Bone is a dynamic heterogeneous tissue, which is structurally important and plays a major role in mineral homeostasis and hematopoiesis. Together, bones and joints provide mechanical support for movement, protect viscera, and determine the attributes of body size and shape [1].
Among the myriad tumours, bone tumors are relatively uncommon, constituting only 0.5% of the total world cancer incidence [2]. Bone lesions are diverse, relatively rare and range from being harmless to rapidly fatal. This diversity makes it critical in diagnosis, staging and treating bone tumours and tumour-like lesions precisely [2]. Some groups of these neoplasms can affect all ages while some others are mostly developed during the first few decades of life [3]. If cancer is diagnosed during adolescence and young adulthood, patients need additional care and follow-up, as it can have devastating effects in the future, including development of secondary cancers even after clinical cure [4].
The structural complexity of bone gives rise to primary malignant tumors of different histogenesis in addition to secondary tumours [5]. Primary bone tumours constitute 0.2% of all tumours in an individual and some of these tumours show inter and intra national variations insite, incidence and age distribution [6]. Low incidence of tumours and the limited experience in nonspecialised centers is probably a major factor for inaccurate diagnosis [7].
Diagnosing a bone tumour is a challenging task to the surgical pathologist, and a systematic approach to clinical history, radiographic evaluation and histopathology is necessary for accurate diagnosis [11]. Diagnosis of bone tumours remain an alarming challenge to the pathologists and surgeons especially in un-co-operative patients. Clinico-radiological diagnosis can be a non-invasive method suggestive of probable diagnosis in agitated patients. Clinico-radiological diagnosis followed by subsequent histopathological confirmation remains an affirming means of diagnosis of bone tumours which are nonconclusive or incompletely diagnosed on FNAC. Analysis of agreement between the various diagnostic modalities can be helpful to clinicians in providing the most accurate treatment, which is not available at most of the hospitals. Hence, present study was conducted to analyse the level of agreement between the initial clinico-radiological and the subsequent histopathological diagnosis of bone tumours and tumour-like lesions.
Materials and Methods
This was a prospective study conducted in the Department of Pathology at MS Ramaiah Hospital, Bengaluru, over a period of two years from May 2009 to April 2011 (including analysis done over a period of one month). For analysis, bone lesion biopsies, curetting and excised specimen collected from patients were received from the Pathology Department. Patients of all ages irrespective of gender, with biopsy proven primary and metastatic bone tumours were included in the study, maintaining their anonymity throughout, and patients with haematological malignancies involving bone marrow were excluded. For all patients on whom biopsy and/or surgery was performed, informed consent was taken before the procedure and institutional ethical clearance (STD-1/09) for the same was obtained from the Medical Education Unit.
The biopsy specimens were systematically examined after noting down the clinical history from patient records, which included presenting complaints, family history, past history, general physical examination, systemic examination and if lymph nodes were palpable or not. Investigations like haemoglobin percentage, total count, differential count erythrocyte and sedimentation rate were performed. Radiological findings like MRI images (Magnetic Resonance Imaging), CT scan (Computed Tomography) and X-ray obtained from the medical records of the patient were examined. Soft tissues were processed routinely by paraffin section for light microscopy, after fixation in 10% neutral buffered formalin. The large bony pieces were cut into smaller fragments (2-6 mm), fixed in 10% neutral buffered formalin and washed before subjecting to decalcification. Decalcification solution used was 5% nitric acid until the tissue softened, following which they were taken for processing. Sections thus obtained were stained with haematoxylin and eosin. Special stains for collagen/fibrous tissue and IHC (immunohistochemistry) were performed as and when required. The immunohistochemical markers used were CD99, CD20, CD3, CD30, S-100, cytokeratin. The technique for IHC used was “super sensitive link label HRP (Horseradish peroxidase) detection system” which included antigen retrieval in citrate buffer in a microwave oven and blocking endogenous peroxidase with 3% hydrogen peroxide. Incubation was done with primary mouse monoclonal antibody against CD99, CD20, CD3, CD30, S-100 protein, cytokeratin and linking with rabbit anti mouse secondary antibody (Biogenex). Enzyme labelling was done with streptavidin-horseradish peroxidase. Chromogen developed with deaminobenzidine (DAB) and counter stained with haematoxylin. Positive and negative controls were run with each batch of slides.
