Synovial Fluid Eosinophilia (SFE) is a rare finding. Minor SFE is defined as <10% eosinophils of the total leucocyte count in Synovial Fluid (SF), and major SFE as >10% eosinophils of the total leucocyte count in SF. The aetiology and pathophysiology of eosinophilic synovitis is unclear. Most commonly affected joints are Knees; however ankle, elbow and metatarso-phalangeal joint involvement is also being reported. A 10-year-old girl reported with history of pain, swelling and difficulty in bending left knee since five days. On the basis of investigations such as blood investigations including complete blood count, Rheumatoid factor, filarial card test etc., radiographs of knee and arthrocentesis of knee, she was diagnosed as Eosinophilic Synovitis of Knee with peripheral eosinophilia without any known cause. She was treated with Ibuprofen 200 mg BD for 10 days and was relieved of her complaints. After one and half year of follow-up, there were no episodes of recurrent pain or swelling and patient was doing well.
Case Report
A 10-year-old girl reported with history of pain, swelling and difficulty in bending left knee since five days. Pain was dull aching in character, mild in intensity, increases with flexion and walking and was relieved by rest and medication. There was no history of trauma, fever, cough, abdominal pain, diarrhea, headache, watering from eyes or burning micturition. There was no history of treatment for any allergic conditions, drug allergy or skin lesion. No other joints were involved and there was no significant family history.
On local examination, patient had knee swelling without any erythema. Local temperature was slightly raised, there was no tenderness on palpation, range of motion was 0°-110° which was painful and distal neuro-vascular examination was normal. There was no evidence of inguinal and popliteal lymphadenopathy and systemic examination was unremarkable. On the basis of history and clinical examination, differential diagnosis of reactive synovitis, juvenile arthritis, low grade septic arthritis and effusion due to blood dyscrasia was made.
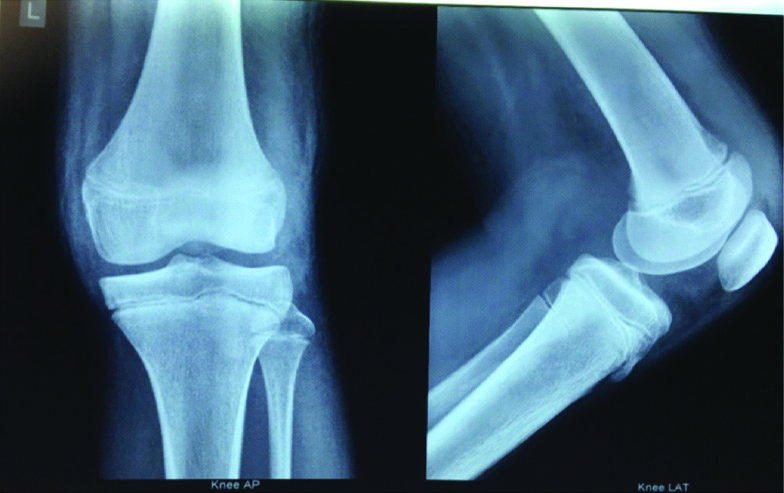
Patient was investigated for further management in the form of blood investigation which included Complete Blood Count (CBC) with peripheral smear, Erythrocyte Sedimentation Rate (ESR), C Reactive Protein (CRP), Rheumatoid factor, Anti-nuclear antibody (ANA), Filaria card test (antigen) and serum Immunoglobulin E (IgE). Blood investigations revealed peripheral eosinophilia of 29% [Table/Fig-1]. Stool examination was performed for ova and cyst and was found to be negative. Radiograph of left knee showed effusion [Table/Fig-2]. Arthrocentesis of left knee was performed under aseptic conditions and approximately 20 mL of synovial fluid was aspirated which was examined for gross appearance, routine microscopy, biochemical and microbiological (Gram staining and Acid Fast Bacilli staining, culture and sensitivity) analysis [Table/Fig-3].
