A Customised Brachytherapy Radiation Carrier for Squamous Cell Carcinoma of Tongue: A Case Report
Anoop Sharma1, Sweekriti Mishra2, BH Harshitha Gowda3, Sanober Khan4
1 Postgraduate Student, Department of Prosthdontic, Ramaiah University of Applied Sciences, Bangalore, Karnataka, India.
2 Postgraduate Student, Department of Prosthdontic, Ramaiah University of Applied Sciences, Bangalore, Karnataka, India.
3 Reader, Department of Prosthdontic, Ramaiah University of Applied Sciences, Bangalore, Karnataka, India.
4 Postgraduate Student, Department of Prosthdontic, Ramaiah University of Applied Sciences, Bangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Sweekriti Mishra, Ramiah Memorial Hosptial, New Bel Road, Bangalore, Karnataka, India.
E-mail: mishra.sweekriti23@gmail.com
Squamous Cell Carcinoma (SCC) of the tongue is the most widely recognised malignant neoplasm, representing 25 to 50% of all oral malignancies. In recent years, brachytherapy has been used in management of neoplasms of the head and neck region. This clinical report illustrates a method of customised mould fabrication for a 48-year-old patient diagnosed with SCC of lateral border of tongue undergoing brachytherapy treatment and emphasises the responsibility of a maxillofacial prosthodontist in designing a non-invasive prosthesis which maintains the radiotherapy catheters in the required predetermined position as per the requirement of the radiologist.
Customised mould brachytherapy, Radiation carrier, Tongue carcinoma
Case Report
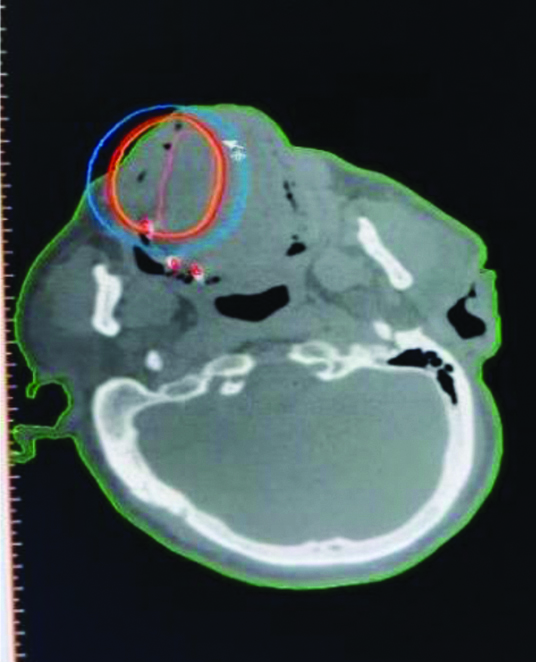
A 48-year-old male patient reported to Department of Radiology, Ramaiah Medical Hospital, Bangalore (Karnataka, India) with a chief complaint of a non-healing ulcerative lesion on the left side of his tongue since two years. On examination a 1.4 × 2.7 cm ulcerative lesion [Table/Fig-1] involving the left lateral border extending onto the dorsal surface of tongue was noted, with no palpable lymph nodes. The lesion had gradually progression with no slough formation, irregular or undermined edges. No history of burning sensation, difficulty in swallowing, tooth loss or bleeding was reported. The oral hygiene of the patient was good; the interincisal opening was approximately 39 mm (which is within the normal range) without restricted tongue movements. Past medical history revealed non-ST segment elevation myocardial infarction, for which he underwent coronary angioplasty a month back. The Computed Tomography (CT) [Table/Fig-2] and Magnetic Resonance Imaging (MRI) revealed a soft tissue growth with no signs of bone invasion or gross lymphadenopathy. Biopsy and histopathological reports indicated stage 1 (T1N0M0) carcinoma. Patient was diagnosed with SCC of lateral border of the tongue. Due to medical history of the patient, in order to avoid any invasive procedure mould brachytherapy of lateral border of tongue was planned by Department of Radiology, Ramaiah Medical Hospital and patient was referred to Faculty of Dental Sciences, Bangalore (Karnataka, India), for the fabrication of carrier device.
Lesion on the lateral border of tongue.

Horizontal view of computer tomography scan showing extend of lesion.
