.08 mg/kg to 0.1 mg/kg was given as intravenous bolus according to requirement and maintained as per need. Vital parameters were monitored continuously and recorded at the time of laryngoscopy and intubation (T4) and after laryngoscopy and intubation at 1, 3, 5, 10 minutes (T5 to T8) [Table/Fig-1].
Flow chart depicting the methodology.
Neostigmine 50 μg/kg and glycopyrrolate 10 μg/kg intravenously were used to reverse neuromuscular blockage after surgery. Extubation was done after satisfying extubation criteria and patient was shifted to Post Anaesthesia Care Unit (PACU).
In post anaesthesia care unit, vital monitoring or any untoward event was monitored for atleast 90 minutes after surgery every 10 minutes. When modified Aldrete score >9, patient was shifted to ward.
Fall in BP 20% below baseline and pulse rate <50 beats per minute (bpm) was considered as hypotension and bradycardia respectively and was treated appropriately. Decreased saturation, rise or fall of EtCO2 was managed according to cause.
After completion of drug infusion, sedation scoring was done as per RAMSAY sedation scale. Adverse effects like hypotension, bradycardia, arrhythmia if present were treated and recorded.
Statistical Analysis
The relevant data on each patient was entered into the proforma and also presented in the master chart. Descriptive statistics was done for all data and suitable statistical tests of comparison were done. Continuous variables were analysed with unpaired t-test and Mann Whitney U test. Categorical variables were analysed with the Chi-square test. Statistical significance was taken as p<0.05, Statisticaly highly significant was taken as p<0.001, Statistical non significance was taken as p>0.05. The observations were depicted in tables. The data was analysed using SPSS (22.00 version) software and Microsoft Excel 2007.
Results
Both groups were comparable and there was no statistically significant difference with regard to age (p=0.9973), sex (p=0.6484), ASA grade (p=0.8414), body weight (p=0.7269) and duration of surgery (p=0.9355).
[Table/Fig-2] shows that the mean heart rate in both the groups was maximum at T4 but it was remarkably increased (p=0.0465) in Group F showing less attenuation of heart rate by fentanyl compared to dexmedetomidine. [Table/Fig-3] shows that the mean systolic blood pressure decreased initially in both the groups at T3 but this difference was non-significant. However, there was rise in systolic blood pressure in both the groups at T4. This rise was significantly lesser in group D (p=0.0187).
Comparison of heart rate at different time intervals in patients of Group D and Group F.
| HR (bpm) | Group D | Group F | p-value |
|---|
| Mean | SD | Mean | SD |
|---|
| T0 | 85.67 | 11.676 | 81.73 | 10.125 | 0.1972 |
| T1 | 86.94 | 12.156 | 83.34 | 9.754 | 0.2538 |
| T2 | 86.22 | 11.274 | 84.48 | 9.133 | 0.5516 |
| T3 | 84.90 | 10.556 | 83.22 | 11.546 | 0.2453 |
| T4 | 93.12 | 9.501 | 98.04 | 8.256 | 0.0465* |
| T5 | 89.27 | 8.781 | 94.01 | 7.548 | 0.0462* |
| T6 | 85.72 | 8.121 | 86.78 | 7.253 | 0.6286 |
| T7 | 84.78 | 7.285 | 84.68 | 7.268 | 0.9614 |
| T8 | 83.45 | 10.325 | 83.07 | 6.774 | 0.8784 |
SD: Standard deviation; * Statistically significant
Comparison of SBP (mmHg) at different time intervals in patients of Group D and Group F.
| SBP (mmHg) | Group D | Group F | p-value |
|---|
| Mean | SD | Mean | SD |
|---|
| T0 | 123.01 | 8.587 | 124.73 | 8.247 | 0.4736 |
| T1 | 125.86 | 9.498 | 128.02 | 9.254 | 0.4194 |
| T2 | 120.07 | 9.877 | 123.55 | 9.745 | 0.2159 |
| T3 | 116.61 | 10.476 | 120.25 | 9.547 | 0.2053 |
| T4 | 133.81 | 9.055 | 139.77 | 8.245 | 0.0187* |
| T5 | 123.95 | 9.245 | 130.03 | 8.547 | 0.0108* |
| T6 | 121.62 | 7.687 | 127.56 | 7.658 | 0.9969 |
| T7 | 121.33 | 6.478 | 124.97 | 6.197 | 0.1474 |
| T8 | 119.91 | 6.542 | 123.03 | 7.475 | 0.0565 |
SD: Standard deviation; * Statistically significant
[Table/Fig-4] shows that the Diastolic blood pressure rose at T4 and was significantly better attenuated by dexmedetomidine as compared to fentanyl (p=0.0227). [Table/Fig-5] shows that the mean arterial pressure was also managed significantly better by dexmedetomidine at T4 (p=0.0092) and at T5 (p=0.0206).