Sample Size Calculation
A study by Negash BE et al., entitled “Bone tumours at Addis Ababa University, Ethiopia: Agreement between radiological and histopathological diagnosis, a- 5-year analysis at Black-Lion teaching hospital” has revealed that the agreement between the radiological and histopathologic diagnosis was 84% [10]. Based on the above study findings with a relative precision of 11% and desired confidence level of 95% it was estimated that a minimum of 60 samples need to be included for the study. However, we included 64 cases in the study.
Statistical Analysis
All the data was initially presented in the form of frequency distribution tables. Respective percentages were calculated for each of the groups based on the total number of patients studied. To understand the clinico-radiologic and histopathologic diagnosis, the data was presented in the form of bivariate tables. Further to understand the extent of association between the various diagnostic entities, kappa statistics was estimated and interpreted. All the analysis was carried out on SPSS 18.0 version. The data was analysed and strength of agreement in diagnosis was calculated using Kappa statistics. For calculating the sensitivity and specificity, the diagnostic entities need to be dichotomised into 2 groups only. Since, the radiologic findings could not be dichotomised into 2 groups unlike histopathologic findings, the sensitivity and specificity could not be calculated.
Results
The [Table/Fig-1] shows the demographical details of the cases. Significance of tumour-like bony lesions is, that their radiologic appearance may mimic that of malignant bone tumours which gives rise to differential diagnostic problems but lack histopathologic changes of pleomorphism, necrosis and mitotic activity and they are quite commonly seen in clinical practice.
Demographical features of cases.
The [Table/Fig-2] shows the common clinical symptoms and sites of tumour in cases. Among which pain and swelling was most common symptom and the commonest tumor site was tibia upper half.
Clinical Symptoms and site distribution of cases.
| Criteria | Frequency (n=64) | Percent (%) |
|---|
| Symptoms | Pain and swelling | 28 | 43.8 |
| Pain | 24 | 37.5 |
| Swelling | 7 | 10.9 |
| Pain and restriction of movements | 2 | 3.1 |
| Constipation | 1 | 1.6 |
| Pain, swelling and difficulty in walking | 1 | 1.6 |
| Inability to walk | 1 | 1.6 |
| Site of tumour | Tibia upper half | 14 | 21.88 |
| Femur lower half | 10 | 15.63 |
| Humerus upper half | 6 | 9.38 |
| Femur upper half | 6 | 9.38 |
| Sacrum | 5 | 7.81 |
| Ilium | 4 | 6.25 |
| Multiple | 3 | 4.69 |
| Spine | 3 | 4.69 |
| Radius lower half | 3 | 4.69 |
| Phalynx | 2 | 3.13 |
| Scapula | 2 | 3.13 |
| Fibula upper half | 1 | 1.56 |
| Fibula lower half | 1 | 1.56 |
| Pubis | 1 | 1.56 |
| Maxilla | 1 | 1.56 |
| Ischium | 1 | 1.56 |
| Sacrum and ilium | 1 | 1.56 |
| Regions involved | Epiphysis | 17 | 26.6 |
| Flat bones | 17 | 26.6 |
| Metaphysis | 12 | 18.8 |
| Diaphysis | 6 | 9.4 |
| Meta-diaphysis | 4 | 6.3 |
| Epi-metaphysis | 2 | 3.1 |
| Multiple | 2 | 3.1 |
| Meta-apophysis | 2 | 3.1 |
| Diffuse involvement | 1 | 1.6 |
| Apophysis | 1 | 1.6 |
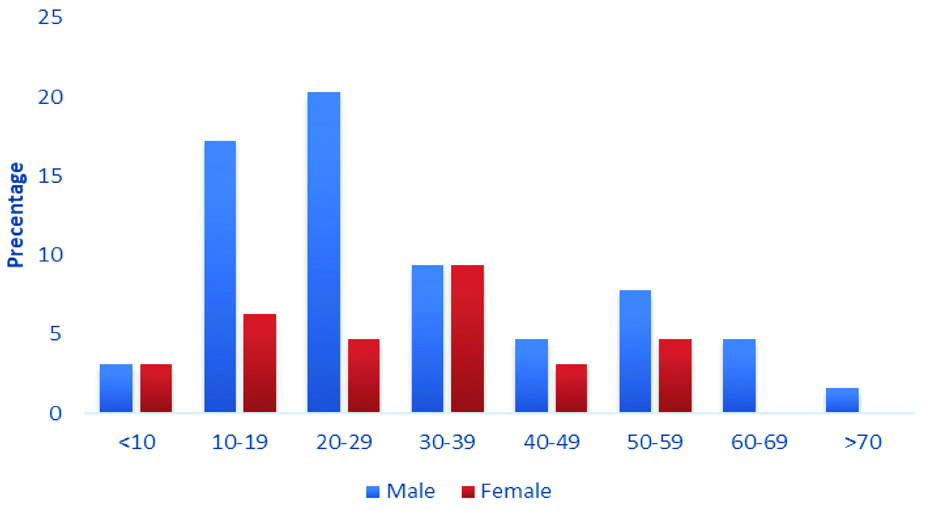
The [Table/Fig-3] shows the distribution of bone lesions based on age. The most common age group for tumour was 20-29 years followed by 10-19 years and 30-39 years.