Procedure for fabrication of radiation device involving lateral border of tongue:
The extent of tumour was marked using an eosin pencil and the impression of tongue was made using putty elastomer material (Aquasil). The tip of the tongue was extended outward in a comfortable position until the material sets.
The impression was disinfected and poured with Type III dental stone (Kalstone, Kalabhai) to prepare a definitive cast.
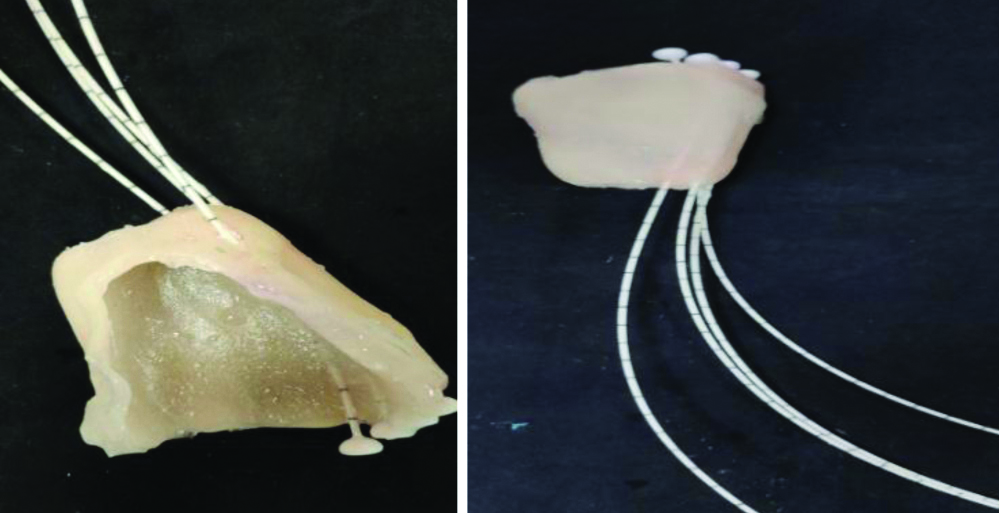
Modelling wax of thickness 1.7 mm (Hindustan modeling wax) was adapted onto the cast in order to prevent direct contact of prosthesis with the lesion [Table/Fig-3]. Four longitudinal wax rolls of 2 mm diameter (Hindustan modeling wax) were placed parallel to each other at a distance of approximately 10 mm, which would indicate the position of the catheter. The number, placement and position of the catheter were consulted with the radiation oncologist and the design of the prosthesis was customised according those requirements. The catheter was secured within the slots (made using four longitudinal wax rolls) using cyanoacrylate adhesive (pidilite).
Wax rolls showing placement of catheral tubes.

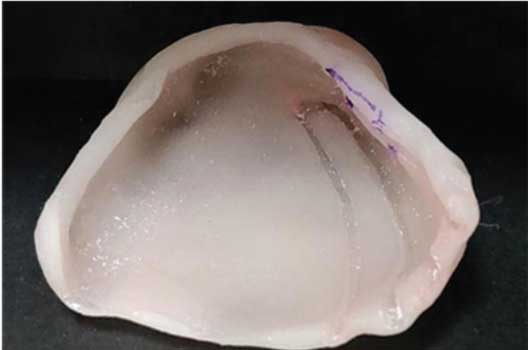
The final appliance was fabricated with clear autopolymerising acrylic resin (DPI RR cold cure) with a thickness of 2-3 mm for better visualisation [Table/Fig-4].
Finished and polished mould.
After finishing and polishing, the fit of the prosthesis was assessed in the patient’s mouth and the patency of the catheter tubes was analysed using lead wire.
In order to stabilise the appliance during administration of radiation (10 minutes) relief was provided around the tip of the tongue [Table/Fig-5,6].
Making the tip of the tongue.

Opening provided for the tip of the tongue.

Soft relining material (GC soft-liner) was placed onto the inner surface of the prosthesis to prevent direct contact of catheter tubes with each other as well as the mucosa. Soft relining of the prosthesis also provided retention stability and patient’s comfort [Table/Fig-7].