Comparison of DBP (mmHg) at different time intervals in Patients of Group D and Group F.
| DBP (mmHg) | Group D | Group F | p-value |
|---|
| Mean | SD | Mean | SD |
|---|
| T0 | 84.73 | 6.784 | 84.69 | 6.258 | 0.9828 |
| T1 | 81.87 | 6.659 | 83.75 | 6.365 | 0.3126 |
| T2 | 80.22 | 7.476 | 80.64 | 6.647 | 0.8346 |
| T3 | 79.99 | 6.890 | 81.67 | 7.679 | 0.4196 |
| T4 | 92.73 | 6.679 | 97.01 | 6.167 | 0.0227* |
| T5 | 85.57 | 7.947 | 90.29 | 6.679 | 0.0275* |
| T6 | 80.47 | 6.359 | 84.49 | 9.573 | 0.0867 |
| T7 | 82.67 | 7.576 | 84.63 | 6.467 | 0.3301 |
| T8 | 80.39 | 6.642 | 82.97 | 8.426 | 0.2351 |
SD: Standard deviation; * Statistically significant
Comparison of MAP (mmHg) at different time intervals in Patients of Group D and Group F.
| MAP (mmHg) | Group D | Group F | p-value |
|---|
| Mean | SD | Mean | SD |
|---|
| T0 | 96.82 | 7.429 | 97.37 | 7.190 | 0.7914 |
| T1 | 97.87 | 8.249 | 99.84 | 7.246 | 0.3741 |
| T2 | 95.43 | 7.536 | 97.54 | 9.768 | 0.3967 |
| T3 | 90.84 | 7.297 | 93.51 | 7.465 | 0.2071 |
| T4 | 107.40 | 6.167 | 112.24 | 6.435 | 0.0092* |
| T5 | 99.10 | 7.142 | 104.18 | 7.845 | 0.0206* |
| T6 | 94.21 | 6.435 | 98.85 | 9.684 | 0.0517 |
| T7 | 96.54 | 7.570 | 99.74 | 6.784 | 0.1221 |
| T8 | 95.57 | 6.674 | 98.33 | 5.974 | 0.1300 |
SD: Standard deviation; * Statistically significant
[Table/Fig-6] shows that no statistically significant difference (p-values >0.05) was found in SpO2 between two groups and both groups were comparable at T0-T8.
Comparison of SpO2 at different time intervals in patients of Group D and Group F. saturation was mainted
| SpO2 | Group D | Group F | p-value |
|---|
| Mean | SD | Mean | SD |
|---|
| T0 | 100.00 | 0.000 | 100.00 | 0.000 | - |
| T1 | 99.97 | 0.314 | 100.00 | 0.000 | 0.5009 |
| T2 | 99.95 | 0.240 | 99.97 | 0.283 | 0.7039 |
| T3 | 99.89 | 0.452 | 99.97 | 0.198 | 0.2544 |
| T4 | 99.95 | 0.240 | 99.96 | 0.240 | 0.0988 |
| T5 | 99.98 | 0.283 | 100.00 | 0.000 | 0.6184 |
| T6 | 99.97 | 0.314 | 100.00 | 0.000 | 0.5009 |
| T7 | 100.00 | 0.000 | 100.00 | 0.000 | - |
| T8 | 100.00 | 0.000 | 100.00 | 0.000 | - |
SD: Standard deviation; All the patients were under controlled ventilation and high level oxygen saturation was maintained.
[Table/Fig-7] shows that no statistically significant difference (p-values >0.05) was found in EtCO2 between two groups and both groups were comparable at T0-T8.
Comparison of EtCO2 at different time intervals in patients of Group D and Group F.
| EtCO2 | Group D | Group F | p-value |
|---|
| Mean | SD | Mean | SD |
|---|
| T0 | 36.07 | 1.007 | 36.03 | 0.856 | 0.8310 |
| T1 | 36.14 | 1.087 | 36.18 | 1.027 | 0.8504 |
| T2 | 36.13 | 0.895 | 36.23 | 0.887 | 0.5760 |
| T3 | 36.14 | 1.374 | 35.87 | 1.017 | 0.2668 |
| T4 | 36.23 | 1.468 | 36.20 | 1.061 | 0.9070 |
| T5 | 36.45 | 1.430 | 36.39 | 1.241 | 0.8232 |
| T6 | 36.61 | 1.524 | 36.30 | 1.371 | 0.2876 |
| T7 | 36.41 | 1.481 | 36.29 | 1.200 | 0.6572 |
| T8 | 36.30 | 1.522 | 36.25 | 1.285 | 0.8595 |
SD: Standard deviation
The difference in mean dosage of propofol during induction was non-significant in both the groups (p=0.1580). Also the Ramsay Sedation scale score (p=0.5499) and Modified Aldrete score was comparable in both the groups.
