Odontogenic Keratocysts (OKC) are a developmental odontogenic cysts arising from remnants of the dental lamina. They differ from other odontogenic cysts due to their aggressive growth behaviour and high recurrence rates. Malignant or benign transformation may develop from their epithelium. Ameloblastomatous transformation of OKC is an extremely rare case. Such lesions have been described as combined or hybrid odontogenic lesions. In this case report, a 22-year-old patient presented with an unusual lesion in the mandible showing histological features of both OKC and ameloblastoma, and review of the available literature regarding the combined lesions.
Case Report
A systemically healthy 22-year-old male patient was referred to Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Ondokuz Mayıs University, Turkey with painless swelling in the left lower jaw for 2 months. Three weeks before the first visit, the patient was prescribed antibiotics by another dental clinic because of swelling in the left side of the jaw. On extraoral examination, a mild, painless swelling was observed on the left gonial region and ramus of mandible, but overlying skin was normal. There was no lymphadenopathy, limitation in jaw movements and neurologic deficit. Intraoral examination revealed a mild swelling on the lingual aspect, extending from the left lower third molar to the ascending ramus of mandible, there was no expansion at the buccal and lingual cortex, oral mucosa was intact and left lower third molar was missing.
Panoramic radiograph (OPG) revealed an unilocular well-defined with dimensions of 40 mm × 25 mm ovoid radiolucent area involving an impacted tooth on the lower left side that extended from the second molar to the subcondylar region [Table/Fig-1a]. Cone beam computerised tomographic examination showed that the lingual cortex of the ramus was destroyed by extensive lesion [Table/Fig-1b,c].
Preoperative panoramic image: (a) showing ovoid radiolucent area involving an impacted tooth that extended from the second molar to the subcondylar region. Axial (b) and sagittal (c) section of CBCT showing resorption of lingual cortical bone of the ascending ramus.

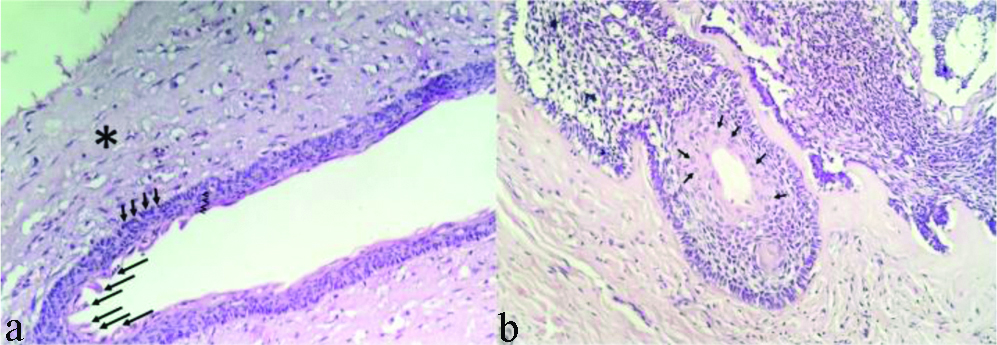
Fine needle aspiration biopsy was performed and no aspirate was obtained. Under local anaesthesia, the impacted third molar tooth was extracted and an incisional biopsy was taken from the lesion for histopathologic examination. Histologic examination revealed a cyst was lined by stratified squamous epithelium with superficial corrugated parakeratosis, approximately 4-6 cell layers and palisaded basal cell layer resembling the OKC [Table/Fig-2a]. Some areas inside the cyst wall showed stellate reticulum-like epithelial cells and a basal cell layer of tall columnar cells with palisaded, revers polarised nuclei resembling the ameloblastomatous epithelium [Table/Fig-2b]. The lesion was diagnosed as Odontogenic Keratocyst (OKC) with ameloblastomatous transformation.
a) Histopathological appearance of the OKC showing a thin connective tissue wall (*) lined by stratified squamous epithelium (arrow heads) with superficial corrugated parakeratosis (long arrows) and palisaded basal cell layer (short arrows); b) Some areas showed stellate reticulum-like epithelial cells (arrows) resembling the ameloblastomatous epithelium (a&b, H&E stain, ×200).