| Test | Results |
|---|
| Complete blood count | Haemoglobin: 12.9 g%Total leukocyte count: 11320 cells/mm3Neutrophils: 43%Lymphocytes: 26%Monocytes: 2%Eosinophils: 29%Platelets: 368000/mm3 |
| Peripheral smear | Normocytic normochromic with eosinophilia. No blood parasites seen. |
| Erythrocyte sedimentation rate | 10 mm in 1st hr. |
| C-reactive protein | 0.6 mg/dL |
| Rheumatoid factor | Negative |
| Mantoux test | Negative |
| Filarial card test (antigen) | Negative |
| Serum IgE | 89 (normal <150 KIU/L) |
| Anti-nuclear antibody | Negative |
Anterioposterior and lateral view radiograph of the left knee suggestive of effusion of knee showing no bony abnormality.
| Test | Result |
|---|
| Physical analysis | Amount: 20 mLColour: StrawTurbidity: PresentCoagulum: Not presentSpecific gravity: 1.005pH: 7:0 |
| Chemical analysis | Sugar: 70 mg/dLProtein: 4.30 gm/dL |
| Microscopic finding | Total leucocyte count: 1790 cells/cummPolymorphs: 06%Lymphocytes: 15%Eosinophils: 79%No red blood cellsGram staining: NegativeAFB staining: NegativeOthers: Nil |
| Culture and sensitivity | No growth |
AFB: Acid fast bacilli
On the basis of investigations, she was diagnosed as Eosinophilic Synovitis of Knee with peripheral eosinophilia without any known cause. She was treated with Ibuprofen 200 mg BD for 10 days and was relieved of her complaints. After one and half year of follow-up, there were no episodes of recurrent pain or swelling and patient was doing well.
Discussion
The SFE is a rare finding. There is no consensus regarding the definition of SFE. Some authors consider SFE as the presence of eosinophils in SF at any extent [1,2]. While some authors consider those SFs with differential count of >2% eosinophils and others with the eosinophils count at a percentage >10% [3,4]. Few authors have described the difference between minor and major SFE [2,4,5], and they have considered only major SFEs to have clinical relevance. Minor SFE was defined as <10% eosinophils of the total leucocyte count in SF, and major SFE as >10% eosinophils of the total leucocyte count in SF. In present case, eosinophils in SF were 79% of the total leucocyte count which defines this case as major SFE. Most commonly affected joints are Knees, however ankle, elbow and metatarso-phalangeal joint involvement is also being reported [4,6,7]. The patient sub-group of eosinophilic synovitis is generally children or young adults and is predominantly females as in present case also [5]. The synovitis usually presents with a large component of joint effusion but with few inflammatory signs and resolves rapidly on treatment with Non Steroidal Anti Inflammatory Drugs (NSAIDs) [2,4,5,8,9].
A literature search was performed on Pubmed using words ‘synovial fluid Eosinophilia’ and ‘peripheral eosinophilia’, ‘eosinophilic synovitis knee’. Bibliographical references of relevant retrieved articles were also checked. The search yielded a total of 13 papers in English language and 1 paper in French language from 1975 to 2015 which included 9 case reports and 5 case series and a total of 54 patients of eosinophilic synovitis [2-15]. Clinical characteristics as well as haematological and synovial fluid parameters of patients presented with eosinophilic synovitis presented till now have been summarised in [Table/Fig-4,5]. Out of 54 patients, four patients had minor SFE and 50 patients presented with major SFE. About 18 patients were reported as having Idiopathic eosinophilic synovitis.
Clinical characteristics of patients with Eosinophilic Synovitis [2-15].