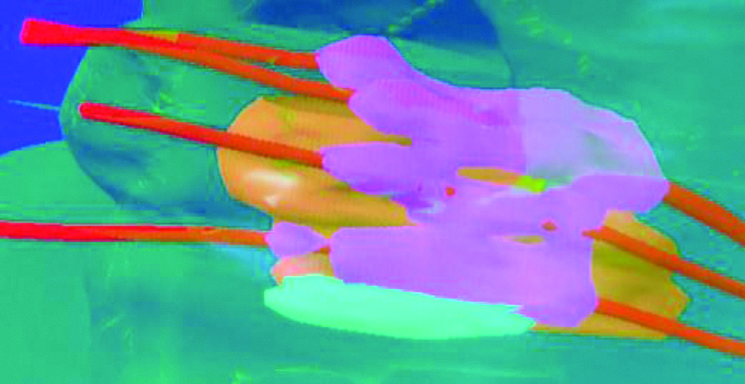
Mock radiation test and CT scan was carried out in order to check the reliability of the device, before starting the procedure. After the source patency was confirmed, the radiation carrier was placed in the patient’s mouth and the catheters were connected to the machine. A fractionated scheme of 34 Gray/10 fractionations; twice a day for 7 days was used as decided by the radiation-oncologist [Table/Fig-8,9]. Subsequent follow-up was done for 7 months.

Sagittal view computed tomography scan showing mould in position with radioactive sources.
Thus, a carrier device was fabricated fulfilling all the requirements needed for a brachytherapy mould.
Discussion
Among the South Indian population the prevalence rate of SCC of the tongue is 14% in which lateral border is most commonly affected [1]. Various treatment options that are present for the management of SCC include surgical excision, chemotherapy, and radiotherapy. In recent years, radiation therapy has emerged as an effective treatment modality for superficial lesion of head and neck carcinomas [2]. Cano ER et al., stated brachytherapy was well tolerated by the patients and resulted in fewer complications [3]. Brachytherapy is a form of intra-operative radiation [4] wherein sealed radioactive sources are used to deliver predetermined doses of radiation directly onto the affected area [5]. Brachytherapy is classified as interstitial, intraluminal and surface application brachytherapy (mould). Mould brachytherapy requires construction of specialised carrier for the treatment of superficial lesion [6] and is considered as an excellent treatment option as it allows areas specific dose distribution [7,8]. This method allows short treatment time and thereby reducing the post radiotherapy sequelae of xerostomia, mucositis, dysphagia, and dysgeusia [9-11]. In addition, there is no radiation hazard to the therapists and nursing staff. However, the method is extremely limited in its application to oral carcinomas because the catheters are not sufficiently flexible to fit along complex anatomically contour of the oral cavity.
Literature highlights few reports on the use of mould brachytherapy [10-13] out of which none revealed fabrication of mould brachytherapy for lateral border to tongue. There are various types of carrier devices that are available; they can either be preloaded or after loaded. The other types are intracavitory and interstitial [14].
Maxillofacial prosthodontist plays a crucial role in the construction of the mould. An impression of the lesion will aid in deciding the location of the catheters for adequate dose distribution. The appliance should have good retention, stability and support which will ensure delivery of radiations to the desired location. The mould should be fabricated such that catheters remain patent without bending as their bending would cause source obstruction thereby hampering the flow of radiation. Previous studies have shown that the thickness of acrylic does not interfere with delivery of radiation [15,16]. The current case report describes a technique for fabrication of radiation carrier that utilises materials which are accessible to prosthodontist, thereby making it simple and cost-effective.
Setting reaction of cold cure generates heat and since catheters are sensitive to the heat, wax rolls were prepared instead of directly in cooperating them into the wax pattern. The parallel placement of catheter and the opening provided in the appliance for each one avoided the risk of bending. Soft liner was used to fill the space between the tongue and the device, and to restrict movement of the prosthesis during treatment, which aided in retention, stability and support. The opening for the tip of tongue provided visual assurance that the tongue was in same position throughout the delivery of radiation. The device was sterilised after each cycle and follow-up was carried out to check for its efficiency. It was noted that custom-made mould is easy to use and it ensured patient comfort.
