The Traumatic Optic Neuropathy (TON) is a rare but devastating cause of partial or complete visual loss caused by deformational forces that injure the optic nerve [1]. Optic nerve injuries can be broadly classified as direct and indirect injuries. Direct anatomical disruption of the optic nerve constitutes direct injury [2]. Indirect injury develops from concussive forces where optic nerve absorbs energy concentrated at the orbital apex. Indirect TON occurs in absence of an open wound but with a positive history of blunt trauma.
Management of TON is controversial. Many studies have been conducted to find a definite and standard protocol for treatment and rehabilitation of visually deprived patients in TON [3]. Steroids are the magical drug that came into effect since late 1980s. It brought about dramatic changes in the inflammatory process and has been proved to have neuroprotective as well as neuro-regenerative properties. The National Acute Spinal Cord Injury Study II (NASCIS II) conducted in 1990 added further evidence to the beneficial effect of steroids in acute spinal cord injury [4]. This encouraged many ophthalmologists to actively intervene in TON patients.
OCT has become an ancillary tests in ophthalmology used for in vivo visualisation of biological tissues in human eyes. By OCT examination, multiple thin slices, laminar sheet structural images of morphologic changes of retina including RNFL thickening or thinning, can easily be detected [5]. OCT, Optic Nerve Head (ONH) and RNFL is of prime role in patients with TON. It helps in documenting the progression of damage [6].
This study was an attempt to identify TON patients at the earliest, after appropriate examination and start treatment with IV steroids in indirect TON patients as early as possible to save their vision. OCT ONH is being used as a follow-up tool to evaluate progression and regression of axonal loss.
Materials and Methods
This observational prospective study was conducted in the Department of Ophthalmology, Emergency Medicine and Neurosurgery, in a tertiary care centre of India, for a period of one year (January 2018 to January 2019) included 29 patients Ethical Committee clearance was taken with ref no. 60/17/IEC/JMMC & RI.
Inclusion Criteria: All patients who present with head trauma or ocular trauma and diagnosed with TON (defective vision and relative afferent pupillary defect) after ocular examination were included.
Exclusion Criteria: Patients who were unconscious and presented with non reactive pupil of both eye; Patients who were discontinued on IV, steroids due to contraindication or intolerance. Patients who were not regular on follow-up. Patients who were not willing to sign the consent form to take part in research.
Methods of Data Collection
Detailed history and complete ophthalmological evaluation were done. CT Brain is done routinely for patients with head trauma to rule out any intracranial pathology of vision loss. Dilated fundus evaluation, Intraocular Pressure (IOP) measurement, colour vision, OCT (ONH) studies was performed before the end of hospital stay. OCT using Cirrus HD-OCT (Carl Zeiss Meditec, Dublin, CA) in undilated pupil and under the same intensity of dim room lighting- by the same specialist was done to analyse the peripapillary RNFL thickness measured as mean thickness in superior, inferior, nasal and temporal quadrants.
Follow-up was done after one week of discharge, then after one month. OCT was performed after one week of discharge and one month thereafter. Patients who were diagnosed as TON were counselled and explained about the prognosis of the his/her visual recovery and taken an informed consent.
Sample size were calculated based on prevalence of improvement of visual acuity in an earlier publication by Sundeep H et al., (prevalence of 93.4%) with 95% confidence level and 15% relative allowable error minimum sample size of my study comes to 22 [7].
Statistical Analysis
Data obtained were coded and entered into Microsoft Excel sheet and analysed using IBM SPSS version 25. The paired t-test/Wilcoxon sign rank test was applied to test the mean differences of study variables from one week to one month.
Results
Data was collected from 29 patients who satisfied the inclusion criteria was taken into the study.
1. Gender/Age-wise Distribution of Patients
All samples in the study were males. The [Table/Fig-1] shows mean age in study population was 27.90±5.14 years. Maximum number of patients was in the age group of 30-33 years (8 patients). Minimum age was 20 years. Maximum age was 40 years.
Age-wise distribution of TON patients.