| Sl. No. | Study | Year | Joint involved | No. of patients | Treatment | Associated clinical condition | Diagnosis |
|---|
| 1 | Present case | 2020 | Knee | 01 | NSAID’S | None | Idiopathic |
| 2 | Muralidharagopalan NR et al., [11] | 2015 | Knee | 01 | Diethylcarbamazine for three weeks | None | Idiopathic |
| 3 | Vazquez Trinanes C et al., [8] | 2013 | | 10 | | | |
| Minor SFE | | Knee | 01 | No treatment | TKA for OA | NA |
| Ankle | 01 | No treatment | Asthma | Allergic |
| Knee | 01 | No treatment | Trauma | Traumatic |
| Major SFE | | Knee | 01 | NA | None | Septic |
| Knee | 01 | NA | None | Septic |
| Wrist | 01 | NA | None | Pseudogout |
| Knee | 01 | NA | None | Pseudogout |
| Knee | 01 | NA | None | Psoriatic Arthritis |
| Knee | 01 | NA | None | Pharmacological Eosinophilia |
| Knee | 01 | NA | None | Idiopathic |
| 4 | Atanes A et al., [5] | 1996 | Knee | 01 | NSAIDS | None | Idiopathic |
| 5 | Tauro B [9] | 1995 | Knee | 12 | Diethylcarbamazine for three weeks | None | Idiopathic |
| 6 | Padeh S et al., [6] | 1992 | Ankle | 01 | Prednisolone | Pruritus | Allergic |
| 7 | Kay J et al., [3] | 1988 | 1st case Knee | 03 | Penicillin, Ampicillin and Minocycline | None | Lyme Disease |
| 2nd case Knee | Tetracycline |
| 3rd case Knee | Salicylates |
| 8 | Brown JP et al., [4] | 1986 | MTP | 01 | NA | Eye allergy | Pseudoallergic |
| Knee | 01 | NA | Eye allergy | Pseudoallergic |
| Knee | 01 | NA | Skin allergy | Pseudoallergic |
| Knee | 01 | NA | Nasal allergy | Pseudoallergic |
| Knee | 01 | NA | Nasal allergy | Pseudoallergic |
| 01 | NA | Asthma | Pseudoallergic |
| 9 | Al-Dabbagh AI and Al-Irhayim B [10] | 1983 | Knee | 01 | Arthrotomy+Penicillin+ Prednisolone | Nasal and pharyngeal alllergy | Pseudoallergic |
| 10 | Amor B et al., [2] | 1983 | Knee (5), Rest NA* | 11 | NA | | Idiopathic (1)Allergic (3)Pseudoallergic (1)Heamarthrosis (1)Post arthrography (2)Psoriatic Rheumatism (1)Filarial arthritis (1)Gougerot Sjogren’s Syndrome (1) |
| 11 | Luzar MJ and Friedman BM [12] | 1982 | Knee | 01 | NA | No | Idiopathic |
| 12 | Klofkorn RW and Lehman TJ [13] | 1982 | 1st case Knee2nd case Knee | 02 | 1st pt Cyproheptadine2nd pt Antihistamine therapy | Urticaria and Angioedema | Allergic |
| 13 | Podell TE et al., [7] | 1980 | Elbow | 01 | No treatment | No | Idiopathic |
| 14 | Hasselbacher P and Schumacher HR [15] | 1978 | NA | 02 | NA | After arthrography | Gout |
| 15 | Goldenberg DL et al., [14] | 1975 | Knee | 01 | Radiotherapy+Chemotherapy | Adenocarcinoma of sigmoid colon | Metastatic synovitis |
MTP: Metatarso-phalangeal; NA: Not available; NSAID’S: Non steroidal anti inflammatory drugs; OA: Osteoarthritis; SFE: Synovial fluid eosinophilia; S. No.: Serial number; TKA: Total knee arthroplasty
*Rest NA means data not available regarding which joint is involved
Haematological parameters and synovial fluid parameters in patients with Eosinophillic Synovitis [2-15].