Conclusion(s)
The current case report describes a method for the fabrication of mould brachytherapy appliance that is simple and non-invasive with good patient acceptability which can be used for treating squamous cell carcinoma involving lateral border of tongue.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jan 11, 2020
Manual Googling: Mar 04, 2020
iThenticate Software: Mar 24, 2020 (12%)
[1]. Landis SH, Murray T, Bolden S, Wingo PA, Cancer statistics, 1999CA Cancer J Clin 1999 49(1):08-31.10.3322/canjclin.49.1.810200775 [Google Scholar] [CrossRef] [PubMed]
[2]. Takeda M, Shibuya H, Inoue T, The efficacy of gold-198 grain mould therapy for mucosa carcimonas of the oral cavityActa Oncol 1996 35:463-67.10.3109/028418696091099238695162 [Google Scholar] [CrossRef] [PubMed]
[3]. Cano ER, Lai SY, Caylakli F, Johnson JT, Ferris RL, Carrau RL, Management of squamous cell carcinoma of the base of tongue with chemoradiation and brachytherapyHead Neck 2009 31(11):1431-38.10.1002/hed.2111119405086 [Google Scholar] [CrossRef] [PubMed]
[4]. Selvamani M, Yamunadevi A, Basandi PS, Madhushankari GS, Prevalence of oral squamous cell carcinoma of tongue in and around Davangere, Karnataka, India: A retrospective study over 13 yearsJ Pharm Bioallied Sci 2015 7(Suppl 2):S49110.4103/0975-7406.16351126538904 [Google Scholar] [CrossRef] [PubMed]
[5]. Sela M, Taicher S, Intraoral radiation carrier for edentulous patientsJ Prosthet Dent 1983 50(6):815-17.10.1016/0022-3913(83)90097-5 [Google Scholar] [CrossRef]
[6]. Beumer J, Curtis TA, Firtell DN, Maxillofacial rehabilitation: Prosthodontic and surgical considerations 1979 St. LouisMosby:40-1. [Google Scholar]
[7]. Wadhwa SS, Duggal N, A customised finger brachytherapy carrierJ Indian Prosthodont Soc 2014 14(3):326-29.10.1007/s13191-012-0250-625183922 [Google Scholar] [CrossRef] [PubMed]
[8]. Ersu B, Custom made mold brachytherapyBasal Cell Carcinoma 2012 :110.5772/26589 [Google Scholar] [CrossRef]
[9]. Rustgi SN, Cumberlin RL, An after loading 192-Ir surface moldMed Dosim 1993 18:39-42.10.1016/0958-3947(93)90026-P [Google Scholar] [CrossRef]
[10]. Poojary S, Singhania S, Role of maxillo-facial prosthodontist to aid in brachytherapy for squamous cell carcinoma of palate with ancillary prosthesis: A case reportJournal of Dental and Orofacial Research 2018 14(1):70-74. [Google Scholar]
[11]. Dantas DD, Ramos CC, Costa AL, Souza LB, Pinto LP, Clinical pathological parameters in squamous cell carcinoma of the tongueBraz Dent J 2003 14:22-25.10.1590/S0103-6440200300010000412656460 [Google Scholar] [CrossRef] [PubMed]
[12]. Chalian VA, Drane JB, Standish SM, Maxillofacial prosthetics 1972 BaltimoreThe William and Wilkins Company:181-183. [Google Scholar]
[13]. Garrán C, Montesdeoca N, Martínez-Monge R, Treatment of upper gum carcinoma with high-dose-rate customised-mold brachytherapyBrachytherapy 2008 7(3):267-69.10.1016/j.brachy.2008.04.00118635026 [Google Scholar] [CrossRef] [PubMed]
[14]. Palaskar J, Mody ZS, Mohila SS, Wankhade JH, Sayali R, Virdiya N, Different types of radiation prostheses to minimize radiation side-effectsInternational Journal of Clinical Research 2016 8(06):33575-78. [Google Scholar]
[15]. Ariji E, Hayashi N, Kimura Y, Uchida T, Hayashi K, Nakamura T, Customised mold brachytherapy for oral carcinomas through use of high-dose-rate remote after loading apparatusOral Surg Oral Med Oral Pathol Oral Radiol Endod 1999 87(4):508-12.10.1016/S1079-2104(99)70253-2 [Google Scholar] [CrossRef]
[16]. Fujita M, Tamamoto M, Hirokawa Y, Kashiwado K, Akagi Y, Kashimoto K, Experimental and clinical studies on dose reduction effects of spacers in interstitial brachytherapy for carcinoma of the mobile tongueOral Surg Oral Med Oral Pathol 1993 76:797-803.10.1016/0030-4220(93)90054-8 [Google Scholar] [CrossRef]