The patient was operated under general anaesthesia. Extraoral submandibular incision was performed [Table/Fig-3a]. Tooth 37 was extracted, marginal resection and curettage was performed by preserving the healthy bone tissue at the inferior border of corpus and posterior border of ascending ramus. Inferior alveolar neurovascular bundle was dissected and preserved [Table/Fig-3b]. Approximately, 6 cm of bone tissue involving the lesion was removed with marginal resection. Reconstruction plate (KLS-Martin, Tuttlingen, Germany) was placed to strengthen the remaining bone tissue and to reduce the risk of fracture. The defect in the alveolar residual ridge was reconstructed by corticocancellous block graft obtained from the anterior crista iliaca and was fixed with 1 mini plate and 4 mini screws (KLS-Martin, Tuttlingen, Germany) [Table/Fig-3c,4a]. The distal flap was closed primarily with 3-0 Vicryl (Ethicon). The patient was discharged on the post-operative fifth day. Oral antibiotics and anti-inflammatory drugs were prescribed.
a) Intra-operative view of incision line planning (arrow) and projection of the mandible (*). b) Intra-operative view of inferior alveolar neurovascular bundle. c) Reconstruction of mandible with anterior crista iliaca graft and reconstruction plate.

Post-operative panoramic radiograph: (a) showing reconstructed mandible; (b) 20 months follow-up.

No complication was observed during the postoperative follow-up. There was no problem in the functional jaw movements and sensory functions of the patient. Long-term follow-up was done without any problem (20 month) [Table/Fig-4b].
Discussion
The development of an ameloblastoma or malignant transformation from the epithelial cells of the OKCs is extremely rare. In the published literature, only 7 cases of ameloblastomas which originated from the OKC’s epithelium were found except the current case. Brannon RB et al., presented 2 cases in 1977, Kakarantza-Angelopoulou E and Nicolatou O, presented 2 cases in 1990, in 2007 Ogunsalu C et al., presented 1 case in 2007, Geng N et al., presented 1 case in 2012 and Neuman AN et al., presented 1 case in 2015 [1-5].
In this case report, previously reported OKCs with ameloblastomatous transformation were investigated and reported [Table/Fig-5]. This table contains information such as author name, year of publication, sex, age, location, clinical and radiological features of lesion, treatment method and follow-up. However, lot of information in most of the cases was lacking. There was treatment and follow-up information of only two cases (Ogunsalu C et al., and Geng N et al., [3,4].
A review of previously reported cases of OKC with ameloblastomatous transformation.
| Author | Publication year | Age (years) | Sex | Location | Clinical features | Radiological features | Microscopic properties | Immunohistochemical properties | Treatment | Follow-up |
|---|
| Brannon RB, (1. case) [1] | 1977 | NS | NS | NS | NS | NS | Mural ameloblastomatous proliferation in an odontogenicKeratocyst(Patient number not specified.) | - | NS | NS |
| Brannon RB, (2. Case)[1] | 1977 | NS | NS | NS | NS | NS | - | NS | NS |
| Kakarantza-angelapoulou E and Nicolatou U, (1. case) [2] | 1990 | NS | NS | NS | NS | NS | Ameloblastoma-like epithelial islands in the fibrous capsule(Patient number not specified.) | - | NS | NS |
| Kakarantza-angelopoulou E and Nicolatou U, (2. case) [2] | 1990 | NS | NS | NS | NS | NS | - | NS | NS |
| Ogunsalu C et al., [3] | 2007 | 21 | NS | In the anterior part of the mandible | Two-month history of a painless intra-oral swelling of the right mandible and a six-month history of numb feeling of the anterior area of mandible | Well defined and moderately well corticated, extensive radiolucent lesion from the region of 45 (distal) crossing the midline to the region of #34. The lesion extends from the lower cortical bone to the apex of all the teeth in this region. The radiolucency was unilocular with no internal bony septa. Resorption of the roots of 41–44 and 31–33 was also present. | Ameloblastoma-like epithelial islands in the fibrous capsule.(patient number not specified.)In one area,However, the epithelium showed transition to ameloblasticType epithelium and there were small buds which were present in the stoma. | - | Cryosurgery with preservation of the lower cortical bone of the mandible. | The radiological follow-up for a period of six years showed no recurrence. |