| S. No. | Study | Blood parameters (TLC/mm3 and Eosinophils in %) | Synovial fluid parameters (TLC /mm3 and Eosinophils in %) |
|---|
| 1 | Present case | 11320 and 29% | 1790 and 79% |
| 2 | Muralidharagopalan NR et al., [11] | 6000 and 12% | 10000 and 95% |
| 3 | Vazquez Trinanes C et al., [8] | | |
| Minor SFE (3 patients) | 1 | NA and no peripheral eosinophilia | 10000 and 1% |
| 2 | NA and no peripheral eosinophilia | 1260 and 3% |
| 3 | NA and no peripheral eosinophilia | 92000 and 2% |
| Major SFE (7 patients) | 4 | 19680 and 410 (2.4%) | NA and 85% |
| 5 | 12590 and 90 (0.7%) | NA and 75% |
| 6 | NA | NA and 20% |
| 7 | 7810 and 0 | NA and 85% |
| 8 | 9500 and 810 (8.5%) | NA and 38% |
| 9 | 13240 and 7280 (54%) | NA and 76% |
| 10 | 7530 and 150 (2%) | NA and 90% |
| 4 | Atanes A et al., [5] | 5020 and 2.4% | 2000 and 67% |
| 5 | Tauro B (12 patients) [9] | Mean 11200 and 6% | 1200-20500, 75-90% in 8 patients., 60-75% in 4 patients. |
| 6 | Padeh S et al., [6] | NA and 1700/mm3 eosinophills | NA,68% |
| 7 | Kay J et al., [3] | 7000 and 3%7000 and 3%11200 and 10% | 18100 and 79%16250 and 34%38850 and 50% |
| 8 | Brown JP et al., [4] | NA and Mean eosinophills 393±82/mm3 | 10850±3665/mm3 and 41±5% |
| 9 | Al-Dabbagh AI and Al-Irhayim B [10] | 11400 and 20% eosinophils | 10500 and 68% eosinophils |
| 10 | Amor B et al., [2] |
| | Allergic | 1 | NA and 399/mm3 | 6300 and 36% |
| 2 | NA and 2180/mm3 | 10000 and 87% |
| 3 | NA and 310/mm3 | 5800 and 33% |
| Pseudoallergic | 4 | NA and 207/mm3 | 3690 and 26% |
| Idiopathic | 5 | NA and No eosinophilia | NA and 73% |
| Rest | 6-11 | NA | NA |
| 11 | Luzar MJ and Friedman BM [12] | NA and No eosinophils | NA and 95% |
| 12 | Klofkorn RW and Lehman TJ [13] (2 pts) | 12000 and 1%8200 and 2% | 12000 and 56%2100 and 7% (minor eosinophilia) |
| 13 | Podell TE et al., [7] | 7000 and 1-2% | 10000 and 83% |
| 14 | Hasselbacher P and Schumacher HR [15] | NA and NA | 5150 and 24% |
| 15 | Goldenberg DL et al., [14] | 7650 and 2% | 8000 and 28% |
NA: Not available; SFE: Synovial fluid eosinophilia; S. No.: Serial number; TLC: Total leucocyte count
Eosinophils are derived from hematopoietic stem cells that give rise to the myeloid series and then to the basophil-eosinophil lineage [16]. The main mediators of toxicity to micro organisms as well as human tissue such as synovitis in this case are eosinophil cationic protein, major basic protein, Eosinophil-Derived Neurotoxin (EDN) [17]. Normal level of eosinophils in the blood is usually 1-6%. Peripheral blood eosinophilia is the usual guide for the presence of an eosinophilic disorder. The degree of blood eosinophilia can be categorised into mild {Absolute Eosinophil Count (AEC) 600-1500 cells/mm3}, moderate (AEC 1500-5000 cells/ mm3), or severe (AEC >5000 cells/ mm3) [18].
Minor SFE, in the range of 1-10%, can occasionally be found in post-traumatic haemorrhagic effusions, rheumatoid arthritis and parasitic diseases. Major SFE is rare and may be found in systemic and local parasitic infections, allergic and pseudoallergic disorders, connective tissue disorders, septic arthritis, pseudogout, in patients with malignancy and in patients with arthrography [4,14,15]. Causes of SFE has been summarised in [Table/Fig-6] [3,11].