Age distribution based on behaviour and number of bone lesions.
| Age (years) | Tumour (n=64) | Total |
|---|
| Benign | Malignant primary | Metastasis | Tumour like lesion |
|---|
| n | Percent (%) | n | Percent (%) | n | Percent (%) | n | Percent (%) | n | Percent (%) |
|---|
| <10 | 0 | 0.00 | 1 | 25.00 | 0 | 0.00 | 3 | 75.00 | 4 | 6.25 |
| 10-19 | 8 | 53.33 | 7 | 46.67 | 0 | 0.00 | 0 | 0.00 | 15 | 23.44 |
| 20-29 | 6 | 37.50 | 9 | 56.25 | 0 | 0.00 | 1 | 6.25 | 16 | 25.00 |
| 30-39 | 6 | 50.00 | 3 | 25.00 | 2 | 16.67 | 1 | 8.33 | 12 | 18.75 |
| 40-49 | 1 | 20.00 | 3 | 60.00 | 1 | 20.00 | 0 | 0.00 | 5 | 7.81 |
| 50-59 | 1 | 12.50 | 5 | 62.50 | 2 | 25.00 | 0 | 0.00 | 8 | 12.50 |
| 60-69 | 1 | 33.33 | 0 | 0.00 | 2 | 66.67 | 0 | 0.00 | 3 | 4.69 |
| >70 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 1 | 100.00 | 1 | 1.56 |
| Total | 23 | 35.94 | 28 | 43.75 | 7 | 10.94 | 6 | 9.38 | 64 | 100.00 |
Benign tumours 18 (41.8%) and tumour-like lesions 5 (11.6%) were seen mostly in males, while malignant primary tumours 10 (47.6%) and metastasis 5 (23.8%) were mostly seen in females [Table/Fig-4].
Gender distribution based on behaviour and number of bone lesions.
| Gender | Tumour | Total (n=64) |
|---|
| Benign (n=23) | Malignant primary (n=28) | Metastasis (n=7) | Tumour like lesion (n=6) |
|---|
| n | Percent (%) | n | Percent (%) | n | Percent (%) | n | Percent (%) | n | Percent (%) |
|---|
| Male | 18 | 41.8 | 18 | 41.8 | 2 | 4.6 | 5 | 11.6 | 43 | 67.19 |
| Female | 5 | 23.8 | 10 | 47.6 | 5 | 23.8 | 1 | 4.7 | 21 | 32.81 |
In this study, radiological diagnosis was confirmed by subsequent histopathological diagnosis [Table/Fig-5]. The corresponding Kappa statistics value (0.749) showed substantial agreement between radiological and histopathological diagnosis of all bone tumours [Table/Fig-6]. However, of the 64 cases, 7 cases had shown disagreement between clinico-radiological and histopathological diagnosis.
Clinico-radiological versus histopathological diagnosis of bone tumours and tumour-like lesions.
| Histopathological diagnosis |
|---|
| Clinico- Radiological diagnosis | Osteochondroma | Chondroblastoma | Chondrosarcoma | Osteoid osteoma | Osteosarcoma | Desmoplastic fibromas | Primary bone malignant lymphoma | GCT | Chordoma | Ewing sarcoma | Metastasis | ABC | SBC | Fibrous dysplasia | LCH | Total |
|---|
| Osteochondroma | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| Chondroblastoma | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| CMF | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Chondrosarcoma | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 |
| Osteoid osteoma | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Osteosarcoma | 0 | 0 | 0 | 0 | 12 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 13 |
| GCT | 0 | 0 | 0 | 0 | 2 | 1 | 0 | 14 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 17 |
| Chordoma | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| Ewing sarcoma | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 3 |
| Metastasis | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 6 | 0 | 0 | 0 | 0 | 7 |
| ABC | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 3 |
| SBC | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 2 |
| Fibrous dysplasia | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 2 |
| LCH | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| Dentigerous cyst | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Total | 3 | 3 | 5 | 1 | 16 | 1 | 1 | 16 | 3 | 3 | 6 | 2 | 2 | 1 | 1 | 64 |
CMF: Chondromyxoid fibroma; GCT: Giant cell tumour; ABC: Aneurysmal bone cyst; SBC: Solitary bone cyst: LCH: Langerhans cell histiocytosis
Measure of agreement between histopathological and radiological diagnosis by Kappa statistics.