2. Frequency of Different Visual Acuities in Assessment Times
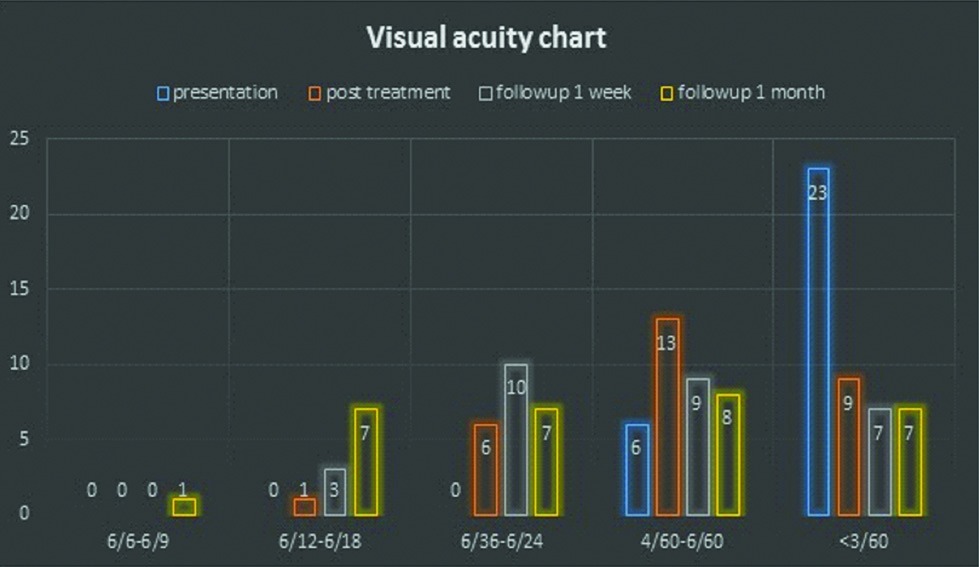
Maximum number of patients presented with a baseline visual acuity of <3/60 that accounted to 23. Remaining six had a baseline visual acuity of 4/60-6/60. Significant difference in visual acuity was seen only in 6/36-6/24 range [Table/Fig-2]. And only one patient improved to 6/9 post treatment after a month.
Frequency of different visual acuities in assessment times.
3. Percentage of Patients with Two Line Improvement in Visual Acuity according to Baseline Visual Acuity
Ten patients presented with No Perception of Light (NPL), PL, HM at the time of presentation [Table/Fig-3]. Only six patients out of these had ≥2 line improvements at the end of one month, while 19 patients with CF or better at the time of presentation, 18 patients had ≥2 line improvement after one month follow-up. Hence, initial visual acuity acts as a prognostic factor in the visual recovery of TON patient.
Percentage of patients with 2 line improvement in visual acuity according to baseline visual acuity.
NPL: No perception of light; PL: Perception of light; HM: Hand movements; CF: Counting fingers

4. Associated Risk Factors that Succumb Vision in TON Patients
Rosette cataract was noted in 17.2%, while fractures due to trauma also hindered visual assessment and recovery and accounted to 34.4%, and refractive error was present in 13.7% [Table/Fig-4].
Associated risk factors that succumb vision in TON patients.
| Associated factor | Frequency | Percentage% |
|---|
| Rosette cataract | 5 | 17.2 |
| Fractures | 10 | 34.4 |
| Refractive error | 4 | 13.7 |
5. IOP Comparison Pre-Treatment and Post-Treatment
IOP baseline mean was calculated as 16.24 and standard deviation of 2.56. IOP on follow-up after one month mean was calculated as 16.45 and standard deviation of 2.22 with a p-value of 0.74 (not significant).
6. RNFL Thickness Comparison in all Four Quadrants
OCT RNFL thickness of baseline and on follow-up in nasal, temporal, and inferior quadrants showed a significant p-value [Table/Fig-5].
RNFL thickness comparison in all four quadrants.
| OCT RNFL | Pre-treatment mean | Post-treatment mean | Pre-treatment SD | Post-treatment SD | p-value |
|---|
| Superior | 109.1 | 112.4 | 8.09 | 5.81 | 0.05 |
| Nasal | 49.2 | 51.6 | 7.3 | 6.7 | 0.03 |
| Inferior | 110.90 | 113.4 | 7.08 | 6.7 | 0.04 |
| Temporal | 57.2 | 54 | 8.2 | 8.8 | 0.007 |
7. Average RNFL Thickness Map
The average RNFL thickness one week and one month injury was calculated with a p-value of 0.001 which is significant [Table/Fig-6].
Average RNFL thickness map.
| OCT average RNFL thickness | Mean | SD | p-value |
|---|
| 1 week | 68.62 | 11.83 | 0.001 |
| 1 month | 75.07 | 15.15 |
Discussion
The TON refers to optic nerve injury resulting from direct and indirect head and facial trauma [1]. It is rare and often missed to diagnose in cases of polytrauma and altered mental status of the patient. Only 0.5 to 2% of head injuries are associated with optic nerve injury.