Discussion
This study was done to know which of these two drugs i.e that dexmedetomidine and fentanyl in achieving haemodynamic stability during intubation.
Heart Rate
There was increase in heart rate at T4 and T5 in both the groups. However, the magnitude of increase in heart rate at T4 and T5 was higher in Group F as compared to Group D (p-value <0.05) showing dexmedetomidine is better in attenuating heart rate than fentanyl.
This is in concordance to literature as similar observations were made by Patel CR et al., in their study [10]. However, the findings are somewhat in contrast with the results of Kharwar RK et al., and Jain V et al., who observed that heart rate was decreased from baseline after laryngoscopy and intubation in both groups, but the decrease was more in Dexmedetomidine group as compared to fentanyl group [11,12].
Systolic Blood Pressure (SBP)
The difference between mean systolic blood pressure at T0, T1, T2, T3 was statistically insignificant (p >0.05). However, this study demonstrated that the mean SBP rose in both groups at T4 and T5. But it’s rise was statistically more in Group F than Group D (p-value <0.05). This shows that dexmedetomidine is more efficacious in controlling systolic blood pressure during intubation as compared to fentanyl.
In the study conducted by Patel CR et al., it was observed that Dexmedetomidine significantly attenuated stress response at intubation compared with fentanyl [10]. This is similar to our study. Jain V et al., also observed that Dexmedetomidine produced more significant attenuation of increase in SBP during laryngoscopy and intubation as compared with fentanyl, which is in concordance with our study [12].
Diastolic Blood Pressure (DBP)
The difference between mean diastolic blood pressure at T0, T1, T2, T3 in the two groups was statistically insignificant (p-values >0.05). The mean diastolic blood pressure at T4 in Group D was 92.73±6.679 mmHg and it was 97.01±6.167 mmHg in Group F. Significant difference was found in the mean diastolic blood pressure between two groups at T4 (p-value=0.0227). The mean diastolic blood pressure at T5 in Group D was 85.57±7.947 mmHg and was 90.29±6.679 mmHg in Group F. This difference was significant (p-value=0.0275). The difference between mean diastolic blood pressure at T6, T7, T8 in both groups was statistically insignificant (p-values >0.05).
The results are in concordance with that of Jain V et al., who observed a significant increase in DBP during laryngoscopy and intubation with fentanyl group as compared to Dexmedetomidine group [12].
Mean Arterial Blood Pressure (MAP)
No statistically significant difference (p-values >0.05) was found in mean arterial pressure between two groups and both groups were comparable at T0, T1, T2, T3. The mean arterial blood pressure at T4 in Group D was 107.40±6.167 mmHg and it was 112.24±6.435 mmHg in Group F which was statistically significant (p-value=0.0092). The mean value of mean arterial blood pressure at T5 in Group D was 99.10±7.142 mmHg and was 104.18±7.845 mmHg in Group F (p-value=0.0206). The mean arterial blood pressure was insignificant in both the groups at T6, T7, T8. These results are in concordance with that of earlier literature [13].
Dose of Anaesthetic Agent
In this study, the mean dose of propofol used for induction in Group D was 103.10±15.79 mg and in Group F was 108.70±11.48 mg. This difference in dose was statistically insignificant in both the groups (p-value=0.1580) nullifying any contributory role of propofol in attenuating haemodynamic responses.
Adverse Effects
No patient in this study had bradycardia (HR <50 bpm), hypotension (SBP <90 mmHg or DBP <60 mmHg or MAP <50 mmHg) or arrhythmias. Vitals were also stable in Post-operative Anaesthesia Care Unit (PACU).
Limitation(s)
Cost of drug is an important factor and in this RCT, cost effectiveness analysis was not conducted. Levels of drug in blood were not measured. Bispectral Index (BIS) was not used to measure depth of anaesthesia. Neuromuscular monitoring was not used in this RCT.
Conclusion(s)
Dexmedetomidine significantly decreased the sympathetic response of laryngoscopy and intubation as compared to Fentanyl, so Dexmdetomidine is superior to Fentanyl in attenuation of haemodynamic response during laryngoscopy and intubtion. On the basis of this study, an intravenous bolus dose of dexmedetomidine 1 μg/kg in 100 mL N.S. is recommended to be administered over 10 minutes before laryngoscopy and intubation especially in high risk patients.
SD: Standard deviation; * Statistically significant
SD: Standard deviation; * Statistically significant
SD: Standard deviation; * Statistically significant
SD: Standard deviation; * Statistically significant
SD: Standard deviation; All the patients were under controlled ventilation and high level oxygen saturation was maintained.
SD: Standard deviation