| Kappa value | Standard error | Approximate p-value |
|---|
| Measure of agreement | 0.749 | 0.0584 | <0.001 |
| Number of valid cases | 64 |
Discussion
Histological examination of bone tumours is comparatively rare and one of the most difficult subjects. Primary benign and malignant bone tumours vary extensively in their clinical behaviour and pathological features [11,12]. Low incidence of these tumours and limited experience in non-specialised centres is the main cause for differences between the initial diagnosis made on clinico-radiological assessment and final histopathological diagnosis [13]. Biopsy is very important to describe the characteristics of bone tumours according to behavior and histopathologic type. However, since most bone lesions are not biopsied, it is difficult to evaluate their precise incidence [14]. In the present study, the assessment of the agreement between clinico-radiological diagnosis with histopathological diagnosis was carried out on 64 cases. Male preponderance was seen in benign, malignant and tumour-like lesions with male:female ratio of 1:0.24, 1:0.67, 1:0.4, respectively, which indicated that males were more affected than females, similar to results by Nayar M et al., [15]. The age distribution from the present study showed that majority of lesions occurred in the second decade of life (29.4%), followed by third decade (23.5%), again in accordance with the study by Nayar M et al., [15].
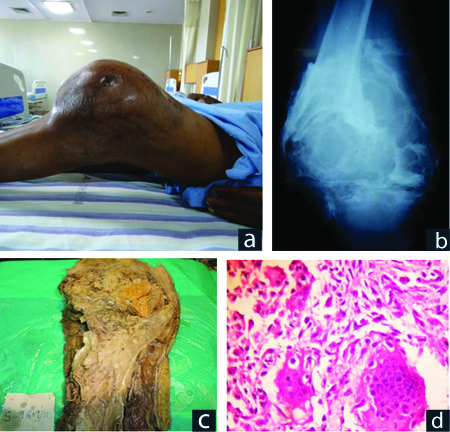
In the present study, malignant tumours comprising of malignant primary and metastatic tumours, were more commonly encountered, constituting 35 (54.6%) of the total lesions. The findings reported by Chitale AR and Jambhekar NA was 52.5% and Nayar M et al., was (66.4%) [12,15]. In this study, osteosarcoma was the most common tumour (45.7%), irrespective of age, similar to studies by Rao VS et al., (45.7%) and Dorfman HD and Czernaik B, (35.9%) [Table/Fig-7a-e] [16,17]. According to this study, osteosarcoma (22.7%) was found to be the most common tumour among children, which was similar to the study by Taran SJ et al., [18]. The most common benign tumour was giant cell tumour (osteoclastoma), forming 65.4% of the bone tumours observed, which is similar to the study by Broehm CJ et al., [Table/Fig-8a-d] [19]. Among tumour-like lesions, we found that Aneurysmal bone cyst was seen most frequently (42.9%), similar to observations by Rao VS et al., (30.5%) [16], but in contrast to Nayar M et al., who found fibrous dysplasia to be the most common (33.3%) and Aneurysmal bone cyst to be the second most common tumour-like lesion (26.7%) [15].
Osteosarcoma. (a) Swelling in left distal thigh; (b) X-ray: Pathological fracture femur, mixed lytic, sclerotic mass; (c) Specimen of left distal femur and proximal tibia with tumour; (d) Osteoid with sheets of (e) Pleomorphic spindle cells spindle cells (H&E X100) (H&E X400).

Giant cell tumour. a) Massive swelling around left knee (b) X-ray-Expansile lytic lesion with septae in left femur; (c) Specimen of left above knee amputation Grey white mass with areas of hemorrhage; (d) Osteoclastic giant cells with neoplastic stromal spindle cells (H&E X400).