| Geng N et al., [4] | 2012 | 38 | F | In the posterior part of the left maxilla | 3-year history of a painless swelling in the left maxilla | A multilocular ill-defined radiolucent lesion, approximately 4.0 × 2.5 cm. The lesion extended from the left maxillary premolar region to the tuberosity, and infiltrated into the surrounding bony trabecula | Ameloblastoma-like lining epithelium was detected in some of the cystic structures | Ck14 and ck19 positive in ameloblastomatous transformation areasCk10 and ck13 positive in OKC areasKi-67 index rate is about 8% in ameloblastomatous transformation areas and is average 20% in OKC areas | Block section from the first premolar to tuberosity of left maxillary. | No recurrence in 36 month |
| Neumann AN et al., [5] | 2015 | 17 | F | In the left molar region(exact localis ation not specified) | NS | NS | Seen in the specimenwere islands of odontogenic epithelium resembling theEnamel organ; these islands exhibited peripheral palisadingwith reverse polarity and apical vacuolisation. | - | NS | NS |
| Present case | - | 22 | M | In the angulus and ramus of left mandible | Extraoral swelling in the left ramus of the mandible for about 2 months | A large size lesion of the left mandible, containing the all of the ramus and extending the distal aspect of second molar and involving an impacted tooth | Thin parakeratinised stratified epithelium with prominent and local ameloblastic transformations were seen. | - | Marginal section from the second molar to the coronoid process of left mandible and preservation of the lower cortical bone of the mandible. | No recurrence in 20 months |
M: Male; F: Female: NS: Not state
However, they reported that cases of ameloblastomatous transformation from the odontogenic keratocyst epithelium can be associated with Nevoid Basal Cell Carcinoma Syndrome (NBCCS) and said that ameloblastoma is more prevalent in patients with NBCCS. However, there were no syndromic associations with the cases presented by Kakarantza-Angelopoulou E and Nicolatou O, Ogunsalu C et al., Geng N et al., Neuman AN et al., [2-5]. Similarly, there were no NBCC syndromes in the current case.
There was no information about the age, sex, clinical radiological and histopathological features of two cases reported by Kakarantza-Angelopoulou E and Nicolatou O, [2]. However, Ogunsalu C et al., reported an OKC case with ameloblastomatous transformation and treated this patient with cryosurgery only [3]. They stated that there was no recurrence in the 6-year follow-up period. Geng N et al., treated patient with block resection of an OKC with ameloblastomatous transformation and they observed that there was no recurrence till 3-year follow-up [4]. They performed clinical, radiological and microscopic features of their case. No follow-up data was available for case reported by Neuman AN et al., [5]. Present case is in line with the previously reported cases regarding to clinical features such as young age, posterior localisation, history of painless swelling and microscopic features.
Combined odontogenic lesions of the jaws are complex cases and they may be misdiagnosed. A precise identification of the lesion is imperative before appropriate treatment plan to be established.
Histopathological and immunohistochemical examination of the biopsy specimens plays a vital role in both correct diagnosis and prognosis. Jeyaraj P stated that immunohistochemistry can be a valuable tool especially, tumour markers such as “calretinin” specific to ameloblastomatous cells that serves as a diagnostic marker and is used to distinguish between odontogenic tumour and cysts [6]. He also used immunohistochemical cell proliferation markers to determine the treatment modality in their cases and decided to surgical method according to the ratio of these markers. In addition, ıt is suggested that proliferation markers such as Ki-67 and PCNA (proliferating cell nuclear antigen) can also be used as a prognostic indicator in terms of the clinical prognosis, aggressive potential and biological behaviour [7,8]. Unfortunately, immunohistochemistry was not done in the current case.
OKC (especially solid variant of OKC) may be confused with Keratoameloblastoma (KA) because they contain keratinisation. KA is extremely rare variants of ameloblastoma. It has histological features such as solid tumour islands, keratinisation sites, peripheral palisading, reversed polarisation of nuclei and subnuclear vacuolisation [9]. To diagnose the lesion as a KA, all regions of the lesion must have these histologic properties. However, in the presented case, cyst was lined by thin stratified squamous epithelium with superficial corrugated parakeratosis and palisaded basal cell layer, resembling the OKC. In addition, in some areas of the cyst wall, reversed polarisation of nuclei, tall columnar cells with palisaded nuclei and overlying stellate reticulum-like cells are seen. These histologic properties belong to ameloblastoma. Combining the features of two different lesions proves that the lesion is a hybrid lesion.