The present study was conducted in a tertiary care centre with well-established emergency services, hence all trauma patients undergo complete examination and none of the patients were missed. Present study was done to evaluate and promptly diagnose every TON patient without any undo delay and to administer steroids in indirect TON after neurosurgical clearance. We also monitored the patient during the hospital stay and performed OCT to evaluate ONH-RNFL and found that there was significant reduction in circumpapillary nerve fibre layer but with IV steroids the progression of axonal loss was stabilised.
This study showed majority of the patients were within age group of 30-33 years. This findings were similar to Pirouzmand F study and a UK based study by Lee V et al., [8,9]. In study by Pirouzmand F the median age group was 33.5 years [8]. While in the study by Lee V et al., the median age was 31 years [9], that in the study by Sundeep H et al., it was 39.1 years, which was more than the index study [7].
Most common cause of TON was road traffic accidents with head injury (92%), similar to the study by Levin LA et al., [10]. While in the study by Lee V et al., the leading causes of TON included falls (25.6%), road traffic accidents (21.5%), and assaults (20.7%) [9].
In this study the risk factors associated for outcome in indirect TON included adjacent facial bone fractures, refractive error, rosette cataract and severe head injury. Adjacent facial bone fractures causes periorbital edema and ecchymosis which makes it difficult to assess pupil and vision in these patients. Similarly severe head injury hinders visual acuity assessment due to altered conscious level. Rosette cataract developed in three patients after 5-7 days of injury.
IOP on follow-up after one month mean was calculated as 16.45±2.22 mm Hg. The IOP values were not significant before and after treatment with steroids. This was comparable to the study by Ropposch T et al., on indirect TON [11]. A total of 34.5% of patients presented with poor initial visual acuity of NPL, PL, HM and 51.7% presented CF or better vision. But following treatment with steroids 82.6% patients achieved ≥2 line improvement in visual acuity.
The National Acute Spinal Cord Injury Study 2 brought about the concept of i.v., steroids in treatment of TON. This multicenter clinical trial evaluated the role of placebo, methylprednisolone, or naloxone in patients with acute brain and spinal cord injury [12]. The results showed that methylprednisolone (30 mg/kg loading dose, followed by 5.4 mg/kg/h for 24 h) started within 8 h of injury resulted in a significant improvement in neurological outcome compared with placebo.
While in this study, the dosage of IV, methylprednisolone was 1 g IV bolus dose followed by 500 mg twice a daily dose for 3 days. It was shifted to oral steroids and dose tapered for 4-6 days. A visual recovery rate of 40-60% has been reported for indirect TON cases when managed conservatively with IV steroids. The baseline visual acuity was the most important predictor of final outcome. Patients with initial visual acuity of NPL had limited or no visual improvement [13-15].
In this study most of the patients were given a similar dose of IV steroids within 24 hours to injury after neurosurgical clearance. But concomitant brain injury especially in large subdural haemorrhage may have poorer neurological benefit with megadose of steroids [16].
RNFL analysis using OCT showed significant reduction mainly on the nasal side and in superior side after two weeks of trauma. But on subsequent follow-up of one month, the RNFL thickness in all patients had improved but did not reach the normal. Kanamori A et al., found that the reductions in circumpapillary RNFL and RGC complex in TON patients began to decrease at two weeks after trauma and plateaued at 20 weeks in all cases [17]. Cunha LP et al., also compared circumpapillary RNFL loss and macular thinning in three patients with TON using stratus OCT. They showed progressive reduction of macular as well as peripapillary RNFL average thickness measurements after TON documented sequentially by OCT [18]. Similar studies were done by Medeiros FA et al., and Miyahara T et al., which also proves OCT is a helpful tool in TON [Table/Fig-7] [6,19].
Showing OCT RNFL of a TON patient done at first week and four weeks following treatment with intravenous steroids, patient’s visual acuity was 6/60, initially. Nasal and temporal RNFL quadrants are reduced initially, but improved after weeks. Average RNFL thickness is within normal limits when right eye of same patient is taken as a control.

Limitation(s)
The sample size was small. Vision could not be converted into log MAR charts as counting fingers were not represented in these charts.
Conclusion(s)
The use of IV steroids can help in visual recovery in patients with indirect TON. As most of the patients are young and loose their vision to a great extent IV, steroids can be considered in the reduction of associated inflammation in the optic canal. But meticulous evaluation and monitoring of the patients during the course of IV steroids is also crucial. The baseline visual acuity of the patient is a prognostic factor for the visual recovery. The timing of start of the therapy within 24 hours of injury before a full-fledged inflammation sets in is another prognostic factor. OCT RNFL is helpful in assessing the nerve fiber layer which is gravely affected in TON, hence can be recommended as a follow-up tool for these patients. A definite diagnosis and neurosurgical monitoring is also recommended.