In the present study, the strength of agreement between clinico-radiological diagnosis and histopathological diagnosis was found to be substantial (kappa value:0.749), and close to the study results by Negash BE et al (kappa value:0.82) [10]. The present study serves as a great help in the improvement of bone lesion evaluation. Though radiology may not give the exact histological variant of the bone tumour, it accurately indicates the nature of the lesion.
Of 13 cases of osteosarcoma, 12 were concordant and one discordant. The case was clinic-radiologically diagnosed as Ewing sarcoma. Discordancy was because of minimal sclerotic margin on radiology and less common location i.e., in the metadiaphysis. Single case of Desmoplastic fibroma was diagnosed as Giant cell tumour due to lytic lesion radiologically [Table/Fig-9a-d]. Of 17 biopsy proven cases of Giant cell tumor, two were discordant, one due to focal lytic lesion radiologically involving the ilium and pubic symphysis and clinical correlation in a known case of cervical Squamous cell carcinoma. The other case was diagnosed as Aneurysmal bone cyst in a 13-year-old male child. Of the three cases of Ewing sarcoma diagnosed on radiologic diagnosis, one was proven as Osteosarcoma on histopathology but because of late presentation proved a radiologic mimic of Ewing. IHC resolved the case [Table/Fig-10a-d]. A single case of biopsy proven lymphoma was diagnosed radiologically as Ewing sarcoma in a 24-year-old male. Immunohistochemistry resolved the case. Lastly, of five cases of chondrosarcoma, one was radiologically diagnosed as benign cartilage producing lesion chondromyxoid fibroma. The reasons for discordancy occurred mainly because radiologically bone formation or destruction can be associated with many conditions besides bone tumours. Hence, clinical signs and symptoms have a major weightage, besides certain lesions are more common in a particular age group and at a particular site in the bone and the type of bone involved.
Desmoplastic fibroma. (a) X-ray: Expansile lytic lesion with trabeculations in left tibia; (b) MRI: Heterogenous eccentric lesion; (c) Specimen of left proximal tibia with irregular grey white mass; (d) Spindle cells without atypia (H&E X100).

Ewing sarcoma. (a) X- ray: Permeative lytic lesion of (b) CT-lytic and sclerotic lesion of left left ilium. Ilium with soft tissue extension. (c) Small round tumour cells. (d) CD99 positive tumour cells. (X100) (H&E X100).

The [Table/Fig-11,12 and 13] show the radiologic, gross and microscopic characteristics of the other various spectrum of tumours of the bone encountered.
Chordoma. (a) X-ray: Lytic lesion in lower sacrum and coccyx, (b) MRI: Irregularly lobulated hyperintense region; (c) and (d): Partial sacrectomy specimen. (e) Physaliferous cells in lobules. (H&E X100).

Osteosarcoma: Fibroblastic type. (a) X-ray: Right tibia-lytic lesion with rim of sclerosis; (b) Specimen of right proximal tibia - Irregular, necrotic, hemorrhagic grey white tumour. (c) Sheets of pleomorphic spindle cells.

Chondrosarcoma. (a) X-ray: Lytic lesion with specks of calcification in right distal femur (b) MRI: Hyperintense lesion; (c) Specimen of right distal femur: Grey white mass (d&e): Pleomorphic chondrocytes against chondroid matrix (H&E A X100. B X400)

Histopathologic evaluation to confirm the radiologic diagnosis is essential and confirmatory in difficult cases and as a convention when the lesions distort bone and soft tissues, to decide whether benign or malignant, upon which the treatment strategy rests.
Limitation(s)
A main drawback of this study was that only the first diagnosis in the differential was considered for evaluation. The results may have varied, and the agreement would have been even higher, if the first and/or second lesion in the differential radiological diagnosis (e.g., Ewing Sarcoma, Lymphoma) were considered for agreement with the histopathological diagnosis. The study value would be more enhanced if the sample size was increased.
Conclusion(s)
Bone tumours and tumour like lesions are not uncommonly encountered in clinical practice. Good clinical examination with expert radiologic interpretation is a must. Histopathological examination is the gold standard for establishing most accurate diagnosis for appropriate treatment. Ancillary diagnostic techniques as special stains, immune histochemistry, cytogenetics are required in special cases for confirmation.
CMF: Chondromyxoid fibroma; GCT: Giant cell tumour; ABC: Aneurysmal bone cyst; SBC: Solitary bone cyst: LCH: Langerhans cell histiocytosis