Causes of synovial fluid eosinophilia.
| Parasitic diseasesAscariasisAncyclostomiasisFilariasisOthersAllergic and pseudoallergic causesAngioedemaUrticariaDermatographismAtopic diseasesRheumatoid arthritisTubercular arthritisSeptic arthritisPsoriatic arthritisPseudogoutLyme diseasePost traumatic effusionsMalignancyPost-arthrographyRadiationIdiopathic |
The aetiology and pathophysiology of eosinophilic synovitis is unclear. Majority of the patients of Idiopathic variety does not have peripheral eosinophilia at the time of development of synovitis which suggests that synovitis is not in response to a systemic condition. In cases with a specific cause for synovitis such as parasites, metastasis or contrast material; it may be postulated that SFE is a response by the synovium to an unknown stimulus [5]. In present case also, an unknown stimulus may be the triggering factor for accumulation of eosinophils in the synovium causing synovitis.
Many systemic conditions such as Churg Strauss syndrome, Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), Hypereosinophilic Syndrome (HES) and others which cause intense peripheral eosinophilia does not usually cause eosinophilic synovitis and majority of the cases of eosinophilic synovitis does not have peripheral eosinophilia [8].
Brown JP et al., have suggested a ‘pseudoallergic reaction’ in their patients with dermatographism. Pseudoallergic reactions are defined as group of symptoms that mimics the clinical feature of an allergic reaction but its pathophysiology does not involve the usual immunological mechanisms which are associated with immediate type hypersensitivity. Mast cell degranulation in response to physical stimulus has been postulated in patients with dermatographism [4].
The case of pharmacological eosinophilia was reported with the use of fluvastatin. However, no other case of fluvastatin induced eosinophilia has been reported till now [8]. Al-Dabbagh AI and Al-Irhayim B, performed an open synovial biopsy from knee joint and extensive degree of infiltration of synovial lining was found, mainly by eosinophils. However, we did not perform any biopsy [10].
Present case also has been reported from an endemic region for filariasis as similar to cases reported by others, however no any evidence of infection with filaria either in blood or synovial fluid was found [9,11,19].
Kay J et al., reported three cases of SFE with Lyme disease. Two of these patients had protracted course of illness before diagnosis could be made. Even third patient could be diagnosed as Lyme disease after three months of presentation [3]. We did not perform test for Lyme disease at the first presentation and as in present case patient did not had any history of fever, cough, rash, headache, lymphadenopathy, any other joint involvement and she responded well to treatment and swelling has not recurred in follow-up period, we have excluded Lyme disease as the cause.
Conclusion(s)
Eosinophilic synovitis is an uncommon clinical condition. Idiopathic variety has a good prognosis and is easily curable with NSAID’s. More research is required as little is known about the pathophysiology of the disease. Recognition of this clinical entity by the treating clinician is important in preventing the prescription of unnecessary and costlier investigations.
AFB: Acid fast bacilli
MTP: Metatarso-phalangeal; NA: Not available; NSAID’S: Non steroidal anti inflammatory drugs; OA: Osteoarthritis; SFE: Synovial fluid eosinophilia; S. No.: Serial number; TKA: Total knee arthroplasty
*Rest NA means data not available regarding which joint is involved
NA: Not available; SFE: Synovial fluid eosinophilia; S. No.: Serial number; TLC: Total leucocyte count