Geng N et al., emphasised that the hybrid cases with different pathologic diagnoses may represent the possible transformation of the odontogenic epithelium during tumourigenesis [4]. They considered that their case fell within the broad histopathologic spectrum between solid variant of OKC and KA. Similarly, in the presented case, histologically the main part of the lesion showed OKC architecture and only some areas demonstrated ameloblastomatous features. Considering treatment planning, block resection is the best surgical method to completely eliminate this hybrid lesion. As the treatment plan is usually based on more aggressive of the involved lesions, the current case was treated with marginal resection to preserve mandibular continuity and inferior alveolar nerve and reconstructed with anterior iliac crest graft.
Conclusion(s)
The current case report was of a hybrid lesion of Odontogenic keratocyst with Ameloblastomatous transformation, successfully treated by marginal resection and reconstruction with anterior iliac crest graft with no recurrence during the 20 months follow-up period. However, due to the rarity and lack of the data of the reported cases the prognosis and best treatment option of these cases is unknown. The increased number of reported cases will provide a better understanding of combined or hybrid lesions.
M: Male; F: Female: NS: Not state
[1]. Brannon RB, The odontogenic keratocyst. A clinicopathologic study of 312 cases. Part II. Histologic featuresOral Surg Oral Med Oral Pathol 1977 43(2):233-55.10.1016/0030-4220(77)90161-X [Google Scholar] [CrossRef]
[2]. Kakarantza-Angelopoulou E, Nicolatou O, Odontogenic keratocysts: Clinicopathologic study of 87 casesJ Oral Maxillofac Surg 1990 48:593-99.10.1016/S0278-2391(10)80472-0 [Google Scholar] [CrossRef]
[3]. Ogunsalu C, Daisley H, Kamta A, Kanhai D, Mankee M, Maharaj A, Odontogenic keratocyst in Jamaica: A review of five new cases and five instances of recurrence together with comparative analyses of four treatment modalitiesWest Indian Med J 2007 56(1):86-89.10.1590/S0043-3144200700010001717621852 [Google Scholar] [CrossRef] [PubMed]
[4]. Geng N, Lv D, Chen QM, Zhu ZY, Wu RQ, He ZX, Solid variant of keratocystic odontogenic tumour with ameloblastomatous transformation: A case report and review of the literatureOral Surg Oral Med Oral Pathol Oral Radiol 2012 114(2):223-29.10.1016/j.oooo.2011.11.02322769408 [Google Scholar] [CrossRef] [PubMed]
[5]. Neuman AN, Montague L, Cohen D, Islam N, Bhattacharyya I, Report of two cases of combined odontogenic tumours: Ameloblastoma with odontogenic keratocyst and ameloblastic fibroma with calcifying odontogenic cystHead Neck Pathol 2015 9(3):417-20.10.1007/s12105-014-0601-125552434 [Google Scholar] [CrossRef] [PubMed]
[6]. Jeyaraj P, The dilemma of extensive unilocular radiolucent lesions of the jaws-value of immunohistochemistry as a diagnostic marker and prognostic IndicatorAnnals of diagnostic pathology 2019 40:105-35.10.1016/j.anndiagpath.2019.04.00731077874 [Google Scholar] [CrossRef] [PubMed]
[7]. Coleman H, Altini M, Ali H, Doglioni C, Favia G, Maiorano E, Use of calretinin in the differential diagnosis of unicystic ameloblastomasHistopathology 2001 38(4):312-17.10.1046/j.1365-2559.2001.01100.x11318896 [Google Scholar] [CrossRef] [PubMed]
[8]. Meer S, Galpin JS, Altini M, Coleman H, Ali H, Proliferating cell nuclear antigen and Ki67 immunoreactivity in ameloblastomasOral Surg Oral Med Oral Pathol Oral Radiol Endod 2003 95(2):213-21.10.1067/moe.2003.6212582363 [Google Scholar] [CrossRef] [PubMed]
[9]. Ide F, Mishima K, Saito I, Solid-cystic tumour variant of odontogenic keratocyst: An aggressive but benign lesion simulating keratoameloblastomaVirchows Archiv 2003 442(5):501-03.10.1007/s00428-003-0764-812687356 [Google Scholar] [CrossRef] [PubMed]