[1]. Dougados M, Synovial fluid cell analysisBaillieres Clin Rheumatol 1996 10(3):519-34.10.1016/S0950-3579(96)80047-1 [Google Scholar] [CrossRef]
[2]. Amor B, Benhamou CL, Dougados M, Grant A, Eosinophilic arthritis and general review of the significance of articular eosinophiliaRev Rhum Mal Osteoartic 1983 50(10):659-64. [Google Scholar]
[3]. Kay J, Eichenfield AH, Athreya BH, Doughty RA, Schumacher HR Jr, Synovial fluid eosinophilia in lyme diseaseArthritis Rheum 1988 31(11):1384-89.10.1002/art.17803111073056421 [Google Scholar] [CrossRef] [PubMed]
[4]. Brown JP, Rola-Pleszczynski M, Ménard HA, Eosinophilic synovitis: Clinical observations on a newly recognized subset of patients with dermatographismArthritis Rheum 1986 29(9):1147-51.10.1002/art.17802909133753540 [Google Scholar] [CrossRef] [PubMed]
[5]. Atanes A, Fernández V, Núñez R, Galed I, Blanco FJ, García-Porrúa C, Idiopathic eosinophilic synovitis. Case report and review of the literatureScand J Rheumatol 1996 25(3):183-85.10.3109/030097496090800138668965 [Google Scholar] [CrossRef] [PubMed]
[6]. Padeh S, Laxer RM, Gleich GJ, Armstrong PF, Silverman ED, High synovial immunoglobulin E levels in eosinophilic synovitisJ Pediatr 1992 121(3):417-19.10.1016/S0022-3476(05)81799-8 [Google Scholar] [CrossRef]
[7]. Podell TE, Ault M, Sullam P, Klinenberg JR, Synovial fluid eosinophiliaArthritis Rheum 1980 23(9):1060-61.10.1002/art.17802309167417355 [Google Scholar] [CrossRef] [PubMed]
[8]. Vázquez-Triñanes C, Sopeña B, González-González L, Díaz R, Rivera A, Freire M, Synovial fluid eosinophilia: A case series with a long follow-up and literature reviewRheumatology (Oxford) 2013 52(2):346-51.10.1093/rheumatology/kes23623041597 [Google Scholar] [CrossRef] [PubMed]
[9]. Tauro B, Eosinophilic synovitis. A new entity?J Bone Joint Surg Br 1995 77(4):654-56.10.1302/0301-620X.77B4.7615616 [Google Scholar] [CrossRef]
[10]. Al-Dabbagh AI, Al-Irhayim B, Eosinophilic transient synovitisAnn Rheum Dis 1983 42(4):462-65.10.1136/ard.42.4.4626882043 [Google Scholar] [CrossRef] [PubMed]
[11]. Muralidharagopalan NR, Harikrishnan V, Subbaiah S, Srinivasan C, Idiopathic eosinophilic synovitis of the knee joint with peripheral eosinophilia- A rare case reportJ Clin Diagn Res 2015 9(1):RD01-02.10.7860/JCDR/2015/10285.536725738047 [Google Scholar] [CrossRef] [PubMed]
[12]. Luzar MJ, Friedman BM, Acute synovial fluid eosinophiliaJ Rheumatol 1982 9(6):961-62. [Google Scholar]
[13]. Klofkorn RW, Lehman TJ, Eosinophilic synovial effusions complicating chronic urticaria and angioedemaArthritis Rheum 1982 25(6):708-09.10.1002/art.17802506177092970 [Google Scholar] [CrossRef] [PubMed]
[14]. Goldenberg DL, Kelley W, Gibbons RB, Metastatic adenocarcinoma of synovium presenting as an acute arthritis. Diagnosis by closed synovial biopsyArthritis Rheum 1975 18(2):107-10.10.1002/art.17801802021131279 [Google Scholar] [CrossRef] [PubMed]
[15]. Hasselbacher P, Schumacher HR, Synovial fluid eosinophilia following arthrographyJ Rheumatol 1978 5(2):173-76. [Google Scholar]
[16]. Tefferi A, Blood eosinophilia: A new paradigm in disease classification, diagnosis, and treatmentMayo Clin Proc 2005 80(1):75-83.10.1016/S0025-6196(11)62962-5 [Google Scholar] [CrossRef]
[17]. Gleich GJ, Adolphson CR, Leiferman KM, The biology of the eosinophilic leukocyteAnnu Rev Med 1993 44:85-101.10.1146/annurev.me.44.020193.0005058476270 [Google Scholar] [CrossRef] [PubMed]
[18]. Brito-Babapulle F, The eosinophilias, including the idiopathic hypereosinophilic syndromeBr J Haematol 2003 121(2):203-23.10.1046/j.1365-2141.2003.04195.x12694242 [Google Scholar] [CrossRef] [PubMed]
[19]. Narain K, Gupta V, An epidemiological study showing prevalence of lymphatic filariasis in endemic & non-endemic regionsThe J Med Res 2018 4(6):267-73.10.31254/jmr.2018.4604 [Google Scholar] [CrossRef]